7 Stress Testing and Nuclear Imaging
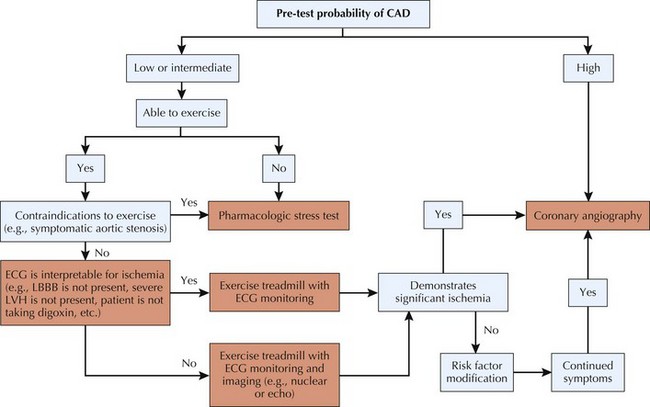
Stress electrocardiography and stress imaging studies are widely used noninvasive procedures that provide important information on cardiac function and the presence of hemodynamically significant coronary artery disease (CAD). The correct use of stress testing is critically important in the cost-effective management of patients with known or suspected CAD. When the most appropriate procedure is performed, it provides important diagnostic and prognostic information that determines the optimal management strategy to be undertaken for that individual. Stress testing is also used in patients with known CAD so as to determine exercise “prescriptions” before cardiac rehabilitation (Fig. 7-1).
Exercise Stress Testing
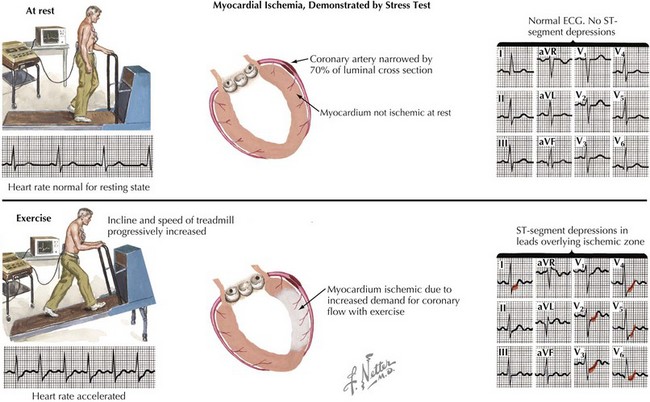
At the end of exercise testing, the patient slowly reduces the intensity of exercise. Vigorous exercise results in increased blood flow and pooling in the extremities, and a “step-down” phase (low-level exercise) allows the patient to re-equilibrate before ceasing exercise. After exercise termination, patients are monitored in a supine position until they are no longer tachycardiac (i.e., HR < 100 bpm) if not back to baseline HR. Importantly, if there were any ECG changes or symptoms experienced by the patient during the study, post-test monitoring should be continued with any necessary treatments until these have resolved, even if hemodynamics (HR and blood pressure) have returned to acceptable levels. The post-test monitoring serves to reveal any arrhythmias or ST-segment changes that may develop and be late signs of ischemic disease (Fig. 7-2).