Solitary Pulmonary Nodule
GENERAL PRINCIPLES
• The solitary pulmonary nodule (SPN) is a common incidental finding on CXR or CT scan.
• The primary goal of working up an SPN is to determine whether the nodule is malignant or benign. Early removal of malignant nodules can significantly increase survival rate.
• After an SPN is detected, all prior CXR and CT scans should be reviewed. If the nodule is unchanged over 2 years, no further evaluation is necessary.
• For nodules with low malignancy likelihood, serial imaging is recommended.
• Intermediate malignancy likelihood requires additional diagnostic studies.
• Nodules with high likelihood of malignancy should be removed and further treatment is indicated.
• The SPN is defined as a single opacity <3 cm within and surrounded by aerated lung parenchyma without evidence of atelectasis or hilar enlargement. These were previously referred to as coin lesions.
• Lesions >3 cm are referred to as a mass, and have a higher likelihood of being malignant.
• Prevalence of malignant SPN varies widely depending on population and reason for imaging (i.e., in the setting of a screening study or detected incidentally).
• Over 150,000 patients per year evaluated for SPN, almost all are asymptomatic.1
• Of benign nodules, >80% are infection related.2
• Malignant nodules are usually primary neoplasms of the lung—about 50% are adenocarcinoma, 22% squamous cell carcinoma, 8% solitary metastasis, 7% undifferentiated non–small-cell carcinoma, and 4% small-cell carcinoma. Uncommon causes include large cell carcinoma, carcinoid, and lymphoma.3
• SPNs are relatively common, particularly by CT scan.
DIAGNOSIS
Clinical Presentation
History
• SPN is radiographic diagnosis, but one should obtain a complete history with an emphasis on risk factors for malignancy or granulomatous disease.
• A detailed smoking history is essential because tobacco is the leading risk factor for primary lung cancer, with relative risk 10–30-fold greater than that of nonsmokers.
• Age is also important. In patients >50 years old, an SPN has a 65% chance of being malignant, whereas in patients <50 years old the chance is 33%.4
• Other risk factors include
 Exposures to asbestos, second-hand smoke, radon, arsenic, radiation, haloethers, nickel, and polycyclic aromatic hydrocarbons.
Exposures to asbestos, second-hand smoke, radon, arsenic, radiation, haloethers, nickel, and polycyclic aromatic hydrocarbons.
 Environmental exposures such as living in an area with pathogenic endemic fungi.
Environmental exposures such as living in an area with pathogenic endemic fungi.
 Risk factors for or having resided in an area with a high prevalence of Mycobacteriumtuberculosis.
Risk factors for or having resided in an area with a high prevalence of Mycobacteriumtuberculosis.
• Details on symptoms if present:
 Chest pain, especially pleuritic, may indicate pleural, mediastinal, or pericardial involvement.
Chest pain, especially pleuritic, may indicate pleural, mediastinal, or pericardial involvement.
 New diffuse pain or bone pain may indicate metastatic disease or hypertrophic osteoarthropathy.
New diffuse pain or bone pain may indicate metastatic disease or hypertrophic osteoarthropathy.
 Weight loss is nonspecific but if present with malignancy is a poor prognostic factor.
Weight loss is nonspecific but if present with malignancy is a poor prognostic factor.
 Cough may or may not be present and is nonspecific.
Cough may or may not be present and is nonspecific.
 Hemoptysis with an SPN can suggest malignancy such as a squamous cell carcinoma or proximal lesion.
Hemoptysis with an SPN can suggest malignancy such as a squamous cell carcinoma or proximal lesion.
 Hoarseness may be present from compression or invasion of the left recurrent laryngeal nerve.
Hoarseness may be present from compression or invasion of the left recurrent laryngeal nerve.
• Past medical history can yield risk factors for infection or malignancy.
 Any immunosuppressed state including HIV, autoimmune disease, chronic corticosteroid or other immune-modulating medications, or post-transplantation status broadens the differential diagnosis for infection as well as malignancy.
Any immunosuppressed state including HIV, autoimmune disease, chronic corticosteroid or other immune-modulating medications, or post-transplantation status broadens the differential diagnosis for infection as well as malignancy.
 History of chronic obstructive pulmonary disease (COPD) may indicate past or current smoking history.
History of chronic obstructive pulmonary disease (COPD) may indicate past or current smoking history.
 History of any malignancy, but especially cancers that metastasize to the lung (e.g., lung cancer, malignant melanoma, sarcomas, and colon, breast, renal, germ cell, and bladder cancers), raises suspicion of a metastatic lung nodule.
History of any malignancy, but especially cancers that metastasize to the lung (e.g., lung cancer, malignant melanoma, sarcomas, and colon, breast, renal, germ cell, and bladder cancers), raises suspicion of a metastatic lung nodule.
Physical Examination
• A thorough examination can yield clues to complications of direct involvement of the SPN, metastatic disease, paraneoplastic disease, or evidence of infection.
• Focal wheezing may suggest intraluminal tumor.
• Signs to look for include clubbing and long bone swelling (hypertrophic osteoarthropathy), hepatomegaly, bone tenderness (metastases), plethoric face, engorged neck, and superficial veins (superior vena cava syndrome), wasting, lymphadenopathy, and focal neurologic deficits.
Differential Diagnosis
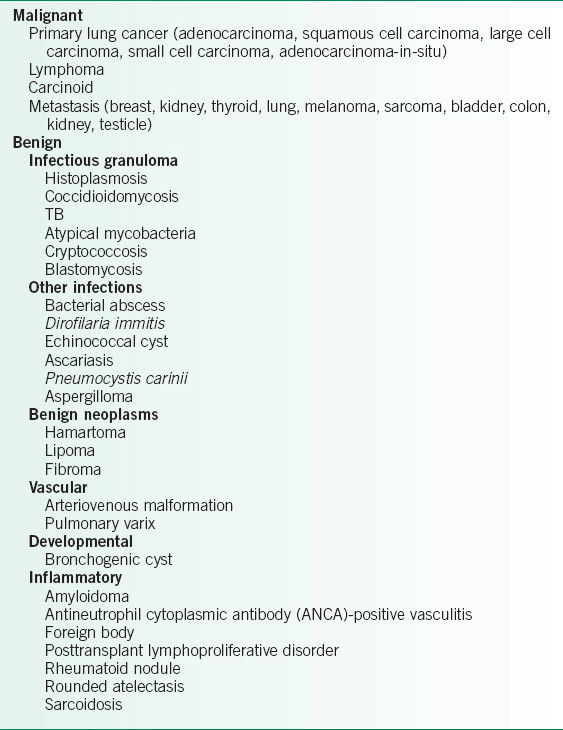
• The differential diagnosis can be divided into malignant and nonmalignant causes (Table 27-1).
• Malignant causes include primary lung cancers (adenocarcinoma, squamous cell carcinoma, large-cell carcinoma, small-cell carcinoma, adenocarcinoma-in-situ [fomerly referred to as bronchoalveolar cell carcinoma]), metastatic cancers, and carcinoid tumors.
• Nonmalignant causes include benign neoplasms, vascular malformations, developmental abnormalities, inflammatory nodules, and infections (granulomatous and nongranulomatous).
Diagnostic Testing
Laboratories
• Laboratory evaluation should include a complete blood count, electrolyte panel, creatinine, and hepatic function panel.
• Hypercalcemia may be due to bony metastases or release of parathyroid hormone (PTH)-related peptide from a squamous cell carcinoma.
• Hyponatremia may be due to the syndrome of inappropriate antidiuretic hormone secretion (SIADH), which can be seen in small-cell carcinoma or significant pulmonary or neurologic disease.
• Liver abnormalities may suggest liver metastases.
• If the history includes risk factors for endemic fungi or TB, additional focused laboratory testing should be obtained.
TABLE 27-1 DIFFERENTIAL DIAGNOSIS OF THE SOLITARY PULMONARY NODULE
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


