, Jason L. Quill2 , Alexander J. Hill3, 4 and Paul A. Iaizzo5
(1)
Departments of Surgery and Biomedical Engineering, University of Minnesota, 420 Delaware St. SE, MMC 195, Minneapolis, MN 55455, USA
(2)
Medtronic, Inc., 8200 Coral Sea St. NE, Mounds View, Minneapolis, MN 55112, USA
(3)
Cardiovascular, Medtronic, Inc., 8200 Coral Sea St. NE, Mounds View, Minneapolis, MN 55112, USA
(4)
Department of Surgery, University of Minnesota, 420 Delaware St. SE, MMC 195, Minneapolis, MN 55455, USA
(5)
Department of Surgery, Institute for Engineering in Medicine, Lillehei Heart Institute, University of Minnesota, 420 Delaware St. SE, MMC 195, Minneapolis, MN 55455, USA
Abstract
The semilunar valves determine the passage of blood between the ventricles and the main arteries, transporting blood away from the heart to the vital organs. In a healthy individual these valves are defined by three leaflets attached in a semilunar fashion within a supporting sinus making up an arterial root positioned between their respective outflow tracts and arterial trunks. During systole, when the ventricles are contracting, the semilunar valve leaflets open to allow blood to flow to the body, i.e., ventricular ejection. As the myocardium starts to relax, prior to ventricular end diastole, the pressure within the right and left ventricles drops below the pressures in the arterial system causing the valves to snap shut. This chapter covers the histological, structural, and functional features of both the aortic and pulmonic semilunar valves and discusses the use of echocardiography to image the structures. A detailed understanding of the semilunar valve anatomy provides the foundation of knowledge critical to physicians and engineers developing future clinical therapies for the treatment of congenital and degenerative diseases.
2.1 Introduction
2.1.1 Historical Perspective
In the past century, with the advent of high resolution noninvasive imaging, our understanding of the functional internal anatomy of the body has rapidly progressed. New insights greatly extend beyond the classic work of anatomists such as Galen, Vesalius, Leonardo da Vinci, and more recently Hunter, Gray, and Netter. For a more in-depth description of progress in the understanding of the anatomy and morphology of the cardiac valves, the reader is referred to Chap. 1.
2.1.2 Attitudinally Correct Cardiac Anatomy
As mentioned previously in Chap. 1, the published descriptions of human cardiac anatomy have not adhered to the same fundamental rules of orientation and/or anatomical position as overall gross anatomy. Briefly, the three planes of the body, sagittal, coronal, and transverse (Fig. 2.1), are used to describe the position and nature of almost all other aspects of internal anatomy with respect to the patient’s own orientation. Only recently have cardiac anatomy specialists turned away from the traditional labeling of the human heart as though explanted from the body, to now redefine the nomenclature as though the heart was situated within the body (i.e., describe the cardiac anatomical features relative to the body’s anatomical planes) [1].
The naming of the cardiac semilunar valves, as seen in Fig. 2.2, has not been directly affected by attitudinally correct nomenclature due to the leaflets of each valve being described by their surrounding anatomies, rather than their position within the heart. For example, the three leaflets of the aortic valve are traditionally named after the coronary arteries that branch from the sinus of Valsalva supplying blood to the left and the right sides of the heart—the left, right, and non-coronary leaflets (Fig. 2.2). More recently due to repeated reports of coronary arteries arising from the posterior sinus, the non-coronary leaflet is referred to as the nonadjacent. Further, due to its oblique positioning in the body, the pulmonary valve leaflets are not named according to the sagittal, coronal, and axial planes, but have rather been described by their relationships to the aortic valve [2]. In a normal anatomical orientation, the right and left coronary cusps of the aortic valve face the septum between the right and left chambers. These leaflets are usually opposed by two leaflets of the pulmonary valve, hence these two leaflets of the pulmonary valve are labeled the “right and left facing leaflets.” The third leaflet of the pulmonary valve is consequently labeled the nonfacing leaflet to complete the trifecta. The specific anatomies of each semilunar valve will be described in more detail later in this chapter.
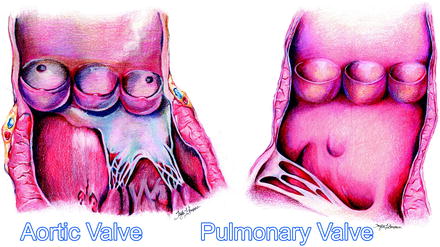
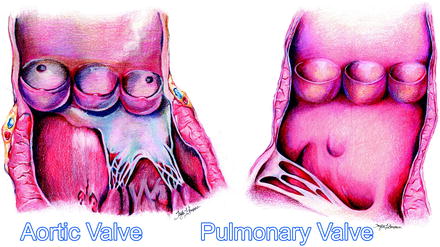
Fig. 2.2
An artist’s rendition of the healthy aortic and pulmonary valves clearly showing the leaflets, sinuses, outflow tracts, and arterial trunks
2.2 The Cardiac Skeleton
The cardiac valves are situated in close proximity to each other, shown in Fig. 2.3, and as with the atrioventricular valves, it is important to carefully describe the anatomical framework that holds these valves in position [2].
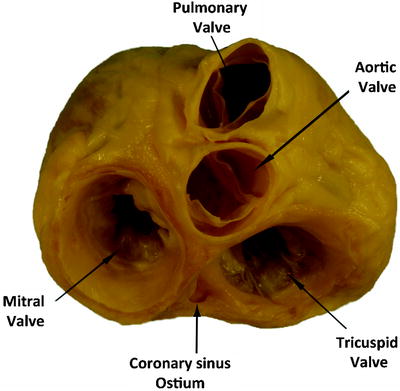
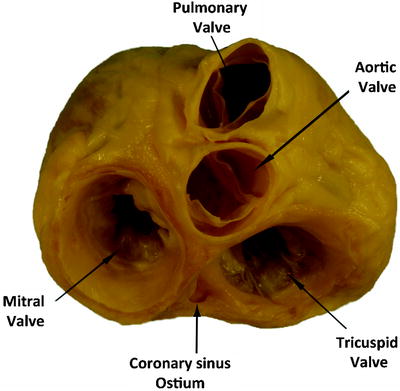
Fig. 2.3
An anatomical plate of a human heart with the atria and great arteries removed showing the relationship between the four valves at the base of the heart
Understanding the specific anatomies of the arterial valves requires an appreciation of their ventricular supporting structures themselves. Only part of this support is provided by the so-called fibrous skeleton (Fig. 2.4). In the human heart, the components of the skeleton support the aortic-mitral unit, binding it into the roof of the left ventricle. Inconstant cords of fibrous tissue then extend from the margins of the fibrous continuity between the aortic and mitral valve to support the mural (anterior) leaflet of the mitral valve. It has been described previously by the authors that the position of the aortic valve within the cardiac base makes it the centerpiece of the organ [3]. The central fibrous body, the strongest portion of the cardiac skeleton, is formed by the union of the right fibrous trigone with the membranous part of the ventricular septum. The right trigone itself is the rightward end of the area of fibrous continuity between the leaflets of the aortic and mitral valves. The smaller left fibrous trigone is formed at the leftward end of this zone of fibrous continuity [3].
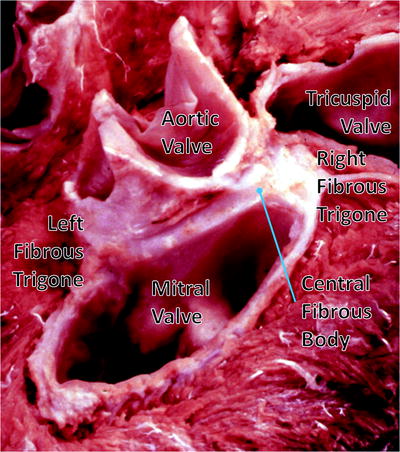
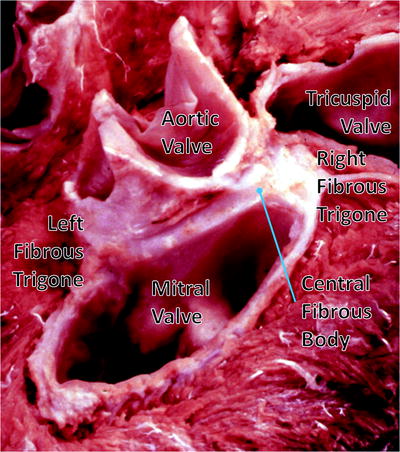
Fig. 2.4
Dissection of the cardiac base with the atrial walls and great vessels removed. It shows the coronet shape of the aortic root and its relationship with the mitral valve. The image is reproduced by kind permission of Professor Robert H. Anderson, and was published initially in “Cardiac Anatomy” [34]. This figure was published in Cardiac Anatomy: An Integrated Text and Colour Atlas, RH Anderson, AE Becker, and SP Allword, page 239, © Elsevier 1980
The leaflets of the pulmonary valve have no direct fibrous support other than that provided by the valvar sinuses. The basal components of each leaflet are supported by the right ventricular infundibulum. It is this unique positioning of the pulmonary root away from the other valvar structures that makes possible its surgical removal during the Ross procedure, while the presence of the supporting skirt of infundibular musculature facilitates its use as an autograft to replace the aortic valve [3].
2.3 Anatomical Features of the Semilunar Valves
In the most basic anatomical sense, a healthy semilunar valve is composed of three valve leaflets, each attached to its respective sinus, as visualized in Fig. 2.2. These valves lie between the ventricular outflow tracts and the arterial trunks, the main arteries carrying blood away from the heart. This elegant structure is much simpler than that of the atrioventricular valves described in Chap. 1, in that the semilunar valve leaflets do not require a tension apparatus to maintain competency. When closed, the three leaflets of each valve co-apt along zones of apposition or commissures, which are fibrous zones some distance from the free edge of the leaflets. At the center of the valve where all three leaflets co-apt, a distinct fibrous nodule can be found in the center. The valve leaflet margins are attached to the arterial wall in the shape of a half-moon, hence the semilunar moniker. Normally, the regions of the valves where the commissures meet the arterial wall are considerably higher than the seats of the leaflets, thereby giving the valve a crown-like shape. These three points, particularly in the aortic valve, are used to define the sinutubular junctions (Fig. 2.5). Although we have discussed the positioning of the valves in the heart by referring to their respective annuluses, many anatomists contest the idea that there are single defined annuluses for both the pulmonary and aortic valves [4]. Interestingly, there is a defined annulus where the respective arteries are attached to the ventricular outflow tract; however, due to the crown-like structure of the valve, the hemodynamic junction of the valves spans this annulus. This structural shape results in part of the arterial wall being considered a ventricular structure (in a hemodynamic sense) and part of the ventricular wall (hemodynamically an arterial structure). Just distal to the valves are the arterial sinuses that are represented by dilations of the artery positioned above each leaflet and additionally house the coronary artery ostium. The sinus also provides a recess for the valve leaflets to retract into, allowing for unrestricted flow from the ventricle to the artery. Finally, the virtual ring, upon which many annular measurements are based and which defines the basal plane of aortic valve, is defined by the three anatomical anchors at the nadir of each aortic leaflet [5]. These features are illustrated by the diagram in Fig. 2.5. The position and definition of the valve annulus is often contested by different medical specialists and a recent questionnaire highlighted the current lack of consensus between physicians regarding the optimal means of describing the semilunar valve anatomy [6]. As such it is important to be precise in the definition of exactly what is being measured when documenting the size and shape of the semilunar valve annuluses.
Fig. 2.5
Idealized three-dimensional arrangement of the semilunar valve (this diagram represents an aortic root). The model contains three circular rings with the leaflets suspended within the root in crown-like fashion. The cartoon is reproduced by kind permission of Professor Robert H. Anderson, who retains the intellectual copyright in the original image [3]. We acknowledge the excellent artwork created by Gemma Price. This same figure is being published in two Springer publications at the same time (Heart Valves: From Design to Clinical Implantation and The Clinical Anatomy and Pathology of the Human Arterial Valves: Implications for Repair or Replacement, J Cardiovasc Transl Res, MG Bateman, AJ Hill, JL Quill, and PA Iaizzo, 2013 Jan 17 [Epub ahead of print], PMID: 23325456)
2.3.1 The Functioning of the Semilunar Valves
When a semilunar valve is functioning correctly, the leaflets are pushed into the sinus during myocardial contraction (systole) to allow blood to leave the ventricles. As the myocardium relaxes and the pressure within the ventricle drops below the pressure distal to the valve in the arterial system (the aorta or pulmonary artery), the valve snaps shut. This usually happens soon after ventricular systole but before the heart has completely relaxed, so that during diastole, when the chambers are filling through the atrioventricular valves, the leaflets of the semilunar valves remain tightly closed. A positive pressure difference between the aorta and the coronary sinus, which lies within the right atrium, allows for the flow of blood through the coronary vasculature. Thus, it should be noted that the heart muscle is perfused with blood when the semilunar valves are closed and the cardiac myocytes are relaxing.
Figures 2.6 and 2.7 show image sequences of the functional movements of the pulmonary and aortic valves respectively; these images were obtained from reanimated human hearts employing Visible Heart® methodologies [7, 8]. See Chap. 15 for an in-depth description of this technique. The images include views of semilunar valves from above (i.e., from videoscopes within the pulmonary artery and the aorta) and from below (with videoscopes within the right and left ventricular outflow tracts).
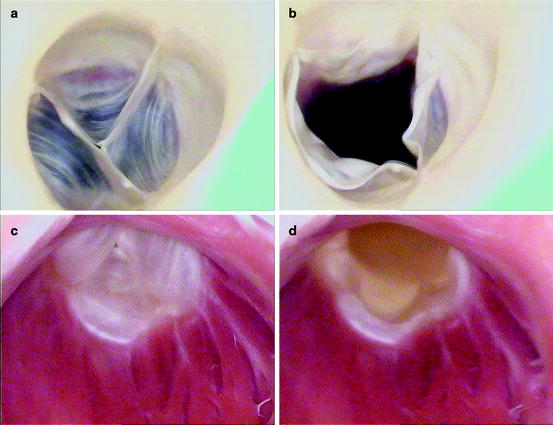
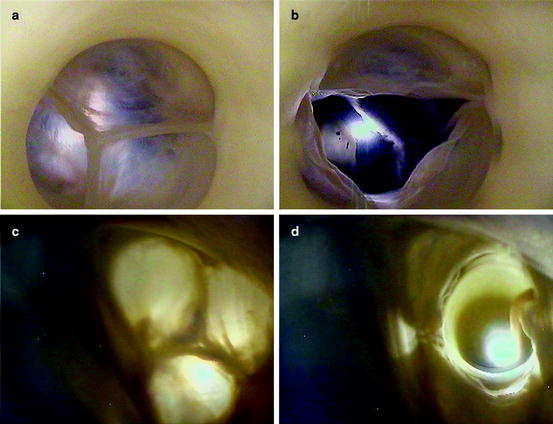
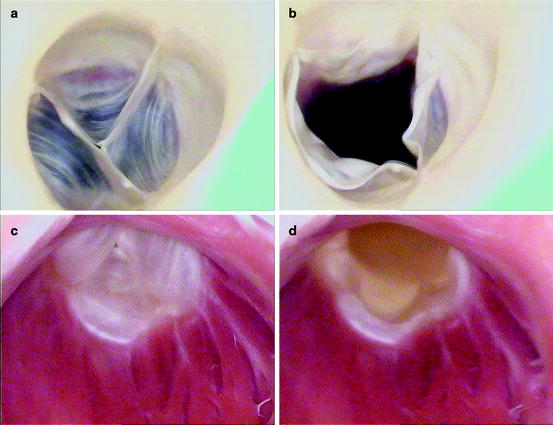
Fig. 2.6
Internal videoscopic images of the pulmonary valve from above (a, b) and below (c, d) during systole (a, c) and diastole (b, d) obtained employing Visible Heart® methodologies
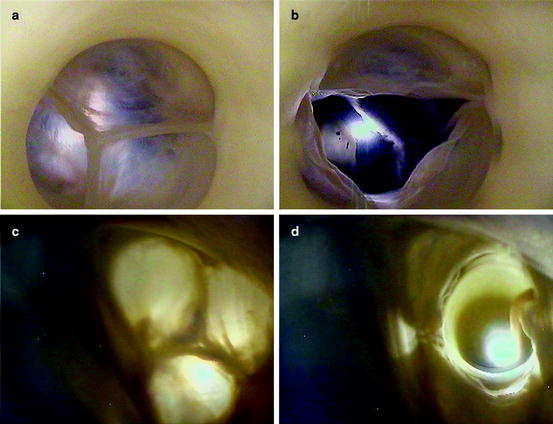
Fig. 2.7
Internal videoscopic images of the aortic valve from above (a, b) and below (c, d) during systole (a, c) and diastole (b, d) obtained employing Visible Heart® methodologies
In general, dysfunctions of the semilunar valves are usually characterized by one of two symptoms: failure of the valves to successfully close or failure of the valves to successfully open. Such dysfunctions of the valves during systole, i.e., failure of the valve to successfully open, are defined as stenosis of the valve. This pathology is characterized by reduction in the effective orifice area of the valve (the size of the opening that allows blood to pass), which in turn forces the ventricles to work harder to move blood to the body or lungs. Dysfunctions of the semilunar valves during diastole, when the ventricles are relaxing, result in regurgitation; this occurs when blood is allowed back into the ventricle from the arterial system, overloading the ventricles and potentially causing chronic heart failure. These pathologies are described in more detail in Chap. 6.
2.3.2 Histologic Features of the Semilunar Valves
It was Gross who first drew attention to the specific histological structures of the arterial valves, his account then being endorsed by others such as Misfeld and colleagues [9, 10]. Each leaflet of the semilunar valve has a fibrous core, or fibrosa, with an endothelial lining containing delicate sheets of elastin on its arterial and ventricular aspects. This so-called fibrous “backbone” is represented by a dense collagenous layer, which gives way to a much looser structure, or spongiosa, toward the ventricular aspects of the leaflet cusps. The zone of apposition of the leaflets consists of an abrupt thickening of the fibrous layer made up of closely packed vertically directed fibers and builds at the central portion of the free edge, creating a node termed the Nodulus Arantii [9, 10]. Figure 2.8 displays a cross-section of an aortic valve leaflet displaying the varying tissue types [11].