The national observational study of diagnostic and interventional cardiac catheterization (ONACI) is a prospective multicenter registry of the French Society of Cardiology including all interventional cardiology procedures performed from 2004. We aimed to evaluate “real-world” management of patients with coronary artery disease in France from this registry. The present study was focused on data collected from 2004 to 2008. Patient demographics and co-morbidities, invasive parameters, treatment options, and procedural techniques were prospectively collected. Patients were recruited from 99 hospitals (55% of patients were hospitalized in private clinics and 45% in public institutions). During a 5-year period, a total of 298,105 patients underwent coronary angiography and 176,166 patients underwent percutaneous coronary intervention. Diagnosis was acute coronary syndrome in 22%, stable angina or silent ischemia in 23%, and atypical chest pain in 9% of cases. Normal coronary arteries or nonsignificant coronary narrowing were found in 26% of patients. Radial access was increasingly used over the years regardless of the indication. The average number of percutaneous coronary interventions per procedure was 1.5 ± 0.7 (range, 1.3 ± 0.7 to 1.5 ± 0.7) and that of stents per procedure was 1.5 ± 0.8 (range, 1.5 ± 0.8 to 1.6 ± 0.8). Drug-eluting stents were used in 45% (range, 34% to 62%), increasing from 2004 to 2006, and then decreasing after the 2006 controversy. In conclusion, ONACI is one of the largest catheterization registries during this period, providing a detailed and comprehensive global description of the spectrum and management of patients with suspected coronary artery disease undergoing cardiac catheterization.
The national observational study of diagnostic and interventional cardiac catheterization (ONACI) is a registry established in 2004 by the French Society of Cardiology to describe cardiovascular epidemiology and details of interventional cardiology practices in France. All procedures performed in France from 2004 at the participating institutions were recorded in this registry. The present study summarizes the main initial findings from the ONACI registry, characterizing the clinical and demographic characteristics of the patients, their management (including interventional procedures), and in-hospital outcomes.
Methods
ONACI is a national, prospective multicenter registry including most of the interventional cardiology procedures performed in France from 2004. Consecutive patients >18 years of age who underwent coronary angiography (CAG) and/or percutaneous coronary intervention (PCI) from 2004 are included. The present study was focused on data during a period of 5 years (from 2004 to 2008). Participation in the registry was on a voluntary basis, strongly encouraged by the French Society of Cardiology; it did not affect the therapeutic approach of cardiologists in any way.
Our population was divided into 2 groups: the first one including patients who underwent CAG (±PCI), analyzed to evaluate clinical characteristics and angiographic features and the second one including patients who underwent PCI (±CAG) used to assess procedural characteristics.
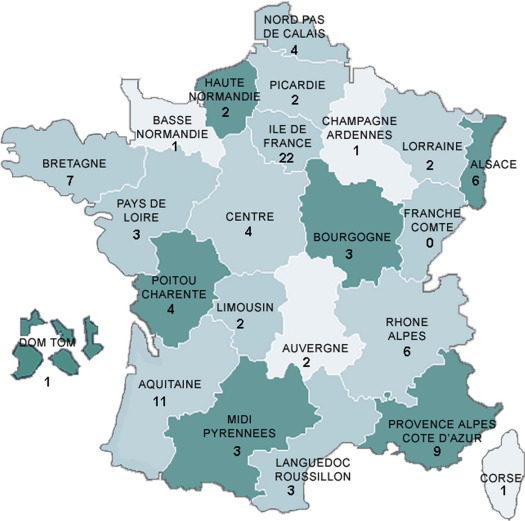
CAG and PCI were performed for 4 main indications: atypical chest pain, suspected stable angina or suspected silent ischemia, acute coronary syndromes (ACSs) at the acute stage, and recent myocardial infarction (MI, defined as MI <1 month, but beyond the acute stage). Suspected silent ischemia was defined before CAG, in the absence of anginal symptoms, when either an exercise test result was considered positive or an imaging stress test demonstrated reversible abnormalities suggestive of myocardial ischemia. Asymptomatic patients with a false-positive exercise test results may therefore have been included in this category. Other indications included arrhythmias, cardiomyopathy, cardiac arrest, and elective evaluation before surgery. Participation in the study was offered to all French institutions, university hospitals, general and regional hospitals, and private clinics that could perform PCI. In each center, a physician was in charge of the registry and provided a full list of all patients admitted to his/her unit. Analyses according to the type of center and administrative regions were also performed to determine potential regional variations, possibly linked to the north-south gradient in prevalence of coronary artery disease (CAD) existing in France as in Europe. For this analysis, France was divided into 2 parts: a northern one (including the regions Alsace, Basse-Normandie, Bourgogne, Bretagne, Centre, Champagne Ardennes, Haute-Normandie, Ile de France, Lorraine, Nord Pas de Calais, Pays de la Loire, and Picardie) and a southern one (including Aquitaine, Auvergne, Corse, Languedoc-Roussillon, Limousin, Midi-Pyrénées, Poitou-Charentes, Provence-Alpes-Côte-d’Azur, and Rhône-Alpes). Data collection has been previously described in detail elsewhere. Data were entered in local electronic databases at each center by the physicians who performed the procedures, and data files were sent every 6 months to the French Society of Cardiology, where they were merged into a common database. The following data were prospectively collected and electronically stored for each patient: demographic characteristics (age, gender, and body mass index), cardiovascular risk factors (arterial hypertension, body mass index ≥30, diabetes, current smoking, and hyperlipidemia), and medical cardiovascular history (presence of previous acute MI, previous PCI, previous coronary artery bypass grafting, peripheral artery disease, and chronic kidney disease). Chronic kidney disease was defined as creatinine clearance <30 ml/mm or creatinine >15 mg/L. Left ventricular ejection fraction, assessed at entry or any time during the hospital stay, was recorded. Procedural information about the devices used and the vessels treated with angioplasty (e.g., number of lesions treated and number of stents implanted) was collected as previously described. Finally, in-hospital complications (death, stroke, MI, bleedings, and renal failure) occurring <24 hours of the procedures were recorded. Data were then checked for coherence and completeness by a cardiologist and a statistician (EP and MCP), and individual records with too many missing data (patients with >50% of data missing) were excluded from the present analysis.
The study was conducted in compliance with good clinical practice, French law, and the French data protection law. The protocol was reviewed by the Committee for the Protection of Human Subjects in Biomedical Research of Saint-Antoine University Hospital. Data file of the ONACI registry was declared to and authorized by the French data protection committee (Commission Nationale Informatique et Liberté). Statistical analysis was performed using SPSS 18.0 software (SPSS Inc., Chicago, Illinois). For quantitative variables, means, SDs, and minimum and maximum values were calculated. In addition, medians with the interquartile range were calculated for some of the variables. Discrete variables are presented as percentages. Comparisons were made with chi-square tests or Fisher’s exact tests for discrete variables and with unpaired t tests, Wilcoxon signed-rank tests, or 1-way analyses of variance for continuous variables. For all analyses, a p value <0.05 was considered significant.
Results
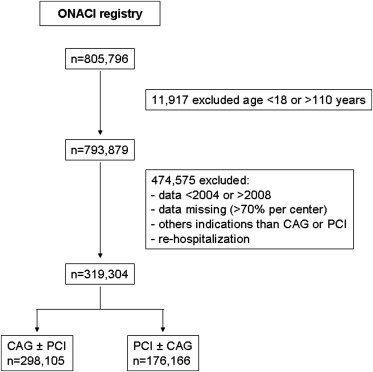
During a 5-year period, a total of 298,105 patients were included in the registry for CAG and 176,166 patients for PCI ( Figure 1 ). Patients were enrolled in 99 hospitals: 19 university hospitals, 30 public nonacademic hospitals, and 50 private clinics. The recruitment of patients according to French administrative regions is shown in Figure 2 . All regions were represented except Franche-Comté. Fifty-five percent of patients were hospitalized in private clinics and 45% in public institutions, which included university hospitals (25%) and public nonacademic hospitals (20%).
Baseline clinical characteristics of patients hospitalized for CAG are listed in Table 1 . CAG was indicated for suspected stable angina or silent ischemia in 23% of the patients, and stress tests had been performed before CAG in 75% of them; the stress test result was considered positive in 70% of the cases. ACS (22%) and recent MI (3%) represented the second most common indication for CAG. Of the patients presenting with ACS, 40% were admitted for unstable angina, 31% for ST elevation MI, and 29% for non–ST elevation MI. CAG was performed for atypical chest pain in 9% of the patients, of whom 61% had undergone a stress test before catheterization (with a positive test result in 50%). The other indications were arrhythmias (n = 2,063, 0.7%), cardiomyopathy (n = 6,691, 2.2%), cardiac arrest (n = 1,281, 0.4%), elective evaluation before cardiac surgery (n = 9,746, 3.3%), and other screenings for CAD (n = 18,026, 6.1%). The stress tests had been performed in 28% of these patients and were considered positive in only 24%. A total of 30.9% of indications were undefined.
| Variable | SA/SI (n = 69,187) | Atypical Chest Pain (n = 25,893) | ACS (n = 64,932) | Recent MI (n = 8,078) | Others ∗ (n = 37,807) | All (n = 298,105) | p |
|---|---|---|---|---|---|---|---|
| Age (yrs) | 66.6 ± 10.7 | 63.5 ± 12.3 | 65.67 ± 13.3 | 66.1 ± 13.2 | 66.4 ± 12.1 | 65.9 ± 12.2 | <0.001 |
| Men | 53,245 (77) | 16,625 (64) | 47,628 (73) | 5,917 (73) | 27,251 (72) | 219,545 (74) | <0.001 |
| BMI (kg/m²) | 27.3 ± 4.4 | 27.3 ± 4.9 | 26.9 ± 4.5 | 26.7 ± 4.5 | 27.0 ± 4.9 | 27.1 ± 4.6 | <0.001 |
| Ejection fraction | 62 ± 12 | 63 ± 12 | 58 ± 12.9 | 52 ± 13 | 56 ± 16 | 59 ± 14 | <0.001 |
| Family history | 15,361 (22) | 5,866 (23) | 13,207 (20) | 1,524 (19) | 5,297 (15) | 48,400 (21) | <0.001 |
| Previous MI | 11,115 (16) | 2,709 (11) | 8,163 (13) | 875 (11) | 2,964 (8) | 32,819 (14) | <0.001 |
| Previous PCI | 19,319 (28) | 5,075 (20) | 12,704 (20) | 620 (8) | 3,827 (10) | 52,050 (21) | <0.001 |
| Previous CABG | 6,075 (9) | 1,059 (5) | 3,842 (6) | 166 (2) | 1,523 (4) | 15,905 (6) | <0.001 |
| Peripheral vascular disease | 8,243 (12) | 1,753 (7) | 5,444 (8) | 492 (6) | 4,044 (11) | 25,322 (10) | <0.001 |
| Chronic kidney disease † | 3,382 (5) | 860 (3) | 3,626 (6) | 424 (5) | 2,042 (6) | 13,844 (6) | <0.001 |
| Smoker | 27,598 (40) | 9,970 (39) | 28,610 (44) | 3,415 (42) | 11,505 (31) | 100,872 (41) | <0.001 |
| Diabetes mellitus | 19,294 (28) | 5,022 (19) | 13,119 (20) | 1,549 (19) | 7,278 (20) | 56,708 (23) | <0.001 |
| Hypertension | 40,716 (59) | 13,589 (53) | 32,930 (51) | 3,505 (43) | 17,978 (48) | 133,045 (54) | <0.001 |
| Hyperlipidemia | 42,524 (62) | 13,396 (52) | 33,339 (51) | 3,701 (46) | 15,293 (41) | 132,003 (53) | <0.001 |
∗ Arrhythmias, cardiomyopathy, cardiac arrest, and elective evaluation before surgery.
† Defined as creatinine clearance <30 ml/min or creatinine >15 mg/L.
Of the patients with a positive stress test result, 56% were subsequently treated with PCI, 37% with medical therapy only, and 7% with coronary artery bypass grafting.
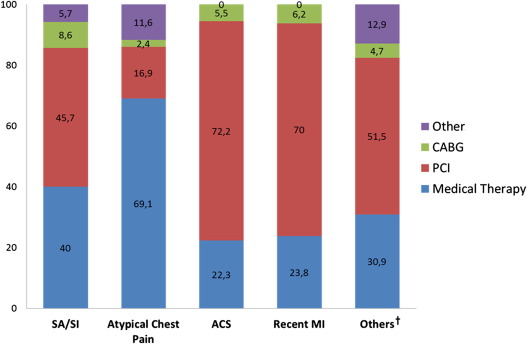
The results of CAG are listed in Table 2 . We found normal coronary arteries or nonsignificant coronary lesions (<50% of diameter stenosis) in 26% of patients (range 6% to 60% according to the indications). Patients presenting with atypical chest pain and patients hospitalized for CAD screening frequently had a 1-vessel disease. Patients presenting with ACS, as expected, had more severe and diffuse coronary disease. The choice of the treatment depends on the indications for CAG ( Figure 3 ).
| SA/SI, n = 69,187 (%) | Atypical Chest Pain, n = 25,893 (%) | ACS, n = 64,932 (%) | Recent MI, n = 8,078 (%) | Others, ∗ n = 37,807 (%) | All, n = 298,105 (%) | p | |
|---|---|---|---|---|---|---|---|
| No significant lesion † | 15,289 (22) | 15,455 (60) | 7,018 (11) | 520 (6) | 20,931 (55) | 77,731 (26) | <0.001 |
| Significant lesion | |||||||
| 1-Vessel disease | 18,424 (27) | 4,789 (19) | 21,098 (33) | 2,826 (35) | 6,866 (18) | 80,106 (27) | |
| 2-Vessel disease | 17,630 (25) | 3,153 (12) | 19,028 (29) | 2,496 (31) | 5,275 (14) | 71,976 (24) | |
| 3-Vessel disease | 17,844 (26) | 2,496 (9) | 17,786 (27) | 2,235 (28) | 4,733 (13) | 68,292 (23) | |
| LMCA | 4,298 (7) | 525 (2) | 3,629 (6) | 277 (4) | 1,200 (3) | 3,491 (2) | |
∗ Arrhythmias, cardiomyopathy, cardiac arrest, and elective evaluation before surgery.
Baseline procedural features are summarized in Supplementary File 1 . Radial access was used as often as femoral access; in patients with ST elevation MI, however, femoral access was used more often (56%). The most frequently used sheath sizes were 6 and 5 Fr. The average number of PCIs per procedure was 1.5 ± 0.7 (range, 1.3 ± 0.7 to 1.5 ± 0.7) and that of stents per procedure was 1.5 ± 0.8 (range, 1.5 ± 0.8 to 1.6 ± 0.8). Drug-eluting stents (DESs) were used in 45% (range, 34% to 62%).
Clinical outcomes during the first 24 hours are listed in Table 3 . Overall, clinical outcomes depended on the indication of the procedure. Patients with ACS (or recent MI) had significantly more complications (death, nonfatal MI, stroke, or urgent revascularization) than those with stable angina or atypical chest pain. PCI success was obtained in 96.9% (range, 95.7% to 97.2%, depending on the indication).
| SA/SI, n = 37,752 (%) | Atypical Chest Pain, n = 4,359 (%) | ACS, n = 48,904 (%) | Recent MI, n = 6,239 (%) | Others, ∗ n = 6,672 (%) | All, n = 176,166 (%) | p | |
|---|---|---|---|---|---|---|---|
| Angiographic success | 97 | 97 | 97 | 96 | 97 | 97 | <0.001 |
| No adverse events † | 37,565 (99.5) | 4,345 (99.7) | 48,091 (98.3) | 6,137 (98.4) | 6,482 (97.2) | 173,429 (98.5) | <0.001 |
| Death | 48 (0.1) | 3 (0.1) | 420 (0.9) | 46 (0.7) | 154 (2.3) | 783 (0.5) | <0.001 |
| Nonfatal MI | 90 (0.2) | 5 (0.1) | 212 (0.4) | 37 (0.6) | 32 (0.5) | 434 (0.2) | <0.001 |
| Urgent revascularization | <0.001 | ||||||
| CABG | 6 (0) | 1 (0) | 16 (0) | 1 (0) | 0 (0) | 29 (0) | |
| PCI | 17 (0) | 4 (0.1) | 43 (0.1) | 13 (0.2) | 4 (0.1) | 91 (0.1) | |
| Stroke | 12 (0) | 2 (0) | 42 (0.1) | 7 (0.1) | 3 (0) | 81 (0) | <0.001 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


