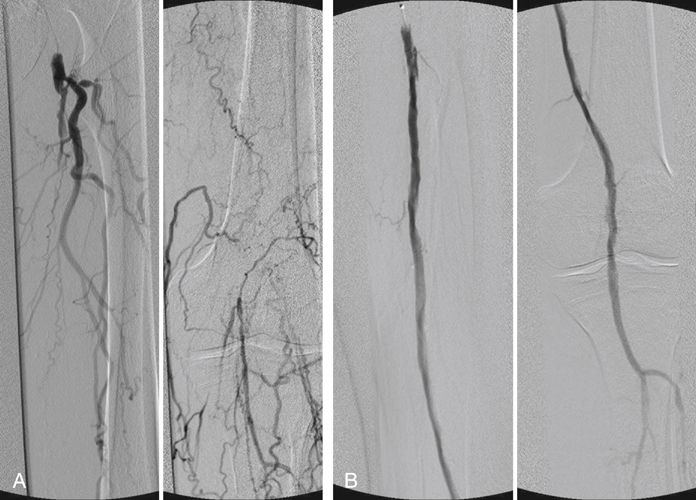
An appropriately sized balloon catheter can be used to dilate the channel with rapid segmental inflations from distal to proximal once the wire has traversed through the subintimal plane, along the occlusion, and back into the true lumen below the occlusion. After angioplasty, angiography is performed to document the characteristic appearances of a subintimal recanalization (Figures 1 and 2). Radiographic appearances demonstrate a very irregular channel. However, the most important characteristic of the angiogram is velocity of flow. Fast flow is the hallmark of a successful recanalization.
Subintimal Recanalization for Lower Limb Occlusive Disease
Technique
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Thoracic Key
Fastest Thoracic Insight Engine