Michael A. Bettmann
The Chest Radiograph in Cardiovascular Disease
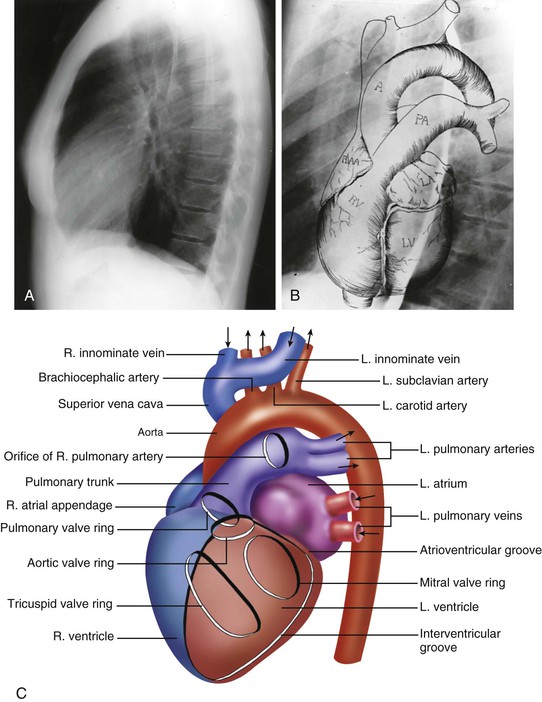
The chest x-ray (CXR) remains the most common radiographic examination and one of the most difficult to interpret. With careful evaluation, it yields a large amount of anatomic and physiologic information, but it is difficult and sometimes even impossible to extract all the information that it contains. The aims of this chapter are to review how the CXR is obtained, present a basic approach to its interpretation, and discuss and illustrate common and characteristic CXR findings in adults with cardiovascular disease. The major variables that determine what can be learned from the CXR include (1) the technical factors (milliamperage, kilovoltage, exposure duration) used in obtaining the CXR; (2) patient-specific factors (e.g., body habitus, age, physiologic status, ability to stand and to take and hold a deep breath); and (3) the training, experience, and focus of the interpreter.
Image Recording and Radiation Exposure
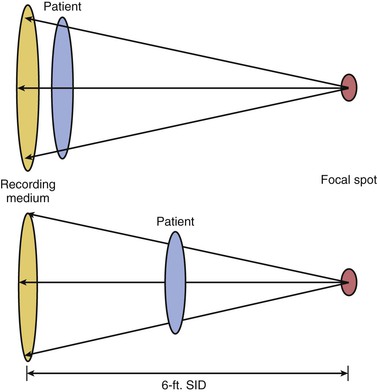
Until the turn of the last century, all CXRs were recorded on high-resolution radiographic film. With optimal technique and a cooperative patient who can hold a deep inspiration, the result is a study that clearly and accurately depicts very small structures, such as the contour of small pulmonary arteries. With radiographic film, the incident x-rays (and scattered photons) alter the silver iodide crystals in an emulsion. When the film is developed, these alterations produce an image reflecting the extent to which the x-rays have interacted with specific areas of the film. There is inherently very high resolution of structures because of the small size of the silver iodide crystals and their sensitivity to incident x-ray photons. This has changed with the use of computed radiography (CR) and digital radiography (DR), filmless forms of radiography. DR is the direct recording of images by digital means, without analog-to-digital conversion, onto a panel that allows direct recording of incident photons of different energy and frequency on a flat digital panel, without the use of a permanent film or analog-to-digital conversion. This information is then directly downloaded and can be viewed and postprocessed. CR is similar, but instead of a direct connection to the radiology information system (RIS), the image is recorded onto a reusable panel, which is then “read” into the system and downloaded. Currently, CR is less expensive, and because it does not inherently require direct connection to the RIS, it is widely used for portable imaging. As the cost of flat panels for DR decreases and the ability to download images wirelessly improves, CR is gradually being replaced. The inherent resolution with both is very similar to that of conventional radiographic film, but the elimination of analog-to-digital conversion eliminates some noise and thus the overall resolution tends to be as good as with conventional film-screen radiographs.5–16 DR has additional advantages. First, digital technology leads to an image that is posted immediately on the RIS, without going through the step of developing the film. Using picture archiving and communication systems (PACS), digital images are then available as soon as they are downloaded for review at any location where a PACS-enabled workstation is present. This adds speed and availability and obviates the problem of lost films—all films are digitally archived—and the need to go to a remote location to review a film.17,18 The dose to an individual patient may or may not be lower as a function of patient factors and the specific imaging system.8,15,17 Overall radiation exposure to patients, however, is decreased because the need to repeat films as a result of inadequate positioning or exposure is substantially eliminated: with DR, the image can be postprocessed to alter the relative density (window and level), and magnification and even the area included can be altered without re-exposing the patient. This provides the ability to add substantial information (Fig. e15-2![]() ). Storage of conventional radiographic films is relatively straightforward, although it is time and space intensive. Storage of digital images, even though initially more complex, eliminates many of the major problems encountered with storage of standard radiographs. Integration with a system-wide electronic medical record allows improved access and use in comparison to what was available even a decade ago.17,18
). Storage of conventional radiographic films is relatively straightforward, although it is time and space intensive. Storage of digital images, even though initially more complex, eliminates many of the major problems encountered with storage of standard radiographs. Integration with a system-wide electronic medical record allows improved access and use in comparison to what was available even a decade ago.17,18
The radiation exposure to the patient should always be kept in mind when any radiographic study is ordered or performed. The complexity of diagnostic radiation in the general population limits obtaining clear answers. The radiation necessary for PA and lateral CXRs is usually minimal in terms of radiation effects, in both the dose of a single study (generally <1 mSv) and the cumulative dose of repeated CXRs. In pregnant women and children, radiation exposure is always a concern because of the long latency period for radiation-induced cancer.19–21 Concerns have been raised that exposure of the population has increased over the last few decades, largely because of the use of high-tech imaging such as computed tomography (CT), radionuclide studies, and cardiac interventional procedures. The contribution from conventional imaging procedures such as CXRs is small, but the precise relationships between individual exposures and cumulative effect are not known. Basically, all diagnostic imaging carries at least a small theoretical risk, even at very low doses, so any use must balance this possible risk against the probable benefit; each CXR should be ordered with care.2,3,20