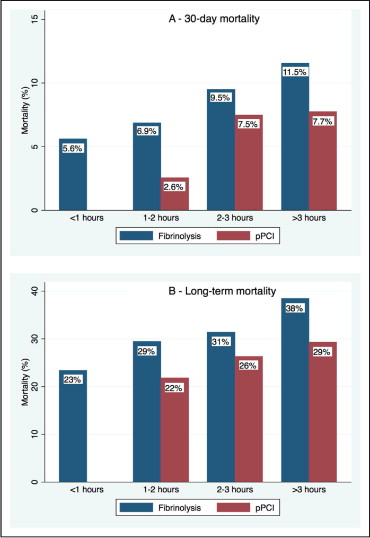
The interval from the first alert of the healthcare system to the initiation of reperfusion therapy (system delay) is associated with mortality in patients with ST-segment elevation myocardial infarction treated with primary percutaneous coronary intervention (pPCI). The importance of system delay in patients treated with fibrinolysis versus pPCI has not been assessed. We obtained data on system delay from the Danish Acute Myocardial Infarction-2 study, which randomized 1,572 patients to fibrinolysis or pPCI. The study end points were 30-day and 8-year mortality. The short system delays were associated with reduced absolute mortality in both the fibrinolysis group (<1 hour, 5.6%; 1 to 2 hours, 6.9%; 2 to 3 hours, 9.5%; and >3 hours, 11.5%; test for trend, p = 0.08) and pPCI group (<1 hour, not assessed; 1 to 2 hours, 2.6%; 2 to 3 hours, 7.5%; >3 hours, 7.7%; test for trend, p = 0.02). The lowest 30-day mortality was obtained with pPCI and a system delay of 1 to 2 hours (vs fibrinolysis within <1 hour, adjusted hazard ratio 0.33; 95% confidence interval 0.10 to 1.10; p = 0.07; vs fibrinolysis within 1 to 2 hours, adjusted hazard ratio 0.37; 95% confidence interval 0.14 to 0.95; p = 0.04). pPCI and system delay >3 hours was associated with a similar 30-day and 8-year mortality as fibrinolysis within 1 to 2 hours. In conclusion, short system delays are associated with reduced mortality in patients with ST-segment elevation myocardial infarction treated with fibrinolysis as well as pPCI. pPCI performed with a system delay of <2 hours is associated with lower mortality than fibrinolysis performed with a faster or similar system delay.
The reduction in the interval to reperfusion is important to decrease mortality in patients with ST-elevation myocardial infarction (STEMI). Previous studies have focused on a reduction in patient delay (i.e., interval from symptom onset to when the patient alerts the healthcare system), but even large-scale media campaigns have failed to successfully achieve a reduction in patient delay or mortality. The current American and European guidelines have mainly focused on the door-to-balloon (D2B) or door-to-needle (D2N) time as indicators of the quality of care and predictors of mortality. These intervals, however, are short compared to the cumulated time from symptom onset to the initiation of reperfusion therapy (i.e., treatment delay) and do not reflect the entire interval that can be modified by the healthcare system. System delay (i.e., the interval from when the patient alerts the healthcare system to reperfusion therapy) might be more optimal as a performance measure, because it holds all the healthcare-related delay. We have recently shown that system delay was associated with mortality in a registry cohort of 6,209 patients with STEMI treated with primary percutaneous coronary intervention (pPCI). The importance of system delay in patients treated with fibrinolysis has neither been reported nor been compared to system delay with pPCI. Hence, the purpose of the present study was to compare the relative effect of system delay after fibrinolysis and pPCI as a predictor for 30-day mortality and long-term mortality.
Methods
The study population included patients enrolled in the Danish Acute Myocardial Infarction-2 (DANAMI-2) trial. The DANAMI-2 trial randomly assigned 1,572 patients with STEMI to treatment with fibrinolysis or pPCI. Patients who emigrated during follow-up were included in the analyses and censored on the day of emigration. All-cause mortality data were acquired from the Danish Civil Registration System in March 2008.
The definitions of the intervals are given in Figure 1 . The interval of the first balloon inflation is usually used as the time of reperfusion in pPCI; however, reperfusion often takes place before balloon inflation (e.g., during wiring or thrombectomy). Because data on the first wiring were not available and because the first contrast injection is followed within a few minutes by the first coronary intervention, we decided to use the first contrast injection as the interval of the first intervention. Acknowledging the widespread acceptance of the D2B delay as a performance measure, we decided to use the D2B delay synonymously with the time from arrival at the invasive center to the first contrast injection. The patients were divided into 4 groups according to the system delay (<1, 1 to 2, 2 to 3, and >3 hours). In the pPCI group, only 6 patients had a system delay time of <1 hour. Therefore, these 6 patients were included in the 1 to 2-hour system delay group.
The Pearson chi-square test was used for comparison of categorical variables. Continuous variables are reported as the median (interquartile range). The groups were compared using the analysis of variance when normally distributed and the Kruskal-Wallis rank-sum test if not normally distributed. Kaplan-Meier curves were used to illustrate the cumulative mortality and compared using the log-rank test. Multivariate Cox regression analysis, adjusting for age, heart rate at admission, and diabetes, was used to model survival. A p value of ≤0.05 was considered significant (2-sided testing).
Results
Figure 1 illustrates the different intervals of treatment delay. The median treatment delay for all patients was 191 minutes (interquartile range 135 to 287) and differed among patients in the fibrinolysis, pPCI-invasive, and pPCI-referral groups ( Table 1 ). The shortest treatment delay was observed in the fibrinolysis group and the longest treatment delay was in the pPCI-referral group. The patients treated with fibrinolysis and pPCI had similar patient delays ( Table 1 ). The emergency medical service delay was slightly shorter in the fibrinolysis group than in the pPCI-invasive and pPCI-referral groups ( Table 1 ). The median distance for transfer from the referral hospitals to the pPCI centers was 50 km (interquartile range 3 to 150). The system delay and D2N/D2B time differed among the 3 treatment categories ( Table 1 ), with fibrinolysis associated with the shortest delay and pPCI referral with the longest delay.
| Variable | Fibrinolysis Group | pPCI-Invasive Group | pPCI-Referral Group | p Value |
|---|---|---|---|---|
| Patient delay | 53 (15–135) | 48 (16–120) | 55 (15–129) | 0.70 |
| Emergency medical service call to arrival at local hospital | 35 (22–57) | 40 (25–65) | 40 (24–61) | 0.03 |
| In-door-out-door at local hospital | — | — | 57 (30–87) | — |
| Transfer time | — | — | 31 (19–45) | — |
| Door-to-needle/door-to-balloon time | 50 (40–70) | 81 (65–98) | 14 (11–29) | <0.001 |
| System delay | 90 (70–130) | 127 (98–157) | 148 (120–183) | <0.001 |
| Treatment delay | 165 (110–269) | 183 (137–285) | 215 (162–312) | <0.001 |
Data on the treatment delay was missing for 21 patients, 1 patient had missing patient delay data, 22 had missing system delay data, and 77 had missing D2N/D2B time data. The median follow-up interval was 7.8 years (interquartile range 7.1 to 8.5). The vital status at end of follow-up was unknown for 4 patients in the fibrinolysis group and for 4 patients in the pPCI group; all 8 of these patients emigrated during follow-up and were censored on the day of emigration.
The baseline variables for the patients in the 4 different system delay groups are listed in Table 2 . In the fibrinolysis group, the age, gender distribution, number of patients with previous myocardial infarction, number of patients with previous stroke, heart rate, and systolic blood pressure differed among the system delay groups. In the pPCI group, the number of patients with hypertension, diabetes, and previous stroke differed among the system delay groups.
| Variable | Fibrinolysis (h) | pPCI | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 0–1 (n = 107) | 1–2 (n = 452) | 2–3 (n = 137) | >3 (n = 78) | p Value | 0–1 (n = 0) | 1–2 (n = 234) | 2–3 (n = 361) | >3 (n = 181) | p Value | |
| Age (years) | 61 (50–69) | 63 (55–73) | 66 (56–76) | 63 (54–76) | 0.02 | — | 62 (53–71) | 62 (53–71) | 66 (55–74) | 0.17 |
| Men | 83.2% | 72.4% | 67.9% | 78.2% | 0.04 | — | 76.9% | 70.6% | 74.0% | 0.43 |
| Hypertension | 16.8% | 20.2% | 20.4% | 29.5% | 0.19 | — | 18.9% | 23.2% | 13.9% | 0.01 |
| Diabetes mellitus | 10.3% | 6.9% | 5.8% | 6.1% | 0.59 | — | 4.3% | 9.2% | 7.2% | <0.001 |
| Current smoker | 52.8% | 61.6% | 55.3% | 55.3% | 0.11 | — | 63.0% | 57.8% | 52.5% | 0.53 |
| Previous acute myocardial infarction | 15.9% | 9.7% | 10.2% | 20.5% | 0.02 | — | 11.2% | 11.5% | 10.5% | 0.85 |
| Previous coronary angioplasty | 1.9% | 2.2% | 2.9% | 5.1% | 0.47 | — | 4.3% | 4.8% | 3.9% | 0.30 |
| Previous stroke | 1.9% | 3.3% | 5.1% | 10.3% | 0.02 | — | 3.4% | 2.0% | 2.8% | <0.001 |
| Heart rate (beats/min) | 70 (60–80) | 70 (60–84) | 74 (64–86) | 80 (70–88) | 0.01 | — | 70 (60–84) | 75 (60–88) | 76 (65–88) | 0.46 |
| Systolic blood pressure (mm Hg) | 135 (117–150) | 132 (111–150) | 139 (120–150) | 140 (120–160) | 0.02 | — | 136 (120–150) | 135 (120–155) | 140 (120–160) | 0.88 |
| Anterior wall acute myocardial infarction | 50.5% | 51.8% | 53.3% | 59.0% | 0.66 | — | 52.6% | 52.9% | 54.7% | 0.99 |
At 30 days of follow-up, 113 patients had died, 61 in the fibrinolysis group and 52 in the pPCI group. The system delay was associated with incremental mortality in the fibrinolysis group (test for trend, p = 0.08; Figure 2 ) and in the pPCI group (test for trend, p = 0.02; Figure 2 ). Treatment with pPCI within 1 to 2 hours was associated with a nonsignificant 67% reduced mortality rate (2.6% vs 5.6%; adjusted hazard ratio [HR] 0.33, 95% confidence interval [CI] 0.10 to 1.19; p = 0.07) comparison to fibrinolysis within <1 hour. Furthermore, pPCI within 1 to 2 hours was significantly better than fibrinolysis within 1 to 2 hours (2.6% vs 6.9%; adjusted HR 0.37, 95% CI 0.14 to 0.95; p = 0.04). A system delay >3 hours in the pPCI group resulted in similar mortality as fibrinolysis started with a system delay of 1 to 2 hours (7.7% vs 6.9%; adjusted HR 0.97, 95% CI 0.52 to 1.83; p = 0.94).