CHAPTER 3
Stage A: Patients at Risk for Developing Structural Heart Disease
“The superior physician prevents sickness.”
—Chinese proverb
Major Risk Factors and Increasing Prevalence of Heart Failure
Attention to the modifiable risk factors for heart failure, which are present in Stage A, may help reduce the increasing prevalence of heart failure as the population ages.
COMMON ETIOLOGIES OF HEART FAILURE
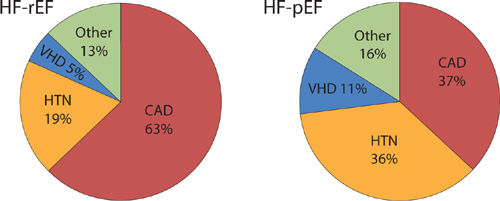
The Framingham Study prospectively determined the etiologies of heart failure in 534 patients (Figure 3.1).1 Overall, coronary artery disease was the most common principal cause of heart failure, even though hypertension was a frequent comorbidity.
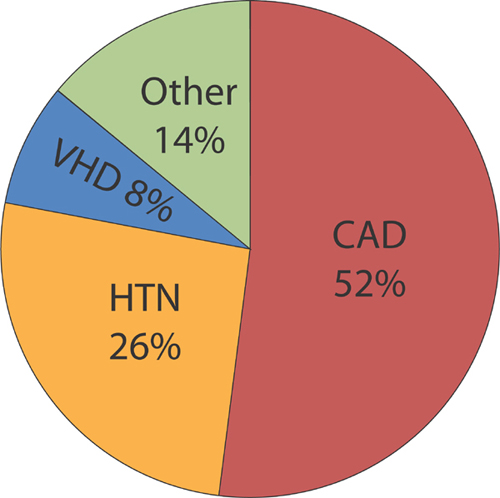
FIGURE 3.1 Primary etiology of heart failure. Primary etiology of heart failure at time of onset in the Framingham Heart Study (n = 534). Abbreviations: CAD, coronary artery disease; HTN, hypertension; VHD, valvular heart disease. Other, includes nonischemic cardiomyopathies.1 Source: Adapted from Lee et al., Circulation. 2009;119(24):3070-3077, with permission.
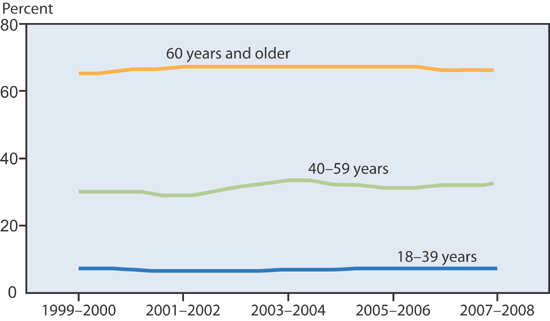
Alternative causes of heart failure include valvular heart disease and cardiomyopathy. Valvular disease as a cause of heart failure is important to identify because valve correction (surgical or percutaneous) can improve cardiac performance and patient outcome. Hypertension was more frequent in patients with higher ejection fractions (Figure 3.2).
FIGURE 3.2 HF-rEF versus HF-pEF in Framingham Heart Study. Etiology of heart failure divided by ejection fraction. Left panel: LVEF ≤ 45%, n = 314; 59% of total. Right panel: LVEF > 45%, n = 220; 41% of total. Abbreviations: Same as Figure 3.1.1 Source: Adapted from Lee et al., Circulation. 2009;119(24):3070-3077, with permission.
PREVALENCE OF RISK FACTORS FOR HEART FAILURE
The common risk factors for developing heart failure (coronary artery disease, hypertension, and diabetes) are associated with aging and obesity (Figure 3.3). When these conditions coexist, the incidence rate of heart failure markedly increases.4
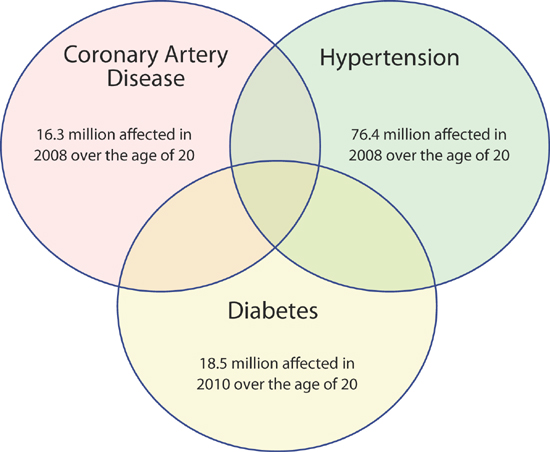
FIGURE 3.3 Prevalence of coronary artery disease, hypertension, and diabetes in the United States.2,3 Source: Adapted from Roger et al., Circulation. 2012;125(1):e2-e220 and Centers for Disease Control and Prevention, 2011, with permission.
Treatable Risk Factors for Heart Failure
Many of the risk factors for heart failure have treatment guidelines that reduce the morbidity and mortality of this syndrome.
CORONARY ARTERY DISEASE AND HEART FAILURE
Although different types of coronary artery disease (CAD) can occur at any age, atherosclerotic CAD is a disease of aging (Figure 3.4).5 In 2010, in age groups < 45, 45–64, and ≥ 65 years, the prevalence of CAD increased from 1.2% to 7.1% to 19.8%, respectively.6 However, between 2006 and 2010, the overall age-adjusted prevalence of CAD in the United States decreased from 6.7% to 6.0%.6 Although age-adjusted rates declined, coronary artery disease still accounted for one-third of all deaths in individuals over the age of 35 and was the primary cause of death in 405,309 cases in 2008.7
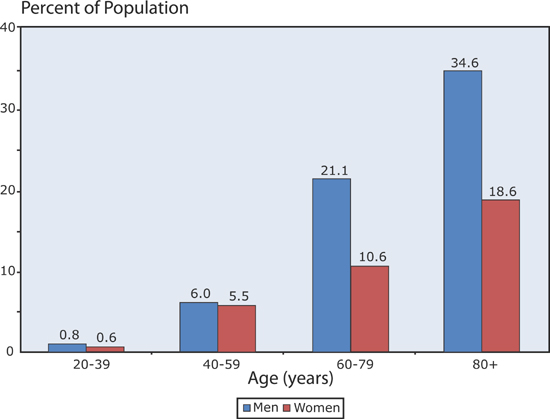
FIGURE 3.4 Prevalence of coronary heart disease by age group. Data from 2007–2010.8 Source: Adapted from Go et al., Circulation. 2013;127(1):e6-e245, with permission.
Prevention of Heart Failure by Treating Lipids in Patients with CAD
In the Scandinavian Simvastatin Survival Study (4S) trial, individuals with CAD without evidence of heart failure were treated with simvastatin versus placebo. Statin-treated patients had a lower risk of developing heart failure over a median follow-up of 5.4 years (relative risk = 0.79, P < 0.015).9 In the same trial, the simvastatin-treated patients also had a reduced likelihood of developing a decline in kidney function (relative risk 0.68, P = 0.01), highlighting the importance of preservation of multi-organ function to achieve the goal of prevention of heart failure.10
HYPERTENSION AND HEART FAILURE
Like CAD, hypertension incidence increases with age (Figure 3.5).11 Within any given age group over the past decade, the prevalence of hypertension, defined as having a blood pressure of ≥ 140/90 or on antihypertensive therapy, has remained steady (Figure 3.6).12
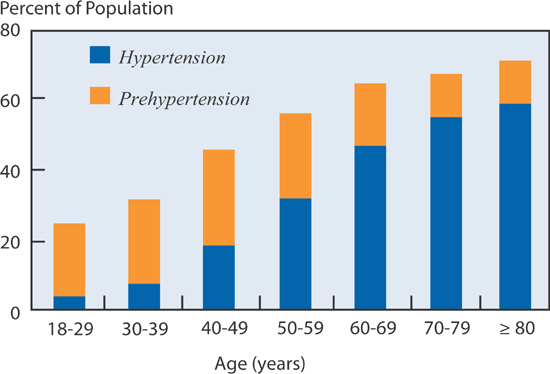
FIGURE 3.5 Prevalence of hypertension by age in the United States. Definitions: Hypertension is defined as systolic BP ≥ 140 mm Hg, or diastolic BP ≥ 90 mm Hg, or on medication. Prehypertension is defined as systolic BP 120–139 mm Hg or diastolic BP 80–89 mm Hg.11 Source: Adapted from the National Heart, Lung, and Blood Institute Chart Book 2012, with permission.
FIGURE 3.6 Prevalence of hypertension by age group has remained steady over time.12 Source: Adapted from the Centers for Disease Control and Prevention, with permission.
Prevention of Heart Failure by Treating Hypertension
In the SHEP (Systolic Hypertension in the Elderly Program) trial, individuals aged 60 years and older with a systolic blood pressure of 160 mm Hg or higher were treated with stepped care consisting of a diuretic, then beta-blocker therapies versus placebo. The treated patients had a reduced relative risk of developing heart failure (RR = 0.51) over a mean follow-up of 4.5 years (P < 0.001).13 In the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT), initial treatment with the diuretic chlorthalidone led to a lower incidence of subsequent heart failure compared to the ACE inhibitor lisinopril or the calcium channel blocker amlodipine.14
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree