27 Supraventricular Tachycardia
Etiology and Pathogenesis
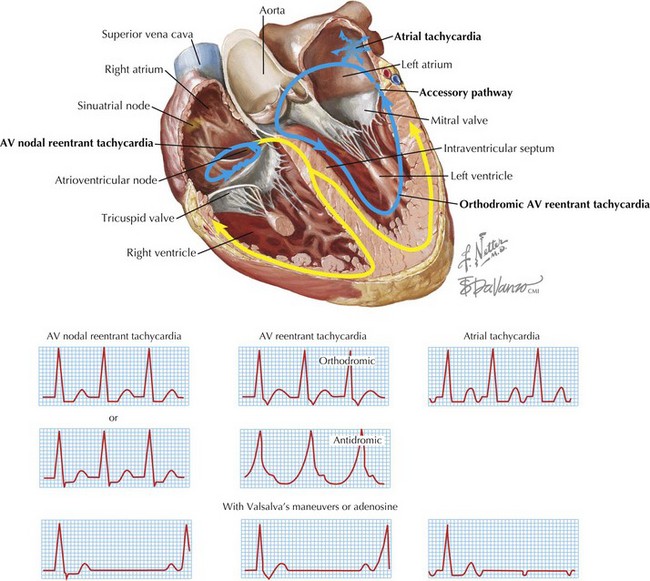
This chapter discusses the three categories of SVT (AVNRT, AVRT, and AT). The other major atrial arrhythmias, atrial fibrillation and atrial flutter, are discussed in Chapter 28.
Differential Diagnosis
Atrioventricular Nodal Reentrant Tachycardia
Mechanism
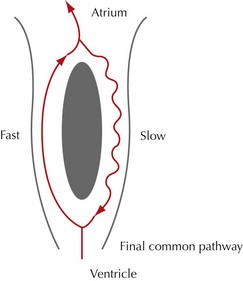
Excluding atrial fibrillation and atrial flutter, the most common SVT is AVNRT, accounting for approximately 60% of cases. AVNRT is characterized by the presence of two distinct pathways within the AV node that facilitate reentry by allowing an electrical impulse to cycle in one direction, creating a reentrant loop or circuit. The presence of two pathways is often referred to as dual AV nodal physiology. One pathway has a short conduction time but a long refractory period (fast pathway); the second has a long conduction time but a short refractory period (slow pathway). The differing conduction times and refractory periods of each pathway allow the electrical impulse to cycle in only one direction, using one pathway in the anterograde direction and one pathway in the retrograde direction. The pathways are joined into one final common pathway before impulses exiting the AV node to continue to the bundle of His (Figs. 27-1 and 27-2).
ECG Recognition
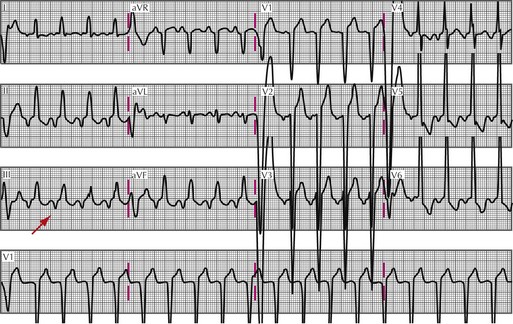
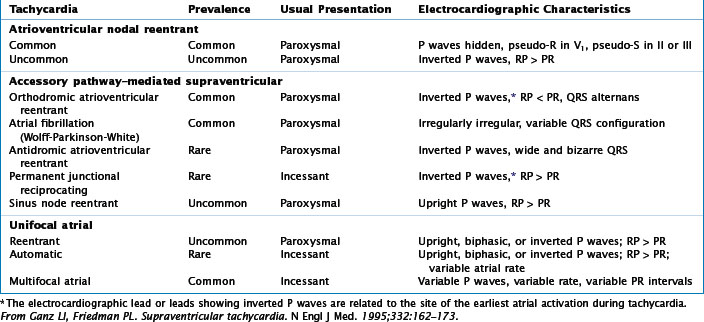
Typical AVNRT can be distinguished from atypical AVNRT on an ECG by comparing the location of the P wave in relation to the QRS complex. In typical AVNRT, near-simultaneous conduction to the ventricles via the slow pathway anterogradely and to the atria via the fast pathway retrogradely may rarely make P wave visible on the ECG because they are inscribed in the QRS complex. When visualized, the P waves occur in close proximity to the QRS, creating a short RP interval (RP interval less than half the RR interval). This can sometimes manifest as a “pseudo-S wave” in the inferior leads II, III, and aVF, and a “pseudo-R wave” in lead V1 (Fig. 27-3). Typical AVNRT, therefore, is an example of a “short-RP” tachycardia. In contrast, P waves are clearly visible in atypical AVNRT. Due to retrograde conduction through a slow pathway, the presence of the P wave occurs later than the QRS complex, resulting in an RP interval that is frequently longer than half the RR interval, called a long RP tachycardia (Fig. 27-4).
Another ECG feature that may help to distinguish typical from atypical AVNRT is the mode of initiation of the reentrant circuit. Though obviously difficult to obtain on a standard 12-lead ECG, should a rhythm strip be available that demonstrates an initiating atrial premature beat, the diagnosis is more likely typical AVNRT. A ventricular premature beat is more likely to precipitate an atypical AVNRT (Table 27-1).