INDICATIONS/CONTRAINDICATIONS
Right lower lobe segmentectomies account for up to 23% of all segmentectomies. Time-honored indications for these segmentectomies include benign lung lesions, localized and active postprimary tuberculous sequelae, and bronchiectases. Segmentectomies are also indicated in the management of lung cancer patients with marginal cardiopulmonary function. However, irrespective of patient’s cardiopulmonary reserves, segmentectomies are also being increasingly used to resect small-sized (<2 cm) primary lung cancers and metastatic deposits from extrathoracic malignancies, with the aim of sparing lung parenchyma albeit maintaining compliance to the principles of oncologic radicality. In a recent series including 785 patients reported by Schuchert et al., 86% of the segmentectomies had been done for lung cancer. In particular, it has been suggested that for the noninvasive adenocarcinoma histologic subsets and ground-glass opacities with a solid component greater than 25%, segmentectomy can be a reliable alternative to lobectomy. In addition, segmental resections can be used both for bilateral benign and malignant lesions aiming at eradication of the disease, either malignant or benign. Conversely, tumor size crossing the segmental plane, unclear margins at frozen section, incomplete intersegmental nodal clearance, and presence of additional nodules in the same lobe represent contraindications to segmentectomy.
 PREOPERATIVE PLANNING
PREOPERATIVE PLANNING
As a rule, chest CT is obtained for lung cancer staging or to precisely localize the infectious lesion. The adjunct of PET is valuable for nodule characterization only if the lesion is larger than 8 mm to fall within PET resolution capability. Pulmonary lesions are detected with increasing frequency at low-dose CT scan done for lung cancer screening in high-risk patients. Preoperative planning should take into consideration the presence of histotypes with low metastatic potential (former bronchoalveolar carcinomas and carcinoids), previous lung resections on the same or the contralateral side, cardiopulmonary reserves, and technical feasibility of a segmentectomy with regard to the size of the nodule and its location compared to the intersegmental plane. Also, in the event of segmentectomy for primary T1N0 NSCLC, a safe tumor-free margin must be anticipated, i.e., greater than the diameter of the lesion or 2 cm. Recently, the use of highly sophisticated 3D CT scan reconstructions in outlining safe margins prior to segmentectomy has been reported.
 SURGERY
SURGERY
Superior (S6) Right Lower Lobe Segmentectomy
Generalities
Under general anesthesia, the patient is placed on a left lateral decubitus and on one lung ventilation. The right chest is prepped and draped for either a posterolateral or a muscle-sparing thoracotomy. Upon entering the chest, the lobe is prepared as for right lower lobectomy. The division of the pulmonary ligament allows for isolation of the inferior pulmonary vein, which is dissected in the subadventitial plane and then encircled.
Segmental Hilar Dissection
A Kittner is used to sweep the adventitia off the main venous trunk distally onto the segmental branches, the most cranial of which is usually the vein from the apical segment (V6). At this point, V6 is encircled and stapled or doubly ligated.
The attention is then turned to the arterial supply to the lower lobe. In particular, the artery to the apical segment of the lower lobe (A6) can be approached inside the fissure and/or from the posterior mediastinal side (Fig. 23.1). In the fissure, the basilar artery is usually identified at the cross between the lower and middle lobes. Once in the subadventitial plane, the dissection is carried out cranially to identify the middle lobe artery and, opposite to it, A6. At this point, it is useful to divide the posterior part of the major fissure (Fig. 23.2). To this purpose, the space between A6 and the ascending posterior artery to the upper lobe is visualized. The tip of a right-angle clamp is engaged in this space and directed posteriorly toward the interbronchial angle between the right upper lobe bronchus and the bronchus intermedius until the posterior mediastinal pleura is entered (Fig. 23.2). Following this same route, a stapler is inserted and fired so as to expose A6.
The artery to the superior segment of the lower lobe (A6) is dissected, doubly ligated, and divided or stapled. This maneuver uncovers the bronchus to S6 (B6), which is carefully dissected and either divided and oversewn or stapled (Figs. 23.2 and 23.3). If the S6 segmentectomy is being performed for an infected segment, the bronchus should be divided first to avoid spillage of purulent secretions with lung manipulation.
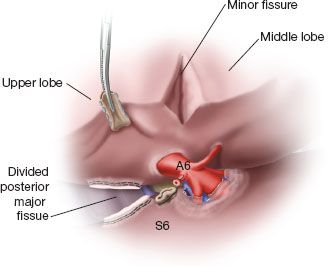
Figure 23.1 Identification of the artery to the superior segment of the right lower lobe (A6), which is ligated and divided. Also visualized is the basilar artery. S6, superior segment.
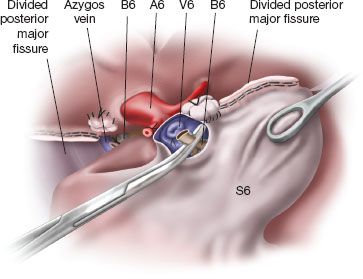
Figure 23.2 The superior segment is rotated anteriorly to demonstrate the divided bronchovascular structures of the superior segment. A clamp is placed on the distal segmental bronchus to prepare for subsequent development of the intersegmental plane. S6, superior segment; B6, bronchus to the superior segment; A6, artery to the superior segment; V6, vein from the superior segment.
The Intersegmental Plane
The rare presence of an additional fissure separating S6 from the remaining segments (identifying the so called “Nelson,” “Devé,” or “Fowler” lobe) will facilitate the creation of an intersegmental plane. However, as a rule, the collapsed lung is cautiously reinflated thus outlining the intersegmental plane by contrast with the atelectatic S6 segment (Fig. 23.3). Alternatively, to improve visualization of the intersegmental plane, a reverse inflation–deflation technique can be used or dye can be injected in the closed distal segmental B6 bronchus. The intersegmental plane is characterized by the presence of an intersegmental vein draining S6 (Fig. 23.4
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


