The experience as a cardiovascular pathologist on sudden cardiac death (SCD) in the young and the impact that the findings had on in vivo diagnosis, treatment, and prevention are herein reported. The story dates back in the late 70s, when a series of juvenile sudden deaths occurred in the Veneto Region, North East of Italy. A successful application for a prospective study on young people dying suddenly (<35 years old, sudden infant death syndrome excluded) was submitted to the regional health authorities, thus implementing a network of collaboration with anatomic and forensic pathologists, to collect all such events and to gather epidemiological data. The project is still in progress, and since then we studied >650 hundreds consecutive juvenile SCD cases, allowing to identify the culprit diseases with abnormalities in the various cardiac structures (aorta, coronary arteries, myocardium, valves, and conduction system). The long standing Veneto Region experience clearly shows that autopsy still plays a pivotal role in the study and prevention of SCD and should be carried out regularly in the young. With time, the investigation of SCD necessarily moved from the classic postmortem study to molecular autopsy. In conclusion, SCD prevention in the young has to be faced by an interdisciplinary team, including pathologists, cardiologists, sport physicians, and geneticists, with a translational approach; the clinicopathologic correlation method still being the polar-star. In other words, the game in the fight against SCD is still played in the anatomical theater, the place where “death enjoys to save lives.”
I come from Italy and belong to the University of Padua, which was founded in 1222 and became the University of the Serenissima Republic of Venice in 1404. Here, during the Italian Renaissance, the “microcosme” of human body was explored in detail and illustrated by Andreas Vesalius in the De Humani Corporis Fabrica , published in 1543 ; the theory of blood circulation was put forward by William Harvey in the Exercitatio Anatomica de Motu Cordis et Sanguinis in Animalibus in 1628, thanks to dissections carried out by Fabrici ab Acquapendente in the anatomical theater, the first research laboratory in the history of medicine; the pathology of cardiovascular disease was investigated by Giovanni Battista Morgagni in De Sedibus et Causis Morborum per Anatomen Indagatis , 1761, thus establishing pathological anatomy as a science and changing the course of medical diagnosis.
Paul Dudley White, the father of American Cardiology, loved Italy. In 1929, he spent a sabbatical of 6 months in Anacapri, Island of Capri, to write the first edition of his book on heart disease. When in Italy, he became a fan of “Mediterranean Diet”, joining Ancel Keys in pursuing the concept that lifestyle and diet play a pivotal role in prevention of coronary artery disease (CAD; Figure 1 ). They became, with several travels, the “medical Marco Polos” of preventive cardiology and cardiovascular disease epidemiology.
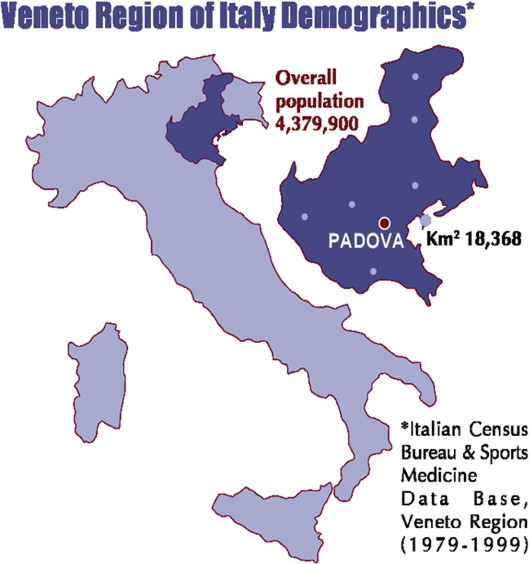
Our experience on sudden cardiac death (SCD) in the young dates back in the late 70s, when a series of juvenile sudden deaths occurred in the Veneto Region ( Figure 2 ). We submitted a successful application for a prospective study on young subjects dying suddenly (<35 year old, sudden infant death syndrome excluded) to the regional health authorities, thus implementing a network of collaboration with anatomic and forensic pathologists, to collect all such events and to gather epidemiological data. The project is still in progress, and since then we studied >650 hundreds consecutive SCD cases in the young, allowing to identify the various culprit diseases.
Gross and microscopic examinations were the classic tools of investigation. We concentrated on SCD, which is the obvious diagnosis when excluding other causes, and realized that the cardiac pathophysiology mechanism is mechanical (cardiac tamponade because of aortic rupture or pulmonary thromboembolism) or, much more frequently, arrhythmic because of ventricular fibrillation (VF). The hidden substrates were found in any heart structure (aorta, coronary artery, myocardium, valves, and conduction system). However, we soon learned that even structurally normal hearts may undergo electrical storm (SCD without anatomical substrate [“mors sine materia”]), and we are now aware that the defect, in these circumstances, is purely functional, namely a disorder of ion channels.
Aortic Disease
In 4% of cases, the cause of death was found into the laceration and external rupture of the ascending aorta with cardiac tamponade. The aortic dissection always occurred in the setting of a congenital and/or heredofamilial condition, namely Marfan syndrome and bicuspid aortic valve (BAV) with or without aortic isthmic coarctation. The aortic wall fragility consisted of severe disruption and/or loss of elastic fibers and smooth muscle cells of the tunica media (medial necrosis), which was equal in Marfan and BAV cases.
As far as BAV, parallel echocardiographic investigations, carried out in living children and male conscripts, showed that the incidence of BAV in children is 0.8% and that nearly 50% of young asymptomatic people with BAV demonstrated a significantly dilated aortic root, supporting the concept of the existence of a BAV “syndrome.”
Coronary Artery Disease
Premature coronary atherosclerosis ranks first as a cause of SCD (18%), particularly in young people >20 years. The substrate usually consists in a single vessel disease with the atherosclerotic plaque located in the proximal left anterior descending coronary artery (“the SCD arterial segment”). Only in 30% of cases, VF is precipitated by acute occlusive coronary artery thrombosis, the latter usually occurring on a noncritical atherosclerotic plaque, triggered either by endothelial erosion or more rarely by fibrous cap rupture. In 70% of cases, the obstruction is most probably due to vasospasm, which has been proved to occur in SCD cases with transient ST-segment elevation at Holter monitoring, followed by onset of VF at reperfusion. Overt acute myocardial infarction, with classic histologic features of coagulative myocyte necrosis, was never observed in young SCD cases with atherosclerotic CAD.
Apart from rare cases of coronary arteritis, another acquired CAD accounting for abrupt coronary artery occlusion occurred in women and consisted in the spontaneous tunica media dissection of a major subepicardial coronary artery, with evidence of eosinophilic infiltrate in the targeted vessel.
The usual congenital abnormality related to SCD was the anomalous origin of a coronary artery from the opposite (“wrong”) sinus, which is the right coronary artery from the left sinus or the left coronary artery from the right sinus. The anomalous coronary vessel showed an obtuse angle takeoff and a proximal course between the aorta and the pulmonary artery, with a slit-like lumen and often an intramural aortic course of the first tract.
Coronary Artery Disease
Premature coronary atherosclerosis ranks first as a cause of SCD (18%), particularly in young people >20 years. The substrate usually consists in a single vessel disease with the atherosclerotic plaque located in the proximal left anterior descending coronary artery (“the SCD arterial segment”). Only in 30% of cases, VF is precipitated by acute occlusive coronary artery thrombosis, the latter usually occurring on a noncritical atherosclerotic plaque, triggered either by endothelial erosion or more rarely by fibrous cap rupture. In 70% of cases, the obstruction is most probably due to vasospasm, which has been proved to occur in SCD cases with transient ST-segment elevation at Holter monitoring, followed by onset of VF at reperfusion. Overt acute myocardial infarction, with classic histologic features of coagulative myocyte necrosis, was never observed in young SCD cases with atherosclerotic CAD.
Apart from rare cases of coronary arteritis, another acquired CAD accounting for abrupt coronary artery occlusion occurred in women and consisted in the spontaneous tunica media dissection of a major subepicardial coronary artery, with evidence of eosinophilic infiltrate in the targeted vessel.
The usual congenital abnormality related to SCD was the anomalous origin of a coronary artery from the opposite (“wrong”) sinus, which is the right coronary artery from the left sinus or the left coronary artery from the right sinus. The anomalous coronary vessel showed an obtuse angle takeoff and a proximal course between the aorta and the pulmonary artery, with a slit-like lumen and often an intramural aortic course of the first tract.
Myocardial Disease
Myocarditis
Inflammation of the myocardium is strongly proarrhythmic and explained 14% of cases of SCD in our experience. Lymphocytic myocarditis is the usual substrate. The burden of inflammation is rarely massive as observed in cardiogenic shock; on the contrary, it is usually scarce but enough to trigger VF. Employment of polymerase chain reaction at postmortem, even in paraffin embedded myocardium, allowed to identify a viral cause in 2/3 of cases, and enterovirus (coxsackie virus) represented the leading infective agent after an apparently trivial flu episode.
Genetically determined cardiomyopathies
Hypertrophic cardiomyopathy (HC) and arrhythmogenic cardiomyopathy (AC) shared the same rate among causes of SCD, 10% each. HC, besides the classic gross and histologic features (cardiomegaly, ventricular hypertrophy mostly septal asymmetric, subaortic plaque, and myocardial disarray; Figure 3 ), showed a peculiar finding consisting of scars within the hypertrophy, a substrate that clearly contributes to enhance the life-threatening electrical instability. The scar is most probably ischemic in origin and may be because of several factors, including the intramural course of the left anterior descending coronary artery, which is a frequent component of the HC phenotype, and impairs coronary reserve because of compression of small intramural coronary arteries by myocardial hypertrophy during diastole.
AC, first discovered as a cause of SCD in the young in the 1980s just in the Veneto Region, as to deserve for a while the nickname of “Venetian disease,” presents with fibrofatty replacement of the ventricular myocardium, which in the right ventricle may be transmural ( Figure 4 ) as to cause aneurysms formation in the so-called “triangle of dysplasia”, whereas in the left ventricle may be confined to the subepicardial and midmural layers. The substrate is usually biventricular and frequently associated with inflammatory reaction. A peculiar form of isolated left ventricular AC has been recently reported, mostly hidden from the electrocardiographic and echocardiographic viewpoint, which only cardiac magnetic resonance may be able to detect.




