Stridor
Christopher M. Walker, MD
DIFFERENTIAL DIAGNOSIS
Common
Tracheobronchomalacia
Saber-Sheath Trachea
Laryngeal/Pharyngeal Tumor
Thyroid Mass
Less Common
Trauma
Tracheal Stenosis
Foreign Body
Wegener Granulomatosis
Rare but Important
Tracheopathia Osteochondroplastica
Infection
Tracheal Neoplasm
Tracheobronchial Amyloidosis
Relapsing Polychondritis
ESSENTIAL INFORMATION
Key Differential Diagnosis Issues
Review focuses on stridor in adults
Stridor
High pitched sound secondary to turbulent flow in upper airway
Indicates pathology in trachea or larynx
Radiography and CT
Primary imaging modalities used in directing differential diagnosis
Final diagnosis may require bronchoscopy with biopsy
Helpful Clues for Common Diagnoses
Tracheobronchomalacia
Abnormal tracheal or bronchial cartilage
≥50% decrease in cross-sectional area with expiration
Trachea may appear normal on inspiratory images
Congenital or acquired causes secondary to
Intubation, external mass or vessel causing compression, infections, or COPD
Saber-Sheath Trachea
Strong association with COPD
Cartilage damage through repeated coughing
Coronal tracheal diameter ≤2/3 sagittal diameter
Normal tracheal wall thickness
Laryngeal/Pharyngeal Tumor
Squamous cell carcinoma most common etiology
Document extent of disease, as it influences surgical and therapeutic plan
Thyroid Mass
Goiter or malignancy may externally compress trachea
Helpful Clues for Less Common Diagnoses
Trauma
Hematoma compressing airway
Secondary tracheal stenosis from remote trauma
Tracheal Stenosis
Focal stricture with circumferential wall thickening
± cartilage damage with resulting tracheomalacia
Prolonged endotracheal intubation
Subglottic tracheal stenosis at cuff site
Reduced incidence with low-pressure balloon cuffs
Tracheostomy tube placement
Stenosis at stoma site
Other etiologies
Complete cartilaginous tracheal ring and sarcoidosis
Treat with mechanical dilation or stenting
Foreign Body
History essential for diagnosis
Foreign body rarely radiopaque
Wegener Granulomatosis
Circumferential subglottic tracheal wall thickening with luminal narrowing
± cavitary lung nodules
± pansinus disease
Laboratory evidence of glomerulonephritis (microscopic hematuria and proteinuria)
Helpful Clues for Rare Diagnoses
Tracheopathia Osteochondroplastica
Benign disease occurring in older men
Often incidental at bronchoscopy
Rarely leads to symptoms
Small and irregularly shaped calcified nodules arising from cartilage
Spares noncartilaginous posterior tracheal membrane
Infection
Tuberculosis
Epiglottitis
More indolent than pediatric epiglottitis, secondary to larger hypopharynx
Rhinoscleroma
Chronic granulomatous infection by Klebsiella rhinoscleromatis
Central America, Africa, and India
Nasal cavity involved in 95% with polyps and soft tissue thickening
Spares paranasal sinuses
25% have subglottic tracheal involvement with concentric or nodular narrowing
Air-filled crypts in tracheal lumen nearly diagnostic
Tracheal Neoplasm
3 different forms
Primary malignant, metastatic disease, and primary benign tumors
3 growth patterns
Sessile, polypoid, and circumferential growth
CT documents extent of disease and trachea distal to lesion
Squamous cell carcinoma
Most common primary malignant disease of trachea
Strong association with smoking
10% multifocal at presentation
Adenoid cystic carcinoma
Posterolateral tracheal wall
± growth along airways
Metastatic disease
Invasion or compression from bronchogenic or esophageal carcinoma
Hematogenous metastases from melanoma, breast, colon, and renal cell carcinoma
± single or multiple endotracheal lesions
Tracheobronchial papillomatosis
HPV infection of tracheal and bronchial tree
Small well-circumscribed noncalcified tracheal nodules
± cystic lung lesions
Tracheobronchial Amyloidosis
Nodular or concentric wall thickening of trachea and mainstem bronchi
± nodular calcification
± atelectasis or lobar collapse
Usually no lung nodules
Treatment with stenting or resection
Relapsing Polychondritis
Systemic disorder associated with repeated bouts of cartilaginous inflammation
Trachea and bronchi affected late in disease course
Also affects cartilage of
Ears, nose, and joints
CT shows
Tracheobronchial wall thickening with sparing of noncartilaginous posterior wall
Severe disease may affect posterior wall
Stenosis leads to recurrent pneumonia
Treat with stents and corticosteroids
Image Gallery
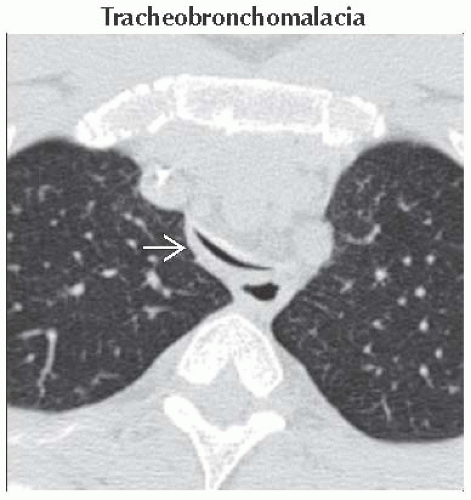 Axial NECT shows diffuse intrathoracic tracheal narrowing
 with more than 50% reduction in cross-sectional area when compared to inspiratory images, which is diagnostic of tracheomalacia. with more than 50% reduction in cross-sectional area when compared to inspiratory images, which is diagnostic of tracheomalacia.Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|