7 Special Techniques
Transseptal Heart Catheterization
Indications
Indications for transseptal heart catheterization include the following (Table 7-1):
Table 7-1 Indications for Transseptal Left-Sided Heart Catheterization
| Measurement of Left Atrial or Left Ventricular Hemodynamics |
| Mitral valve |
| Aortic valve |
| Left Ventricular Angiography |
| Valvuloplasty |
| Electrophysiology Studies |
Contraindications
Contraindications for transseptal heart catheterization include the following:
Transseptal left-sided heart catheterization should be considered carefully for patients with distorted cardiac anatomy resulting from congenital heart disease, dilated aortic root, marked atrial enlargement, or thoracic skeletal deformity.
Procedural Highlights
The Equipment
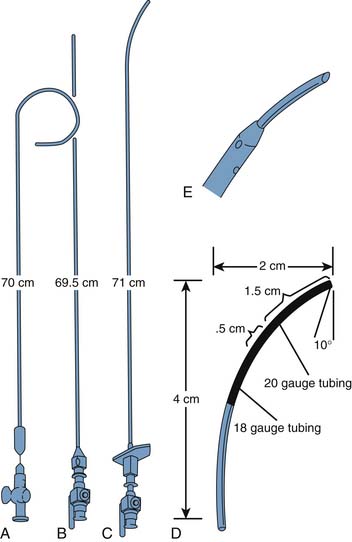
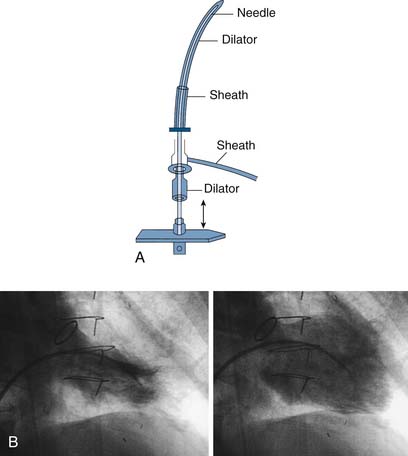
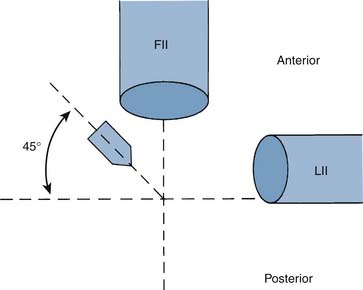
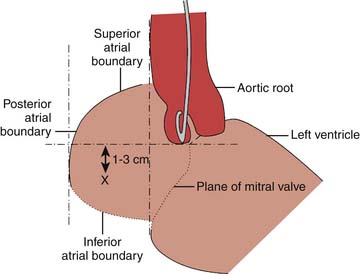
Figure 7-1 shows the curved long catheter (Fig. 7-1, A) and long hollow needle (Fig. 7-1, C) used to cross the atrial septum. A long sheath with an extending curved obturator that accepts a 0.032-inch guidewire has now replaced the straight stylet that was used for insertion of the curved transseptal catheter from the femoral vein into the right atrium. The modified transseptal needle has a 21-gauge needle tip to reduce hazard from accidental puncture of the aorta or atrial wall, and the catheter has side holes (to enhance injection of contrast medium) and a tapered tip to facilitate entry into the femoral vein and traversal of the atrial septum. Detail of transseptal needle tip is shown in Figure 7-1, D. Several methods exist to cross the atrial septum. Intracardiac echocardiography is popular among electrophysiologists to guide their approach. Using angiographic landmarks alone is commonly used by seasoned operators and is described here. The transseptal Mullen’s catheter and sheath system or Brockenbrough catheter with large or small curves are the catheter systems most commonly used (Fig. 7-2). The transseptal needle system is gently curved and attached to a pressure transducer with a rotating adaptor for free movement of the long needle within the catheter as it travels up to the heart.
Steps to perform transseptal catheterization are as follows
Preparatory Notes
Risks of Transseptal Catheterization
Punctures of the aortic root, the coronary sinus (CS), or the posterior free wall of the atrium are potentially lethal problems (Table 7-2). In patients who have not been given anticoagulants the 21-gauge tip of the needle rarely causes a problem. However, if the large transseptal catheter is advanced into these spaces, cardiac tamponade may occur. The catheter-needle combination should not be advanced if the operator is not satisfied with the position of the transseptal catheter in the right atria. If the catheter assembly is not in the correct position, the operator must remove the transseptal needle, reinsert the guidewire to the SVC, reposition the catheter, and reposition the needle with withdrawal and turning to the fossa ovale as indicated earlier.
Table 7-2 Risks Related to Transseptal Catheterization
| Cardiac perforation |
| Puncture into the aortic root |
| Pericardial tamponade∗ |
| Embolus from the left atrium |
∗ Almost all deaths related to transseptal catheterization are a result of tamponade.
Direct Transthoracic Left Ventricular Puncture
Indications
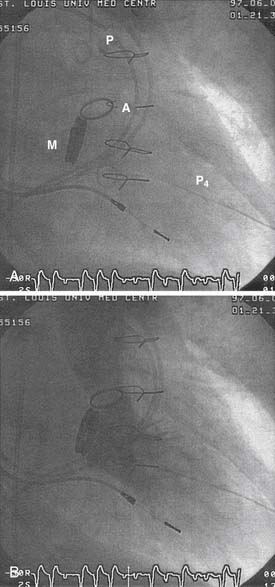
Before the procedure, two-dimensional echocardiography from the apical window is helpful in locating the true LV apex and determining the direction of the long axis of the left ventricle. After the arterial and right-sided heart catheters have been placed, an 18-gauge, 4.25-inch–long needle with a Teflon sheath connected to a pressure transducer is inserted at the apical area through the intercostal space close to the upper border of the lower rib in this space. It is directed posteriorly toward the right shoulder. The pressure tracing is continuously monitored while the needle is advanced. After the needle enters the ventricle, it is removed, leaving the Teflon sheath in place through which pressure recordings and angiography are performed. Alternatively a guidewire can be inserted and a 4 F pigtail catheter can be advanced into the left ventricle for hemodynamic and angiographic data. Figures 7-5 and 7-6 illustrate a typical case of direct LV puncture and associated hemodynamics.