Chapter 12 Stent Insertion for Diffuse Circumferential Tracheobronchomalacia Caused by Relapsing Polychondritis
Case Description
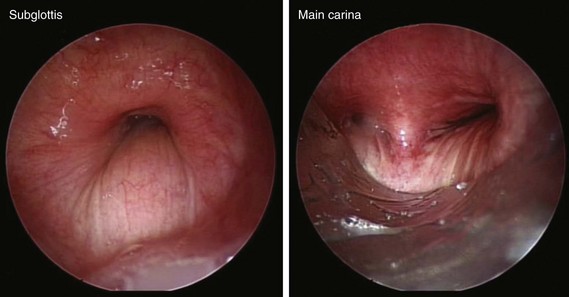
The patient was a 58-year-old woman who had respiratory arrest while playing golf. She was intubated by paramedics and was brought to the hospital, where she was found to be in hypercapnic respiratory failure despite being mechanically ventilated. Arterial blood gas analysis showed the following: pH 7.16/PCO2 70 mm Hg/PaO2 300 mm Hg/HCO3 24 mm Hg, consistent with acute respiratory acidosis. Peak airway pressures were consistently high (≈60 cm H2O), but plateau pressure was normal on mechanical ventilation in assist control volume control mode: TV 500 mL, RR 16, PEEP 5 cm H2O, and FiO2 of 1. According to her husband, shortness of breath and wheezing several days earlier had prompted a visit to the emergency department at an outside hospital. There, she was treated with systemic corticosteroids. Apparently her symptoms improved quickly, and she was discharged home within 48 hours. She had in fact been diagnosed with adult-onset asthma several years ago, for which she was taking albuterol inhalers as needed, fluticasone/salmeterol, Singulair, and prednisone 10 mg every other day. Several months before this admission, however, the patient had developed stridor. A working diagnosis of relapsing polychondritis was made on the basis of tracheal wall thickening noted on computed tomography of her neck. Her past medical history included a nonmalignant thyroid goiter, which had been removed because it was presumptively contributing to her shortness of breath. She had an office job, had never smoked, and had no occupational exposure to toxins or fumes. Her basic metabolic panel and electrocardiogram were normal. Complete blood count revealed hemoglobin of 10.5 g/dL. On arrival, flexible bronchoscopy showed complete collapse of the airway distal to the No. 7 endotracheal tube. Emergent rigid bronchoscopy showed a severe subglottic stricture and diffuse collapse of the entire cartilaginous structure from the subglottis to the distal mainstem bronchi (Figure 12-1).
Discussion Points
1. Describe the relationship between airway stents and respiratory tract infections.
2. Describe two strategies used to prevent stent-related infections and mucus plugging.
3. Describe two alternative treatments to silicone stent insertion in patients with tracheobronchomalacia resulting from relapsing polychondritis.
Case Resolution
Initial Evaluations
Physical Examination, Complementary Tests, and Functional Status Assessment
This patient had bronchoscopic evidence of diffuse collapse of the cartilaginous wall of the trachea and mainstem bronchi with sparing of the posterior membrane—findings consistent with a diagnosis of circumferential tracheobronchomalacia (TBM), and classic for relapsing polychondritis (RP). RP is a multisystem disease,* and it is incapacitating and life threatening because of its airway involvement.1 Auricular chondritis, the most common initial presentation, is seen in 85% to 95% of patients with RP. This patient, however, had no evidence of RP in the eyes, nose, or external ears. Isolated pulmonary presentation, as seen in this case, is not that unusual, and because of its often episodic nature, may result in a significant delay in diagnosis. In a review of 66 patients, the elapsed time from patient presentation for medical care for RP-related symptoms† to diagnosis was reportedly 2.9 years.1 In a small case series of five patients with RP and severe airway involvement requiring stent insertion, all patients were given the diagnosis of asthma before RP was diagnosed.2
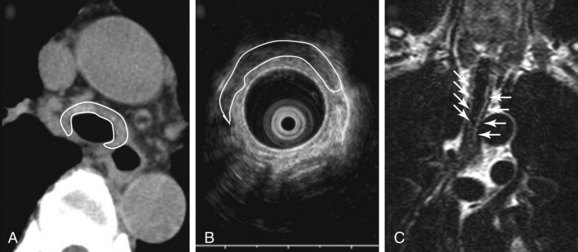
Malacia, identified as loss of supportive cartilaginous structures, is a chronic consequence of RP and is probably due to recurrent extensive inflammation. It may be asymptomatic in earlier stages and detected only on pulmonary function testing, but it becomes symptomatic when it involves the upper airways.3 Similar to this case, dynamic tracheal collapse might occur suddenly, causing dyspnea, respiratory arrest, and death.4 On histology, the airway cartilage shows empty lacunae (empty spaces within the cartilage), a mixed population of inflammatory cells,5 and abundant inflammatory exudates that are often noted to invade the periphery of necrotic cartilaginous tissues. An immunologic mechanism is likely responsible for this disease because RP is often associated with rheumatic or autoimmune disease, although the presence of autoantibodies* is inconsistent. Various studies have found circulating antibodies to cartilage-specific collagen types II, IX, and XI to be present in 30% to 70% of patients with RP, with antibodies to type II collagen† noted and correlating with the severity of acute RP episodes.6 Airway wall structural abnormalities in RP are detected by histopathology but can be identified using high-frequency (20 MHz) radial probe endobronchial ultrasonography (EBUS).7 EBUS reveals thickened and irregular cartilage, but the posterior membrane is normal (Figure 12-2).8 A definitive diagnosis of RP usually is based on the following criteria set by MacAdam et al.*5 and Damiani and Levine†9: (1) bilateral auricular chondritis; (2) nonerosive seronegative inflammatory polyarthritis; (3) nasal chondritis; (4) ocular inflammation; (5) respiratory tract chondritis; and (6) audiovestibular damage.
In one case series, the tracheobronchial tree was involved in about 56% of patients, and respiratory symptoms were responsible for the initial presentation in about 14%.5 In a larger case series of 145 patients suffering from RP, 31 patients had airway involvement, making the prevalence 21%.10 In many of these patients, similar to our patient, complaints of respiratory symptoms led to the diagnosis of RP, underscoring the fact that clinically significant airway compromise does not necessarily present late in the course of the disease. RP-related airway disease is more common among women and in patients between 11 and 61 years of age (median age, 42 years) at the time of first symptoms.* In this particular study, respiratory symptoms were the first manifestation of disease in 17 patients (54%), and dyspnea was the most common symptom in 20 patients (64%), followed by cough, stridor, and hoarseness. Airway involvement in remaining patients included subglottic stenosis (n = 8; 26%), focal and diffuse malacia (n = 15; 48%), and focal stenosis in different areas of the bronchial tree.10
In addition to a thorough review of systems during initial evaluation of a patient suffering from this disease, the treating team should set up realistic expectations, because it is known that the 5 year survival rate associated with RP is reported to be 66% to 74% but could be as low as 45% if RP occurs with systemic vasculitis. Other studies report a survival rate of 94% at 8 years, but these data may represent RP in patients with less severe disease than was observed in patients studied in earlier reports.1
Dynamic (aka functional) bronchoscopy with dynamic breathing and coughing maneuvers is usually performed to visualize and quantify the airway collapse when patients are evaluated for TBM. The degree of dynamic collapse is estimated by visual inspection but can be objectively quantified using morphometric bronchoscopy.† If TBM is present, the amount of collapse during passive and forced exhalation, as well as cough, is documented. In our case, complete collapse was clearly seen on bronchoscopy, making other quantifying methods unnecessary (see Figure 12-1).
Paired inspiratory/expiratory dynamic computed tomography (CT) scanning can reveal the degree, and potentially the cause, of expiratory central airway collapse.11 The boundary between normal physiologic dynamic airway compression and abnormal collapse is far from established, however, and disagreement continues regarding how much of a decrease in cross-sectional area actually signals clinically and physiologically significant airway narrowing.12 Although many investigators use 50% or greater reduction in airway cross-sectional area between inspiration and expiration to identify malacia, recent studies suggest that this definition leads to overdiagnosis, given that 78% of normal people reportedly exceed this criterion.13 However, it is noteworthy that in RP, thickened airway wall is noted, and even during inspiration, the lumen caliber is not normal (Figure 12-3) (see video on ExpertConsult.com) (Video III.12.1![]() ). In view of this, the use of absolute cutoff values to define abnormal collapse is less relevant, and what matters most when evaluating these patients is the impact on flow dynamics and symptoms. One disadvantage of dynamic CT scanning is that expiratory images can be technically unsatisfactory when patients are unable to cooperate with dynamic breathing instructions, thus failing to coordinate breathing with the timing of the scan. This is particularly the case in patients with respiratory distress or respiratory failure on mechanical ventilation. In these cases, CT is inadequate to evaluate for malacia.12 Given our patient’s unstable respiratory status, CT scanning was not performed preoperatively.
). In view of this, the use of absolute cutoff values to define abnormal collapse is less relevant, and what matters most when evaluating these patients is the impact on flow dynamics and symptoms. One disadvantage of dynamic CT scanning is that expiratory images can be technically unsatisfactory when patients are unable to cooperate with dynamic breathing instructions, thus failing to coordinate breathing with the timing of the scan. This is particularly the case in patients with respiratory distress or respiratory failure on mechanical ventilation. In these cases, CT is inadequate to evaluate for malacia.12 Given our patient’s unstable respiratory status, CT scanning was not performed preoperatively.
When feasible, however, CT should be performed and may show tracheobronchial wall thickening (see Figure 12-2) with or without calcification (seen in ≈40 % of patients). These findings are not very sensitive (seen in 17 of 30 patients in one study); however, all patients will have sparing of the posterior membrane—a characteristic finding in RP.10 CT may also reveal varying degrees of tracheal narrowing, often involving multiple segments of the trachea. In addition to its ability to reveal malacia, expiratory images may reveal consequent air trapping. The CT scan is also sensitive in detecting lower airway disease manifested by concentric narrowing in lobar and segmental bronchi and subsegmental bronchi.14 Dynamic CT scanning should be done according to the institution’s central airways CT investigation protocol, usually without intravenous contrast administration. Images are initially obtained using a standard radiation dose technique at end inspiration (170 mAs, 120 kVp, 2.5 mm collimation, high-speed mode, and pitch equivalent of 1.5). This is followed by a low-dose examination (40 mAs, 120 kVp, 2.5 mm collimation, high-speed mode, and pitch equivalent of 1.5) during the dynamic expiratory phase of respiration. Axial CT data are subsequently used to create a series of multiplanar and three-dimensional (3D) images, which are reviewed in conjunction with the axial images.
Magnetic resonance imaging (MRI) is also a useful adjunct in clinical diagnosis. MRI is better than CT in distinguishing between edema, fibrosis, and inflammation. T1-weighted images, T2-weighted images (see Figure 12-2), and T1-weighted images with gadolinium contrast provide characterization of relapsing polychondritis-related changes in cartilaginous tissues. MRI may be useful in detecting other potential RP-related problems such as thickening of the thoracic aorta before dilation occurs. Because of its lack of ionizing radiation, MRI may be a useful noninvasive test for monitoring the effects of treatment.
Pulmonary function testing (PFT) with flow-volume loop studies were not feasible in our patient but are recommended in patients with RP who present with respiratory symptoms. PFTs may assist in differential diagnoses and provide information about the severity of airway obstruction. PFTs can also be used to monitor disease activity. PFTs in patients with RP who have respiratory involvement demonstrate a nonreversible obstructive pattern with the decrease in forced expiratory volume in 1 second correlating with the degree of dyspnea.15 In general, both in normal people and in patients with obstructive ventilatory impairment, the flow-limiting segment, called the choke point, tends to be located in a region of minimum cross-sectional area and minimum side pressure within the airway when maximal flow is reached.16 Because maximum expiratory flow is airway compliance dependent, increased compliance, as is seen in patients with TBM, results in increased airway resistance and decreased maximum expiratory flow. Studies of airflow limitation in experimental models demonstrate that when the collapsing trachea is supported by a rigid tube, airflow improves and the flow-limiting segment migrates from the central airway toward the periphery.17
In this regard, studies in patients with RP have evaluated dynamic intrathoracic obstruction using a combination of physiologic and imaging modalities consisting of PFT, airway measurements with 3D-CT, and radial probe EBUS. To properly assess the location of the choke point, investigators measured intra-airway pressure and cross-sectional areas of the airway from bronchi to trachea.18 For seven patients who underwent self-expandable metallic stent insertion, choke points were detected in the trachea, mainstem bronchi, or lobar bronchi. After stent insertion, the flow-volume curves displayed significant improvements in flow limitation. Intraluminal catheter measurements of pressure differences decreased significantly, suggesting that stents had been inserted appropriately at the flow-limiting segments. Expiratory CT scanning revealed mosaic patterns, indicating air trapping due to migration of the choke points to smaller bronchi, as had been demonstrated in previous experimental studies.17,18
Comorbidities
This patient had no evidence of other organ involvement from RP. The clinical relevance of RP is not limited to airflow obstruction but extends to other systems and may include heart block and vasculitis of both small and larger vessels. Making a prompt diagnosis of heart involvement is essential, especially if patients are scheduled to undergo general anesthesia.19 The cardiovascular system is reportedly affected in 24% of patients with RP. When possible, a thorough history and physical examination should be performed to evaluate for chest pain, abdominal pain, history of pericarditis, abnormal heart rate or rhythm, syncope, and history of subacute myocardial infarction (found on electrocardiogram [ECG]). Aortic and mitral valve regurgitation, aortic aneurysm, aortitis, aortic thrombosis, pericarditis, first- to third-degree heart block, and myocardial infarction, at times mediated through ostial stenosis of a coronary artery or arteries, have been reported.20 Furthermore, although the life expectancy in all patients with RP is decreased compared with age- and sex-matched healthy individuals, patients with RP and renal involvement have a significantly lower age-adjusted life expectancy. Among those with renal disease (glomerulonephritis* diagnosed on the basis of a diagnostic renal biopsy or the presence of microhematuria and proteinuria), uremia is a common cause of death.21
A high prevalence of other autoimmune disorders has been found in patients with RP. These may include systemic vasculitis (≈13%), cutaneous leukocytoclastic vasculitis (≈7%), thyroid disease (≈6%), rheumatoid arthritis (≈5%), and systemic lupus erythematosus (≈4%).20 Association with complex immunologic conditions such as a combination of Crohn’s disease (≈2%), ulcerative colitis (≈2%), and epidermolysis bullosa acquisita has also been described.22
Support System
The husband was very supportive. He requested more information about her diagnosis and searched Internet support sites for patients with RP and their families. Although we do not take responsibility for quality, the website from the Relapsing Polychondritis Support and Awareness Foundation may be helpful.23
Procedural Strategies
Expected Results
Study results show that many patients with severe TBM requiring airway stabilization who are not surgical candidates can benefit immediately from airway stent insertion in terms of improvement in functional status, decreased extent of airway narrowing, and reduced severity of airway collapse.24 In one series, adverse effects from silicone stent insertion were very common; however, a total of 26 stent-related adverse events were noted in 10 of 12 patients (83%) a median of 29 days after intervention, including 6 cases of granulation tissue formation, 8 stent migrations, and 12 cases of partial obstruction from mucus plugs. Five emergent flexible bronchoscopies were necessary, of which 1 prompted an emergent rigid bronchoscopy to manage granulation tissue and post obstructive pneumonia; the other 4 emergent flexible bronchoscopies were done to remove mucus plugging. Six rigid bronchoscopies were performed emergently because of new respiratory symptoms.24 In a different series evaluating only patients with RP and airway involvement, 12 patients (40%) required intervention, including balloon dilation alone (n = 5), stent placement (n = 3), tracheotomy (n = 1), balloon dilation with stent insertion (n = 1), balloon dilation with tracheostomy (n = 1), and tracheostomy with stent insertion (n = 1). Most patients experienced improvement in airway symptoms after intervention, although 1 patient died of progression of airway disease during the follow-up period.10 Most of the patients treated in this study had stenosis, not malacia; in fact, of 8 patients with bronchoscopically detected TBM in the study, only 3 were treated (2 by stent insertion and 1 by tracheostomy and removal of previously placed stents).10
Therapeutic Alternatives
As of this writing, no medical, minimally invasive, or surgical treatment that cures RP is available, especially once cartilage destruction and malacia are established. Stents are reserved for patients with airway involvement (stenosis or malacia) and severe functional impairment.2 In milder forms of airway involvement, treatment should be optimized before invasive therapies are considered. Continuous prednisone therapy has been shown to decrease the severity, frequency, and duration of relapses but does not stop disease progression.5 Prednisone (20 to 60 mg/day) is administered in the acute phase and is tapered to 5 to 25 mg/day for maintenance. Severe relapses may require 80 to 100 mg/day.5 Newer immunomodulating agents such as tumor necrosis factor receptor blockers may have a role in treating the inflammatory destruction of cartilaginous structures and can also be used as steroid-sparing agents.25 Despite aggressive medical therapy (prednisone, mycophenolate mofetil, etanercept, and methotrexate), many patients experience symptom progression warranting invasive interventions.
1. Tracheostomy: may not fully palliate airway collapse owing to malacia of the more distal airways beyond the tracheotomy site.26,27 Tracheostomy is useful when it stents or bypasses the malacic airway or a subglottic stenosis, as is noted in this video from a different patient with RP and subglottic stenosis (see video on ExpertConsult.com) (Video III.12.2![]() ); tracheostomy also allows invasive ventilatory support when necessary and offers a secured airway in cases of acute airway obstruction.12 However, tracheostomy can be complicated by secondary tracheomalacia and stenosis at the stoma site.28 From a physiologic standpoint, tracheostomy may be inadequate and may exacerbate diffuse malacia because it bypasses the physiologic function of the glottis to maintain positive transmural pressure that keeps the airway lumen patent.12
); tracheostomy also allows invasive ventilatory support when necessary and offers a secured airway in cases of acute airway obstruction.12 However, tracheostomy can be complicated by secondary tracheomalacia and stenosis at the stoma site.28 From a physiologic standpoint, tracheostomy may be inadequate and may exacerbate diffuse malacia because it bypasses the physiologic function of the glottis to maintain positive transmural pressure that keeps the airway lumen patent.12
2. Membranous tracheoplasty: not an option for patients with true malacia from cartilaginous destruction24; surgical cases of tracheoplasty excluded RP. In the largest case series reported of patients with RP and airway involvement, none of the 30 patients underwent tracheoplasty.10 This procedure is advocated for some patients with tracheomalacia. The procedure attempts to restore a normal anatomic configuration of the airway, so that cartilaginous structures are brought into a more normal C shape from their flattened pattern.29 This procedure is associated with significant complications* and does not apply to patients with circumferential diffuse TBM from RP, but only to carefully selected patients with crescent-type TBM.30
3. Other surgical interventions: External airway splinting using other tissues of the body or Gore-Tex (A. L. Gore, Flagstaff, Ariz) reportedly prevents collapse in cases of severe upper airway disease.27 The success of laryngotracheal reconstruction has been anecdotally reported when tracheal or subglottic stenosis occurs in isolated segments.31
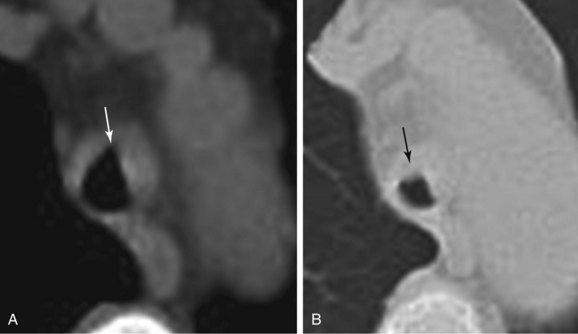
4. Other types of straight airway stents (Figure 12-4): Proper sizing of the stent (length and diameter) in relation to the dimensions of the trachea or bronchus is important to avoid stent-related complications such as migration, mucus plugging, granulation, and tumor ingrowth. Both self-expandable metallic stents and silicone stents have been used in patients with malacia from RP.2,4,18 Sometimes, more than one stent may be required if symptoms persist after stent insertion, presumably because of distally migrated choke points.18,32 With regard to stent selection for this disease, the bronchoscopist should consider the biomechanical properties of the airway stents: Silicone stents have excellent force compression characteristics and are readily removable in case of complications33; metal stents on the other hand, have been associated with severe complications including stent fracture, rupture, and excessive mucosal ingrowth and epithelialization in patients with malacia.34
5. The dynamic stent (Rusch Y stent, Rusch AG, Duluth, Ga) is a bifurcated silicone stent that is designed to simulate tracheal morphology: It is reinforced anteriorly by horseshoe-shaped metal rings that resemble tracheal cartilages and a soft posterior wall that behaves like the membranous trachea by allowing inward bulging during cough. Stent fracture from fatigue and retained secretions are rarely encountered,* and the stent is used for strictures of the trachea, main carina, and/or main bronchi; tracheobronchomalacia; tracheobronchomegaly with excessive dynamic airway collapse; and esophago-respiratory fistula.35
6. The Polyflex stent (Boston Scientific, Natick, Mass) is a self-expanding stent made of cross-woven polyester threads embedded in silicone. Its wall to inner diameter is thinner than that of Dumon (Novatech, Grasse, France) or Noppen (Reynder Medical Supplies, Lennik, Belgium) stents. Its expansile force is stronger than that seen with the Dumon or Ultraflex stent (Boston Scientific).36 This stent can be used to treat benign and malignant strictures, esophago-respiratory fistula, and tracheomalacia (Figure 12-5); stents of different lengths and diameters and tapered models are available for sealing stump fistulas. Incorporation of tungsten into the stent makes it radiopaque and easier to identify on chest radiograph. The stent’s outer surface, however, is smooth, which increases the risk for migration. In a small series of 12 patients in whom 16 Polyflex stents were used for benign airway disorders including TBM, the reported complication rate was 75% even though immediate palliation was achieved in most cases (90%). Stent migration was the most common complication that occurred between 24 hours and 7 months after deployment with all 4 patients with lung transplant–related anastomotic stenoses encountering complications: 2 had significant mucus plugging requiring emergent bronchoscopy, whereas the stents migrated in the other 2 patients.37
7. Laser treatment: Yttrium aluminum pevroskyte (YAP) laser treatment was anecdotally reported to improve lung function and symptoms in excessive dynamic airway collapse due to Mounier-Kuhn syndrome; this was done, however, with the intention of stiffening the posterior membrane by devascularization and subsequent retraction of tissues.38 The YAP laser has been used for treatment of a variety of disease processes involving the central airways. Its wavelength is double that of the yttrium aluminum garnet (YAG) laser, allowing for tissue devascularization and coagulation at low power (15 to 20 W) in a discontinuous mode.39 The depth of penetration using the YAP laser is estimated at 3 mm, and it may reach the submucosal tissues, triggering a retractile fibrotic process that rigidifies the posterior membrane. This effect has been studied in humans to reduce palatal flutter in an attempt to reduce snoring.40
8. Noninvasive positive-pressure ventilation can be used to maintain airway patency, facilitate secretion drainage, and improve expiratory flow. Continuous positive airway pressure (CPAP) acts as a pneumatic stent, decreases pulmonary resistance, and improves expiratory airflow obstruction. It has been used successfully in patients with tracheomalacia due to RP.41 The response to CPAP can be documented by performing CPAP-assisted bronchoscopy42 or CPAP-assisted computed tomography.43
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree