5

Special Techniques
Examination for Emphysema
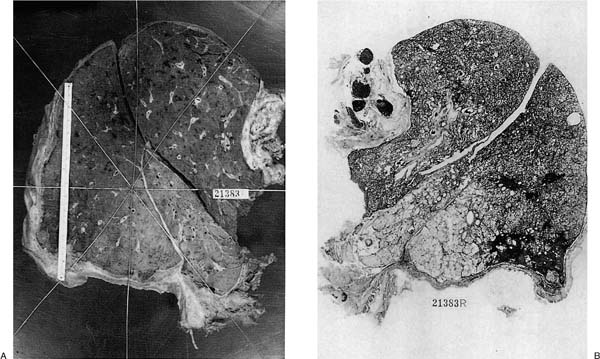
Inflation of the lung was first introduced by Laennec in the early 19th century, enabling him to make the first adequate description of emphysema. The practice of lung inflation then more or less ceased until the 1940s and 1950s, when it was reintroduced primarily to study the morphology of emphysema. Inflation itself is not a guarantee that emphysema can be recognized adequately. Severe emphysema is easily and more accurately recognized from a slice of inflated lung (see Chapter 22) than from uninflated lung (Fig. 5–1). Mild degrees of panacinar emphysema cannot be recognized with facility even on slices from inflated lung, although moderate degrees can be suspected as the lung parenchyma “falls away” and airways, vessels, and lobular septa are raised above the surface of the slice. By contrast, mild centrilobular emphysema can be recognized because bronchial pigment highlights the center of the lobule; the mildest degree of centrilobular emphysema may require the use of a hand lens.
Different techniques have been developed to search for emphysema on a macroscopic (or submacroscopic) level. The paper-mounted whole-lung section technique (see below) was extensively used between the 1950s and 1980s, but has since fallen out of favor because it is messy, time-consuming, and requires a relatively large workspace. The barium sulfate impregnation technique,1 followed by examination with a dissecting microscope or hand lens of the slice immersed in water, continues to be used in many pathology departments (Fig. 5–2). Fixation by Bouin’s fluid has been used as an alternative to barium sulfate impregnation. This colors airspace walls, rendering them opaque, and it also highlights emphysema. In our experience Bouin’s fluid has no advantages over barium sulfate; it is equally messy to deal with, leaves the lung an unpleasant color, and adversely affects some types of immunoperoxidase staining, as well as in situ hybridization.
Other techniques (see later in this chapter) leave the lung in a distended and fixed condition, allowing examination with a hand lens or dissecting microscope without the bother of fluid immersion. The formalin fume fixation method2,3 provides excellent specimens for the teaching museum, but they are rather brittle and must be protected. Cold fume preparations4,5 are described, but have deficiencies in that fixation may be patchy, rendering the specimen inadequate for a museum or laboratory storage archives. The hot formalin fume technique must be performed carefully and in a fume hood, because production of the formalin vapors involves boiling the formalin. The polyethylene glycol method must also be done in a fume hood, but is less dangerous than the formalin fume method in that the fixative mixture is removed from the lung by pressurized room air delivered through the bronchus, with the mixture dripping from the pleural surface into an underlying pan. The lung is then sectioned. The lung parenchyma is relatively soft, allowing sections to be taken. The slices must be protected from compression. Both formalin and polyethylene glycol preparations can be used for radiography or computed tomography (CT) scanning. They cannot be used for morphometric analysis unless prior data (lung volumes, CT scans) are available as correction factors.6
FIGURE 5–1 (A) Formalin-inflated slice of lung is immersed in water. Emphysema is present, although not easy to see, and is most easily recognized in the anterior basal segment of the right lower lobe. (B) A paper-mounted whole-lung section renders the emphysema much easier to see. The patient has nodular and progressive massive silicosis. (From Thurlbeck WM. Christie lecture: emphysema then and now. Can Respir J 1994;1:21–39 with permission.)
Distention of the lung with frozen section embedding media allows for samples to be frozen as archival tissue for subsequent analysis using frozen section. Alternatively, the lung can be distended with agarose gel;7 this would provide the same cytologic detail and ease of sectioning, and is much less expensive than the embedding media.
Special Procedures
A variety of special procedures can be applied to the lung at postresection or postmortem examination. Many procedures are likely to be used primarily for research; for such a purpose, investigators need to have full knowledge of the literature and some empirical experience with the technique involved. A detailed description of these techniques, therefore, is not provided here, but brief and general reference will be made to several techniques.
Electron Microscopy
Fixative with a marker dye can be injected into the lung in situ as soon as autopsy permission is obtained and the injection site identified and sampled at a later time.8 The lung appears to be quite remarkably resistant to postmortem autolysis, and relatively well-preserved normal lung has been described 8 hours postmortem.
Even fresh lungs not specially prepared, formalin-fixed lungs after long periods of time, and lung tissue in paraffin blocks may provide useful information. Typically, virus particles and tumor markers can be identified from such tissues. Although a quite startling return to normal ultrastructural appearance following treatment of the autolyzed lung with a modified Krebs-Henseleit solution and 95% oxygen and 5% carbon dioxide has been found,9 there are finite time limits for success using this technique.
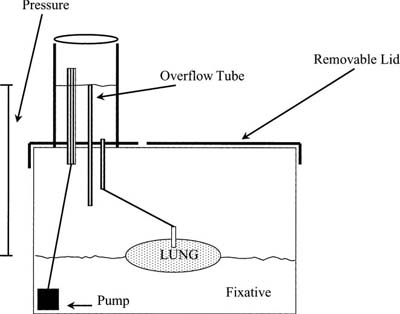
Quantitation of Lung Structure
If the absolute measurements described in Chapter 3, such as alveolar volumes or surface area, are required, the lung needs to be fixed at a standard distending pressure. Various preparation techniques have been described and reviewed in some detail.10 The simplest technique is a modification of a very early design1 (Fig. 5–3), and it is possible to design a system for multiple tanks if necessary.11 A constant distending pressure of 25 or 30 cm is usually used. A tank can be built from sturdy plastic, with the basic tank purchased as a standard kitchen or laundry hamper, and the lid modified for the recirculation chambers. Immersion pumps can be quite inexpensive, and can be easily purchased from a garden store as a low-pressure, low-flow, fountain pump. Fixative is recirculated from the tank that holds the lungs to a reservoir that has an outflow into the main tank; measurements taken from the level of the formalin in the delivery reservoir to the level of the formalin in the tank determine the distending pressure. Conduits from the reservoir lead from plastic tubes into the bronchi of the lungs to be distended and are tied in place using variable-diameter plastic connectors. Tanks are best placed in a well-ventilated place, a standard fume hood, a small portable hood, or custom-built hood. It is important that the lungs be as leak-free as possible; tying the major arteries and veins before removing the lungs from the heart also improves inflation. To reduce leaks, special care needs to be taken when removing the lungs from the cadaver, and a towel placed over the cut ends of the ribs is useful in preventing lacerations.
FIGURE 5–2 Photographs taken by dissecting microscopy after barium sulfate impregnation of a lung slice. (A) Normal lung. (B) Two centrilobular emphysematous spaces. (From Thurlbeck WM. Christie lecture: emphysema then and now. Can Respir J 1994;1:21–39 with permission.)
The lungs should first be distended rapidly to apparent full distention with fixative, and then attached to the constant inflation device. This is necessary because fixation proceeds as distention occurs, and large lungs may not reach full inflation. During the transfer of apparently fully distended lung, formalin will escape from the bronchus, so the fear of overinflation is groundless. Lungs inflated in this way are smaller than those predicted from life and considerably smaller than air-filled excised lungs at comparable pressures,12 but their volume is close to lung volumes assessed radiologically.13 No purpose is served by correcting to predicted total lung capacity (TLC) in individual patients because observed and predicted TLCs vary by ±20% in individual patients. It may be appropriate to correct to air-distended lung volumes, but this requires an additional procedure, and there is no guarantee that it is the appropriate reference volume. The advantage of a standard pressure of fixative is that it is standard; thus, observers using this technique can refer to the results of others using it. Lung volumes are easily and accurately measured by water displacement.14 This is accomplished using a bottom-loading balance; a maximum of 10 kg is necessary for adult lungs. Alternatively, weighing the lung before and after full inflation also provides a relatively accurate estimation of lung volume.
FIGURE 5–3 System for formalin inflation using a recirculation tank apparatus.
Bronchograms
Bronchograms can be performed postmortem using the usual clinical contrast media, lead,15 or tantalum.16 The second of these is toxic, and the third is potentially explosive, and therefore we would strongly recommend using only contrast media. Computed tomography scans can be performed on air-inflated lungs, allowing measurements of bronchial wall thickness, or of bronchial anatomic variations.
Arteriograms (and Venograms)
Arteriograms have been a well-utilized technique, providing information about normal and abnormal appearance of the pulmonary arterial tree in children and adults.17 The particular feature of the technique is that in vivo muscular tone may persist, and to reduce this it is advisable that the postmortem interval be long; freezing and then warming may also be advantageous. In addition, nonphysiologic pressure (120 mm Hg) is advisable so that full distention of vessels is obtained in all cases. A major problem with this technique is the presence of postmortem clots; saline lavage or detergent lavage may obviate this to some extent. The easiest contrast medium to use is that described by Schlesinger.18 It is not necessary to add formalin to the injection mass because subsequent intra-bronchial formalin fixation will harden it. The standard injection technique is that of Short,19 modified for present-day materials. This is a simple technique in which the vasculature is first flushed with a heparinized saline solution, followed by injection of a warm (60°C) mixture of barium (Micropaque) as an 80% suspension with 3% gelatin at 100 cm pressure for 7 minutes. This provides excellent visualization of the smallest vessels.
Casts of Airways and Vessels
This technique was originally devised to investigate airway and vascular branching patterns, and their alterations in disease states.20,21 The resin used by the earlyworkers is not available in North America because of hazards in transportation; large numbers of other resins are available. In casting vessels, we have found that a methacrylate solution such as Mercox (Ladd Research Industries, Burlington, VT), or Batson’s replica and corrosion kit (Polysciences, Markham, Ontario), works well. If only the major vessels are selected, sufficient catalyst must be added so that the solution has an increased viscosity and will not extend into the capillary bed. Conversely, if the capillary bed is to be analyzed, less catalyst should be used. Lungs containing methacrylate can be sectioned for histology, or the lung tissue can be digested using bleach, and the cast can be morphometrically examined using light or scanning electron microscopy.22–25
A negative pressure bronchial casting method using silicone elastomers has been described.26
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree