Fig. 3.1
Normal peristalsis in HRM with EPT plots. The esophageal contraction is characterized by three troughs and the contractile deceleration point (CDP, black dot). EGJ relaxation is assessed using the IRP measured within the white boxes. The DL is measured from UES relaxation to the CDP. The CFV is measured as the tangent to the contractile wavefront at 30-mmHg isobaric contour. The DCI corresponds to the “volume” of the contraction above 20 mmHg between the proximal trough and the EGJ (contractile volume included in the dashed yellow box) measured in units of mmHg-s-cm
The Chicago Classification is an algorithmic scheme for the diagnosis of esophageal motility disorders from HRM studies in terms of EPT [4]. Consequent from their vetting through a consensus process, the Chicago Classification definitions of esophageal motility disorders are widely accepted. An important caveat to this is that only primary esophageal motility disorders are addressed in the Chicago Classification. It was not intended for application to postsurgical studies such as fundoplication, Heller myotomy, or bariatric surgery. Similarly, the characterization of EGJ pressure morphology and UES function is not addressed in the Chicago Classification. The intent of this review is to summarize the current version of the Chicago Classification. The overall scheme of the analysis is to first systematically analyze the ten test swallows and to then apply an algorithm to classify motility disorders.
Swallow Analysis
The metrics, normal values, and analysis for the Chicago Classification are based on a series of ten 5-ml water swallows conducted in a supine posture. Individual test swallows are first scored utilizing EPT-specific metrics that evaluate EGJ relaxation, characterize the esophageal contraction, and characterize bolus pressurization.
Evaluation of EGJ
In absence of hiatal hernia, pressure signals resulting from the lower esophageal sphincter (LES) and crural diaphragm (CD) are not distinguishable. As a consequence the term “EGJ relaxation” is used. Moreover, during swallowing, the pressure measured at the level of the EGJ is the composite of LES pressure, CD contraction, and intrabolus pressure as the swallowed bolus traverses the EGJ. Finally, the LES elevates during swallowing due to esophageal longitudinal muscle contraction. Hence, accurate identification of the axial limits of the EGJ is essential to avoid the artifact of pseudo-relaxation created when the sphincter elevates above the zone of measurement.
The EPT metric which best discriminated normal EGJ relaxation from impaired EGJ relaxation is the integrated relaxation pressure (IRP) [5]. The IRP is derived from an e-sleeve measurement applied at the level of the EGJ within a 10-s window beginning with deglutitive UES relaxation. The IRP is the mean pressure for the 4 s (continuous or noncontinuous) during which the e-sleeve value is least within this window. It is influenced not only by LES relaxation but also by CD contraction and intrabolus pressure. By convention, the IRP is referenced to intragastric pressure. Using the Given adult version circumferential HRM sensing device (Given Imaging, Los Angeles, CA), the upper limit of normal for the IRP is a mean of 15 mmHg for ten swallows in the supine posture. Appropriate normal values for other devices and postures need to be established.
Although the Chicago Classification was not intended to describe EGJ pressure morphology or barrier function, this has been characterized to some degree with EPT. The EGJ can be classified into three subtypes based on the axial relationship between the LES and the CD [6]. With EGJ type I, the LES and CD are superimposed. With EGJ type II there is a minimal separation between LES and CD (1–2 cm). Finally, EGJ type III is characterized by a separation >2 cm at inspiration between the LES and CD. Type III is the HRM signature of hiatal hernia. In a logistic regression analysis, the magnitude of inspiratory augmentation of EGJ pressure was found to be the only manometric variable independently associated with GERD [6]. Patients with esophagitis or increased esophageal acid exposure on ambulatory pH monitoring had significantly less inspiratory EGJ augmentation when compared to asymptomatic controls or patients with negative pH monitoring studies.
EPT Metrics to Assess the Deglutitive Esophageal Contraction
The architecture of the post-deglutitive esophageal contraction is characterized by 2–3 pressure troughs (proximal, distal, and sometimes one in the middle) [7] and a contractile deceleration point (CDP) [8] (Fig. 3.1). The proximal trough is also called the “transition zone.” The CDP is an inflection point in the contractile wavefront velocity corresponding to the transition from the peristaltic propagation to the late phase of esophageal emptying, which proceeds much slower than the peristaltic propagation. Thus the contractile front velocity (CFV) is measured from the proximal pressure trough to the CDP as the slope of the tangent to the 30-mmHg isobaric contour of the contractile wavefront. However, a more important indicator of the integrity of the inhibitory pathway in the distal esophagus is the contraction latency at the CDP. Hence, the distal latency (DL), measured from UES relaxation to the CDP, is used in the Chicago Classification to define premature esophageal contractions, indicative of spasm [9] (Fig. 3.2).
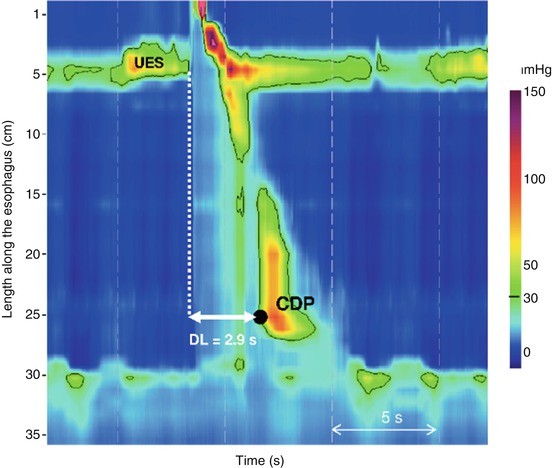
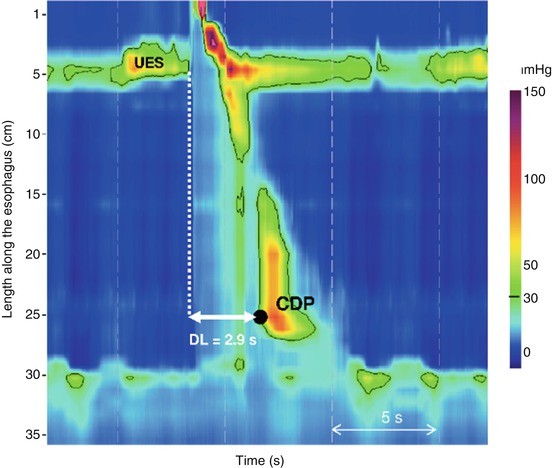
Fig. 3.2
The DL is used to evaluate the integrity of deglutitive inhibition that precedes the distal esophageal contraction. It measured from the beginning of UES relaxation to the CDP (black dot). In this example, the DL is <4.5 s defining a premature contraction. In instances of normal EGJ relaxation (IRP = 9 mmHg in this example), ≥20 % premature contractions define distal esophageal spasm
The metric developed to describe the vigor of the distal esophageal contraction in the Chicago Classification is the distal contractile integral (DCI) [10]. It is measured as the “volume” of the esophageal contraction spanning from the proximal pressure trough to the EGJ. The DCI is the product of the integral of the amplitude (greater than 20 mmHg), the duration, and the length of the contractile segment between the proximal trough and the EGJ (Fig. 3.1). The upper limit of normal (95th percentile) is 5,000 mmHg-s-cm and a value greater than 8,000 mmHg-s-cm was never encountered in a normal population. Lower limits for the DCI were also recently defined: a DCI <150 mmHg-s-cm identifies failed peristalsis and a DCI <450 mmHg-s-cm defines weak peristalsis [11].
Scoring Individual Swallows
Each swallow is characterized for the integrity of the contraction, contraction pattern, and intrabolus pressure pattern (Table 3.1). Contraction integrity should first be assessed based on the integrity of the 20-mmHg isobaric contour. Interruptions, or breaks, in the 20-mmHg isobaric contour between the UES and the EGJ are characterized by their axial length; breaks 2 cm or longer are considered significant based on correlation with impaired bolus transit [12]. Large breaks are >5 cm in length and small breaks are 2–5 cm. Contractions with small or large breaks are defined as weak contractions.
Table 3.1
Esophageal pressure topography scoring of individual swallows
Integrity of contraction | |
Intact contraction | 20-mmHg isobaric contour without large or small break |
Weak contraction | (a) Large break in the 20-mmHg isobaric contour (>5 cm in length) |
(b) Small break in the 20-mmHg isobaric contour (2–5 cm in length) or DCI <450 mmHg-s-cm | |
Failed peristalsis | Minimal (<3 cm) integrity of the 20-mmHg isobaric contour distal to the proximal pressure trough (P) |
Or DCI <150 mmHg-s-cm | |
Contraction pattern (For intact or weak contractions with small breaks) | |
Premature contraction | DL <4.5 s |
Hypercontractile | DCI >8,000 mmHg-s-cm |
Rapid contraction | CFV >9 cm/s |
Normal contraction | Not achieving any of the above diagnostic criteria |
Intrabolus pressure pattern (30–mmHg isobaric contour) | |
Panesophageal pressurization | Uniform pressurization extending from the UES to the EGJ |
Compartmentalized esophageal pressurization | Pressurization extending from the contractile front to a sphincter |
EGJ pressurization | Pressurization restricted to zone between the LES and CD in conjunction with hiatal hernia |
Normal pressurization | No bolus pressurization >30 mmHg |
Intact contractions and weak contractions with small breaks are further characterized by DL, DCI, and CFV. These metrics are used to define premature contractions (DL <4.5 s; Fig. 3.2), hypercontractility (DCI >8,000 mmHg-s-cm; Fig. 3.3), and rapid contraction (CFV >9 cm/s), summarized in Table 3.1. Finally, each swallow is characterized according to the associated pattern of intrabolus pressure, assessed with the 30-mmHg isobaric contour. Intrabolus pressure is qualified as panesophageal pressurization if it spans from UES to EGJ, as compartmentalized pressurization when it is restricted to the segment between the esophageal contraction and one sphincter, or normal when there is no bolus pressurization to greater than 30 mmHg. Panesophageal pressurization can be distinguished from a simultaneous contraction by analyzing the corresponding spatial pressure variation plot. In instance of panesophageal pressurization, the spatial pressure variation plot between sphincters is flat, without regional variation. On the other hand, in instances of simultaneous esophageal contractions, pressure variations are visualized along the esophageal body (Fig. 3.4).
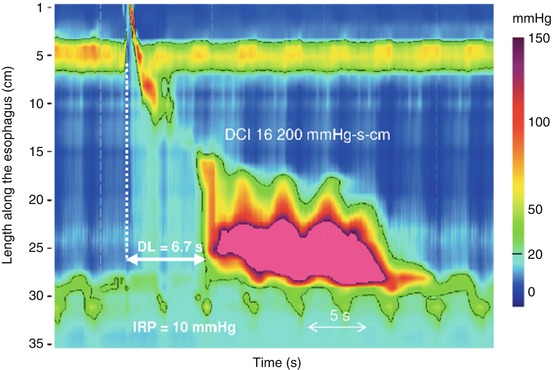
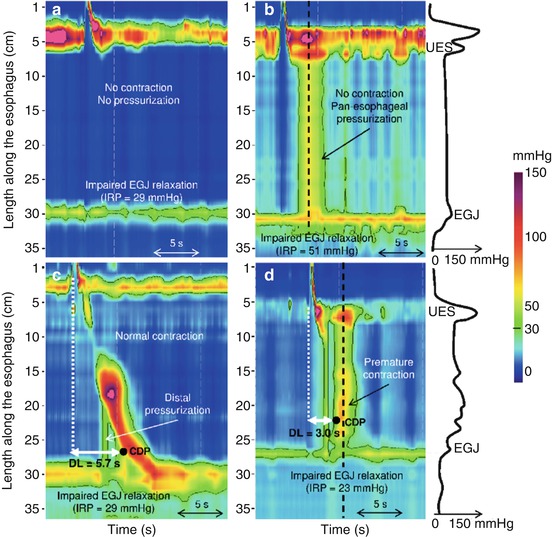
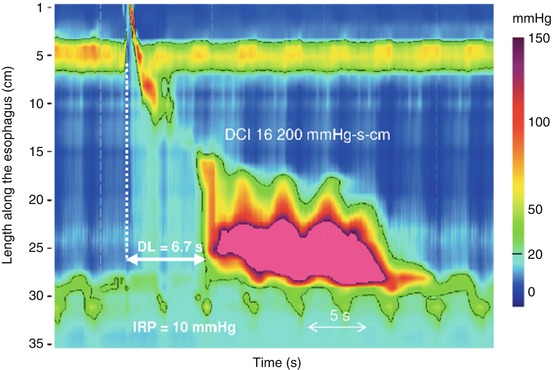
Fig. 3.3
Jackhammer esophagus is defined by a study exhibiting at least one contraction with a DCI >8,000 mmHg-s-cm. Note that esophageal contraction is repetitive in this example. The DL and the IRP are normal
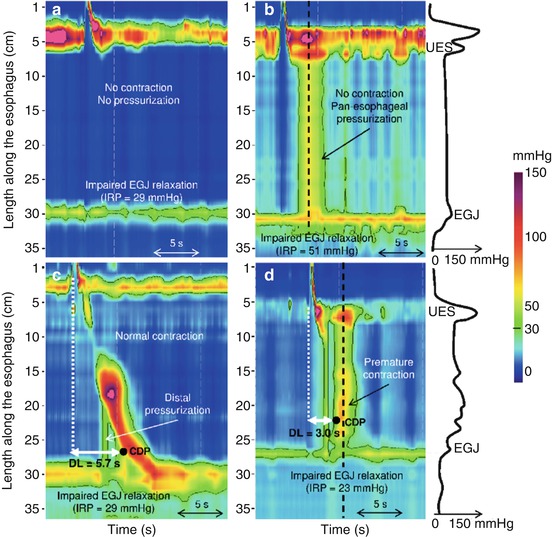
Fig. 3.4
Achalasia subtypes and EGJ outflow obstruction. EGJ relaxation is assessed using the IRP and is >15 mmHg in all of these examples. Type I (panel a) and type II achalasia (panel b) are characterized by absent contractions. In type II, panesophageal pressurization is a pathognomonic finding. Esophageal contractions can be normal, weak, hypertensive, or rapid in EGJ outflow obstruction (panel c), whereas they are premature in type III achalasia (panel d). Panesophageal pressurization (panel b) can be differentiated from simultaneous contraction (panel d) using the spatial pressure variation plot illustrated on the right, corresponding to the pressure profile within the esophagus at the time of the black dashed line. In instances of panesophageal pressurization (panel b), intraesophageal pressure did not vary between the UES and EGJ. In instance of a spastic contraction (panel d), pressure variations are obvious along the esophageal body
Esophageal Motility Disorders
The summary analysis of the ten test swallows is utilized to fit the study to Chicago Classification criteria [4]. The classification prioritizes esophageal motility disorders in a hierarchical fashion: (1) achalasia and motility disorders never observed in normal subjects and (2) peristaltic abnormalities that are out of the range of normal values (95th percentile confidence intervals for a set of normal control subjects). Chicago Classification diagnoses are summarized in Table 3.2.
Table 3.2




Esophageal motility disorders
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


