Chapter 64
Superior Vena Cava Occlusion
Endovascular Treatment
Carlos F. Bechara, Peter H. Lin
Superior vena cava (SVC) occlusion precludes normal blood venous return to the heart. This condition, also known as SVC syndrome, is an uncommon occurrence that affects approximately 15,000 patients each year in the United States. The SVC functions as the primary venous drainage system from the head, neck, upper extremities, and upper thorax; the occlusion can be due to an extraluminal compression or intraluminal obstruction in nature. In general, SVC is 6 to 8 cm long and extends from the junction of the right and left innominate veins to the right atrium. Located in the middle mediastinum, the SVC is surrounded by relatively rigid structures, such as the trachea, right bronchus, sternum, aorta, pulmonary artery, and paratracheal and perihilar lymph nodes. Because the SVC is a low-pressure and thin-walled venous structure, the venous wall of the SVC can be compressed easily as it traverses the right side of the mediastinum.
SVC syndrome was first reported in 1757, when Dr. William Hunter described it in a patient with syphilitic aortic aneurysm.1 Historically, infections were the most common cause of SVC syndrome. In a study reported in 1954 by Schechter,2 who analyzed 274 confirmed cases of SVC syndrome, 40% were due to either syphilitic aneurysms or tuberculous mediastinitis. In the past 5 decades, there has been a gradual decline of these infectious etiologies as primary causes of SVC syndrome, owing in part to improved antimicrobial therapy. In later reports, carcinoma of the lung resulting in extraluminal SVC compression is the predominant cause of SVC obstruction. Patients with SVC obstruction require immediate diagnostic evaluation and therapeutic intervention, because it is common in patients with undiagnosed malignancy within the thorax.
Pathophysiology
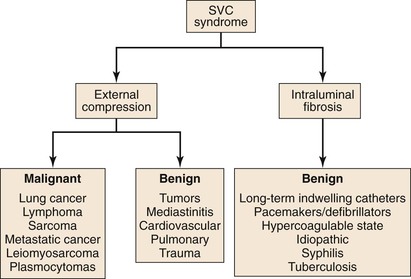
The majority of cases of SVC syndrome are caused by neoplastic progression into the venous wall with resultant tumor mass compression against the relatively fixed, thin-walled SVC. Alternatively, SVC obstruction can also be due to intravascular thrombosis caused by neoplastic involvement. Postmortem studies have demonstrated that complete SVC obstruction is the result of extrinsic tumor compression in conjunction with intravascular thrombosis. In contrast, incomplete SVC obstruction is more frequently caused by extrinsic compression without associated intravascular thrombosis.3,4 Figure 64-1 summarizes various causes of SVC syndrome.
Because of the SVC’s location, primary carcinoma of the lung located in the right upper lung lobe has a higher likelihood of causing SVC obstruction than pulmonary carcinomas located elsewhere. Among various neoplastic etiologies of SVC syndrome, mediastinal malignancy is responsible for 80% of cases. Specifically, bronchogenic carcinomas account for 75% to 80% of all cases, with the majority being small-cell carcinomas. Non-Hodgkin lymphoma is responsible for the remaining 10% to 15% of cases of SVC syndrome of malignant etiology. Other malignant causes of SVC syndrome, albeit less common, are Hodgkin disease, metastatic cancers, primary leiomyosarcomas of the mediastinal vessels, and plasmocytomas.
SVC obstruction can be caused by nonmalignant diseases, which account for less than 25% of all cases of SVC syndrome.3–5 Infectious conditions such as syphilis and tuberculosis accounted for the majority of cases of SVC syndrome around the turn of the twentieth century. The development of effective pharmacologic therapy in the past 4 decades has largely eradicated syphilitic and tuberculosis-related SVC syndrome. The most common nonmalignant cause of SVC syndrome is mediastinal fibrosis from an infectious or radiation-induced process.6 With an aging population on the rise, the frequency of placement of central venous devices, such as pacemakers, defibrillators, central venous infusion ports, and long-term hemodialysis catheters, is similarly increasing. As a result, data have shown that benign disease accounted for 35% to 40% of cases of SVC obstruction.7 These indwelling venous devices can cause SVC obstruction through mechanical trauma to the venous endothelium, which can result in intraluminal fibrosis.8–17
Collateral Venous Pathways
Venous collateral network formation can occur from chronic SVC obstruction. There are several important venous collaterals that return venous circulation from the upper half of the torso to the right atrium. The first and most important pathway is the azygos venous system, which includes the azygos vein, the hemiazygos vein, and the connecting intercostal veins. The second pathway involves the internal mammary venous system as well as tributaries and secondary communications to the superior and inferior epigastric veins. The long thoracic venous system, which represents the third collateral venous network, is connected to the femoral veins and vertebral veins. The development of these collateral venous pathways is influenced by the chronicity of SVC obstruction as well as underlying causative factors (Table 64-1).
Table 64-1
Stanford Classification for Superior Vena Cava (SVC) Obstruction
| Type | Description |
| I | Up to 90% stenosis with patency of the azygos vein |
| II | 90% stenosis to complete occlusion of SVC with patency of the azygos vein and antegrade flow through the azygos vein |
| III | 90% stenosis to complete occlusion of SVC with patency of the azygos vein and retrograde flow through the azygos vein |
| IV | Complete occlusion of SVC and one or more of its branches including the azygos vein |
Clinical Presentations and Diagnostic Evaluation
Clinical manifestations of SVC syndrome and diagnostic evaluation of patients in whom it is suspected are described in detail in Chapter 63.
Treatment Considerations
The traditional treatment for SVC syndrome associated with thoracic malignancy has been radiotherapy, chemotherapy, or both. The treatment response varies, depending on the invasiveness of thoracic malignancy, so typically resolution of symptoms may take several months. Although surgical construction of the SVC to bypass the venous obstruction along with removal of the underlying intrathoracic malignancy is an acceptable treatment option, this treatment approach requires a median sternotomy, which represents a major surgical challenge. The treatment benefits and operative morbidities must be weighed carefully against the patient’s life expectancy in those with malignant SVC syndrome. In patients with nonmalignant SVC syndrome, surgical reconstruction of the SVC creates a new venous conduit, which enables future dialysis access of pacemaker placement.
In patients who have overt SVC syndrome or whose disease does not respond to medical therapy, additional catheter-based treatment such as balloon angioplasty or stenting is necessary in order to maintain SVC luminal patency. In contrast to chemotherapy and radiation treatment for malignant SVC syndrome, endovascular stenting of the SVC establishes immediate luminal patency and provides rapid symptomatic relief. Endovascular stenting has been used prior to chemotherapy in neoplastic SVC syndrome with success.18 Similarly, endovascular treatment options can be equally applied to patients with nonmalignant SVC syndrome. In patients whose SVC obstruction is caused by intraluminal thrombosis, thrombolytic therapy to dissolve the thrombus is effective.
On the basis of an abundance of studies, endovascular therapy should be considered the first line of treatment in both malignant and nonmalignant SVC syndrome.19–22 The use of endovascular therapy to treat SVC syndrome has been extended to treat the pediatric and young adult populations.23 The only contraindication to endovascular therapy is inpatients with a contraindication to thrombolytic therapy or anticoagulation. Patients whose symptoms fail to respond or who are not candidates for endovascular therapy should be evaluated for surgical reconstruction.
Techniques of Endovascular Intervention
The endovascular procedure should be performed in either an interventional suite or operating room with a dedicated angiographic capability or a mobile C-arm fluoroscopic unit. Access for percutaneous stenting of the SVC is typically obtained via the femoral vein, but a brachial, basilic, or internal jugular vessel can also provide useful therapeutic access to the central veins. In the event of venous occlusion involving the SVC or brachiocephalic veins, bilateral upper extremity venous access via either a brachial or basilic vein should be considered because it facilitates the catheterization of the central vein occlusion. In addition to femoral access, additional upper extremity venous access is necessary in about 20% of the cases.22 This dual venous access not only enables antegrade and retrograde venograms but also facilitates crossing the SVC lesion.
Femoral venous access is typically established with a 7F introducer sheath (Boston Scientific, Natick, Mass). A 260-cm Bentson guide wire (Boston Scientific) followed by a pigtail catheter is placed in the SVC. Venography of the SVC and brachiocephalic veins is performed via a femoral approach to visualize the SVC lesion. Whenever possible, a hydrophilic guide wire is used to traverse the SVC lesion. Once the lesion is successfully cannulated with the hydrophilic guide wire, the guide wire is exchanged for a stiff Amplatz wire (Boston Scientific) or a Lunderquist wire (Cook Medical, Inc., Bloomington, Ind) for balloon or stent delivery. If the wire is unable to cross an SVC occlusion or a high-grade lesion, a thrombolytic infusion catheter is placed for delivery of a thrombolytic drug either as a bolus or continuously for a certain period.
Systemic anticoagulation with intravenous heparin (5000 U/kg) is given prior to any catheter-based intervention. We routinely perform an initial SVC balloon dilatation because this maneuver widens the lumen, facilitating subsequent stent deployment; other researchers have similarly supported this maneuver.24,25 In contrast, yet others have advocated avoiding this maneuver to reduce the risk of thrombus embolization.26 Treatment by means of balloon dilatation alone yields poor clinical results in the long term owing to a high rate of restenosis. Given the available clinical results, stenting of the SVC lesion is preferred over to SVC balloon angioplasty.
Balloon angioplasty to dilate the SVC or brachiocephalic venous lesion is performed with either a 10 mm × 40 mm or 12 mm × 40 mm balloon angioplasty catheter. Following balloon dilatation of the SVC lesion, either a balloon-expandable stent or a self-expanding stent is deployed across the lesion. Infrequently a covered stent-graft is used to treat the SVC lesion. Occasionally, more than one stent is needed to treat the underlying pathology. Post-stenting balloon dilatation is routinely performed when a self-expanding stent or a stent-graft is deployed. In our series, if the segment of SVC adjacent to the stricture was greater than 16 mm in diameter, a bilateral brachiocephalic “kissing stent” technique using either a 12-mm- or a 14-mm-diameter stent is performed.22 Completion venography is obtained to document treatment results (Fig. 64-2). Introducer sheaths and guide wires are next removed, and manual compression is applied to achieve hemostasis.
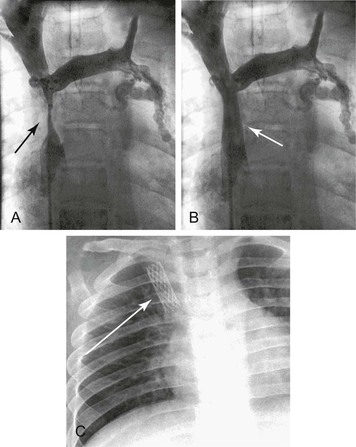
Figure 64-2 Images of a patient with symptomatic superior vena cava (SVC) syndrome. A, A high-grade SVC stenosis is depicted in the venogram (arrow). B, Luminal patency was established with the placement of a balloon-expandable Palmaz stent (arrow). C, Chest radiograph demonstrated the location of the Palmaz stent (arrow).
In the event of chronic venous occlusion whereby conventional catheter and guide wire techniques are not successful in crossing the venous occlusion, radiofrequency guide wire technology has been shown to be beneficial in establishing access across the venous occlusion. The PowerWire Radiofrequency Guidewire (Baylis Medical Company Inc, Montreal) can be used to facilitate crossing vessels with thrombotic occlusion. This 0.035-inch wire has a hot tip and low-friction insulation but is not steerable. The device monitor displays delivered radiofrequency power, impedance, and elapsed time to allow for continuous monitoring. The utility of this technology was highlighted in a series of three patients with malignant SVC syndrome whose SVC occlusions were successfully crossed with use of a radiofrequency guide wire, followed by stent placement.27
Thrombolytic Therapy
The first successful thrombolytic therapy in SVC syndrome caused by a pacemaker lead was described in 1974, in which streptokinase was delivered via catheter-directed infusion.28 This treatment modality with or without angioplasty or stenting has been well validated.28–31 Thrombolytic therapy could lead to complete clot resolution or could partially recanalize the thrombus, allowing further endovascular management such as balloon angioplasty or stenting once the lesion is crossed with a wire. In general, chronic venous occlusions tend to be easier to cross with a wire than chronic arterial occlusions. Catheter-directed thrombolysis utilizes a smaller thrombolytic dose than systemic thrombolysis. The earlier the administration of thrombolytic therapy after the onset of symptoms, the better the response and the thrombus resolution. Most nonmalignant SVC syndromes respond to thrombolytic therapy, because the patients present with subacute or acute-on-chronic thrombosis. The process of thrombotic occlusion in malignant SVC syndrome is more insidious in nature. By the time symptoms occur, sufficient venous collaterals have usually developed.
When thrombosis occurs and results in SVC occlusion, adjuvant thrombolytic therapy may be beneficial to dissolve the thrombus and unmask the underlying lesion prior to definitive endovascular treatment. Many physicians who performed endovascular stenting for SVC syndrome described the benefits of thrombolytic agents.32 Ariza et al24 administered urokinase in a 500,000 IU bolus followed by an infusion of 80,000 to 100,000 IU/hr for 24 to 48 hours after stent implantation. Gray et al33 described the safety and benefit of using streptokinase and urokinase for thrombolysis in SVC syndrome of both malignant and benign etiologies. They reported successful results when thrombolytic infusion was administered through an indwelling catheter within 5 days of the onset of symptoms. In SVC or brachiocephalic thrombotic occlusion, direct thrombolytic infusion via a catheter embedded in thrombus or through a preexisting indwelling catheter is an effective technique for treating SVC thrombosis. Rosenblum et al34 reported the utility of thrombolytic therapy in successfully treating patients with SVC syndrome due to long-term use of indwelling catheter. Sheikh et al25 reported the use of urokinase and recombinant tissue plasminogen activator (t-PA) prior to angioplasty and stent deployment in patients with SVC syndrome.25 Their study shows a high rate of treatment success and supports the use of adjuvant thrombolytic therapy in patients with SVC syndrome with underlying venous thrombosis and no contraindications to thrombolytic therapy. Heparin, oral anticoagulants, or antiplatelet therapy is typically given after IVC stenting, for a duration of at least 6 months and possibly indefinitely.24–26 Overall this anticoagulation is well tolerated and appears to decrease the risk of stent thrombosis, although fatal subdural hematoma was reported in one patient with nonmalignant SVC syndrome.25
Over the past decade, percutaneous mechanical thrombectomy has emerged as an effective treatment modality in patients with thrombotic venous occlusion.35 The clinical advantage of such a thrombectomy system is that it allows simultaneous catheter-directed infusion of thrombolytic agents, thereby creating a pharmacomechanical thrombectomy (PMT) strategy. It is accomplished with the initial administration of thrombolytic agents to exert the pharmacologic benefit of thrombus dissolution, followed by mechanical thrombectomy for thrombus extraction. The pharmacomechanical thrombectomy treatment strategy combines the advantages of pharmacologic thrombolysis and mechanical thrombectomy, in which the thrombolytic dosage can be reduced and the efficacy of mechanical thrombectomy is maximized. This treatment technique was adapted from our previously reported treatment strategy in DVT intervention.35 In our reported series, this pharmacomechanical thrombectomy with rheolytic thrombectomy and catheter-directed tissue plasminogen activator administration has yielded successful treatment outcome in patients with acute thrombosis of the SVC and brachiocephalic vein.22
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree