Split Pleura Sign
Toms Franquet, MD, PhD
DIFFERENTIAL DIAGNOSIS
Common
Empyema
Sterile Reactive Collection
Malignant Effusion
Less Common
Hemothorax
Postsurgical
Pleurodesis
Rare but Important
Chronic Tuberculous Pleuritis
ESSENTIAL INFORMATION
Key Differential Diagnosis Issues
Not specific for empyema
Can occur with other causes of loculated pleural fluid
CECT
Enhancement of thickened inner visceral and outer parietal pleura
Thickened visceral and parietal pleural layers separated by fluid
Thickening of extrapleural fat
Helpful Clues for Common Diagnoses
Empyema
Commonly associated with bacterial pneumonia
Gram positive bacteria (Staphylococcus aureus & Streptococcus pneumoniae): 50%
Transformation of parapneumonic effusion (not infected) into complicated effusion (infected but not purulent) and into empyema (frank pus)
CECT features
Pleural enhancement: Not seen in transudative effusions
High accuracy in differentiating empyema from lung abscess
Sterile Reactive Collection
Smooth, thin pleural surfaces and homogeneous fluid density
Malignant Effusion
Mesothelioma
Parietal and to lesser extent visceral pleura involvement
Metastases: Most common from breast, ovary, lung, and malignant thymoma
Pleural nodularity
Helpful Clues for Less Common Diagnoses
Hemothorax
More uniform pleural thickening
Postsurgical
Expected after lobectomy and pneumonectomy
Pleurodesis
Often for malignant effusions
High attenuation areas in posterior basal regions of pleural space
Extension of talc deposits into fissures
Helpful Clues for Rare Diagnoses
Chronic Tuberculous Pleuritis
Thick calcification
Image Gallery
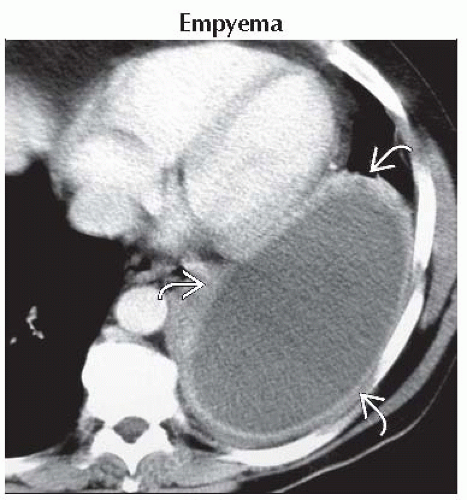 Axial CECT shows a large, loculated, left-sided pleural fluid with a typical split pleura sign
 . Thoracocentesis showed empyema. . Thoracocentesis showed empyema.Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|