The Chest Radiograph
GENERAL PRINCIPLES
• The CXR is ubiquitous in medicine and remains among the hardest of diagnostic studies to master. The key to proficiency lies in reviewing all CXRs ordered. Close interaction with radiology staff is invaluable in building ones’ skills and honing in on a specific diagnosis.
• Using a constant search pattern will allow for systematic and comprehensive analyses.
• Ideally, CXRs should be interpreted without knowledge of the clinical context to allow an unbiased and objective evaluation of the study. However, similar to any diagnostic test, evaluating the CXR in the context of the clinical scenario is very important and allows a focus on specific areas of the study and a detailed search for associated pathologic findings.
• At the Mallinckrodt Institute of Radiology (MIR), we try to initially read all CXRs without any clinical history. The clinical information is reviewed after the initial perusal so as to avoid bias at first glance and ensure subtle, clinically relevant issues are not overlooked.
• The importance of prior CXRs for comparison cannot be stressed enough. Understanding a finding often relies on knowing whether it is acute, subacute, or chronic. An area of consolidation, for example, could represent a community-acquired pneumonia on a CXR. If the area is stable from 1 year ago, low-grade adenocarcinoma or radiation changes become more likely.
• In our daily practice we often rely on old films. They are cheaper and lower in radiation than a CT and often provide greater information.
INITIAL ASSESSMENT
Patient Position and Study Quality
• Initial evaluation begins with assessment of patient position and quality of the study.
• This evaluation includes assessing the film for:
 Rotation
Rotation
 Degree of inspiration
Degree of inspiration
 Patient position
Patient position
 Radiation dose
Radiation dose
Patient Rotation
• A common method of assessing for the presence of rotation is to evaluate the relationship of the medial heads of the clavicles to the spinous processes of the vertebral bodies. When truly straight, each clavicular head will be equidistant to the adjacent spinous process.
• If the patient is rotated, the mediastinal borders will be altered. Rotation can be confused for mediastinal widening. Lack of appreciation for patient rotation can result in needless workup of perceived mediastinal changes.
Degree of Inspiration
• The degree of inspiration will affect the density of the lungs.
• As a general rule, the diaphragm should be crisp and the peak should be rounded.
• For those who prefer counting ribs, 10 posterior ribs and 6 anterior ribs should be seen on an inspiratory study.
Patient Position
• Erect versus supine positioning is pertinent to verify, as it will alter the interpretation of air–fluid interfaces, blood flow distribution, and caliber of the pulmonary vessels. Cephalization, for example, can be appreciated only on an upright film.
• The air–fluid level in the gastric fundus often allows one to understand whether the CXR is upright, supine, or decubitus.
Radiation Dose
• Radiation dose of a CXR has become more challenging in the digital era.
• As a general rule, the optimally exposed CXR allows visualization of the vertebral bodies and disk spaces through the mediastinal structures and also allows visualization of the pulmonary vessels through the heart and diaphragm.
• With new digital techniques, postprocessing allows the technologist to manipulate the image to achieve this same effect. The reader, therefore, must be careful that he/she can see through both the heart and mediastinum but that the image does not look too pixilated. Should pixilation occur, the reader must be aware that an insufficient radiation dose was used.
CXR Views
• There are a number of different variations of a CXR that may be obtained to evaluate thoracic pathology. These include the posteroanterior (PA) view, the lateral (LAT) view, the anteroposterior (AP) view, and the lateral decubitus (LD) view. Some centers also make use of end-expiratory (EE) views.
• All of these views share the concept of a point source which results in a fan x-ray beam. The result is magnification of structures which are farther from the detector. A good analogy is the shadow created by your hand on a classroom desk from an overhead light bulb. If you lift your hand off the desk, the shadow becomes bigger and fuzzier.
Posteroanterior View
The PA view is acquired with the patient in a standing position during full inspiration. The patient faces the detector, which is in contact with the anterior chest wall. The x-ray beam is directed toward the cassette from a distance of 6 ft, which results in minimal magnification of the heart.
Lateral View
• The LAT view is also taken with the patient standing during full inspiration at a distance of 6 ft. The arms are lifted. By convention, the patient’s left side is placed in contact with the detector, and the beam is directed from right to left to reduce magnification of the heart.
• LAT views are useful for evaluating lesions behind the heart, diaphragm, or mediastinum that may be hidden on PA views.
• The left diaphragm can be differentiated from the right diaphragm on this view by locating the loss of the left diaphragmatic border when in contact with the cardiac silhouette or by locating the right posterior ribs (which will appear magnified and larger since they are farther from the cassette).
• It is important to note that magnification is about the same between the PA and LAT views. If a lesion is found on one view, the relationship with a landmark (e.g., aortic arch) can be used to localize it on the other.
Anteroposterior Views
• The AP views are usually taken with portable machines and are most often used to image the chest in patients who cannot have formal PA and LAT views, such as intensive care unit or intraoperative patients.
• These studies are conducted with the cassette behind the patient, in contact with his/her back. The x-rays are directed from front to back, often at a distance of <6 ft. The patient is often in a sitting or supine position and unable to perform a full inspiration.
• AP views often result in increased lung attenuation (from lack of complete inspiration) and increased magnification of mediastinal and cardiac structures (from increased distance between these structures and the cassette).
• It is important to understand that magnification of anterior structures occurs in the AP view to prevent inappropriate interpretation of an enlarged mediastinum or cardiac silhouette.
Lateral Decubitus Views
• LD views are taken with the patient lying on the ipsilateral side. For example, a left LD is taken with the left side down.
• There are four clinical situations in which a decubitus view might be helpful.
 When evaluating whether the ipsilateral effusion is mobile
When evaluating whether the ipsilateral effusion is mobile
 When evaluating whether a contralateral pneumothorax is present
When evaluating whether a contralateral pneumothorax is present
 When the contralateral lung has a concomitant pneumonia with an effusion
When the contralateral lung has a concomitant pneumonia with an effusion
 When the ipsilateral lung collapses normally. If it does not, one might suspect a radiolucent foreign body
When the ipsilateral lung collapses normally. If it does not, one might suspect a radiolucent foreign body
End-Expiratory Views
• EE views are occasionally used to detect a subtle pneumothorax. The EE view should accentuate a pneumothorax as the EE radiograph will make the lung artificially whiter.
• Care must be taken to avoid mixing inspiratory and expiratory images when following a pneumothorax on serial images. The expiratory images will exaggerate the size of the pneumothorax.
GENERAL APPROACH TO CXR INTERPRETATION
• A systematic approach to the CXR reduces the risk of missed pathology. Subtle pathologies can be missed for two reasons. Only the process that is suspected is noted. Or, an obvious but previously unexpected finding commands the viewer’s attention.
• There are as many systems for evaluating CXRs as there are physicians. The schema used here is arranged so that often-neglected areas are addressed first, and more common areas that may divert attention are addressed last.
• The PA CXR is addressed in detail, but any view can be read in a similar or slightly modified fashion.
Osseous Structures
The first structures surveyed are the osseous structures of the thorax, including the ribs (anterior and posterior aspects), the sternum (including signs of previous sternal splitting surgeries), the shoulder girdle (including the clavicles and scapulae), and the spine (both the vertebrae and the disk spaces). The skeletal survey should look for clues to understanding the other findings, including fractures, metastases, or previous surgery.
Upper Abdomen
Next, the upper abdomen is inspected. On an upright film any gas collections are evaluated, including the stomach bubble and the colon. Displacement of these structures may be indicative of organomegaly. An abnormal shape of the gas may be indicative of free intraperitoneal gas. The upright PA film is the study of choice for evaluating the presence of free air in the abdomen which is seen as a thin crescent under the diaphragm.
The Diaphragm
The diaphragm is evaluated next. The hemidiaphragms are smooth hemispherical structures, with the right diaphragm being 2–3 cm higher than the left owing to the presence of the liver below. The hemidiaphragms should be evaluated for shape (flattened in hyperinflation), sharpness (obscured with pleural effusions), and general symmetry (eventration, paralysis, or hernia through the hemidiaphragm leads to asymmetry).
The Mediastinum
Evaluation of the mediastinum usually follows, and is one of the more complex parts of the CXR evaluation because it includes so many thoracic structures.
Mediastinal Lines
The nine key lines of the mediastinum should be assessed for any focal distortion or displacement.
• The interfaces of the lungs, the anterior and posterior junction lines
• The right paratracheal stripe
• The left subclavian artery reflection
• The concave aorticopulmonary window
• The descending aorta
• The left and right paravertebral lines
• The azygoesophageal recess
Mediastinal Borders
• The nine lines are followed by the right and left mediastinal borders.
• The right border is formed (from bottom to top) by the right atrium, the ascending aorta, and superior vena cava.
• The left border is formed (from bottom to top) by the left ventricle, left atrial appendage, main pulmonary artery, and aortic knob.
• Both global cardiac and chamber enlargement should be noted. Global cardiac enlargement can be determined by calculating the cardiothoracic ratio—the width of the cardiac shadow on a PA view should be less than half the internal width of the bony thorax at its widest point. Any ratio >50% usually signifies cardiac enlargement.
• Although chamber enlargement is often the cause of an enlarged cardiac shadow, a pericardial effusion gives a similar appearance and should always be considered, especially when there is an acute change in apparent cardiac size.
• The LAT film can be especially helpful in differentiating chamber enlargement versus pericardial effusion. On an LAT film the pericardium is usually seen as a 2-mm stripe between two lucent arcs. In the presence of an effusion, this stripe is thickened. This finding is fairly specific and is often referred to as the sandwich or Oreo cookie sign.
Mediastinal Masses
• Mediastinal masses are often noted on this portion of the evaluation. The mediastinum is broken up into three different compartments, anterior, middle, and posterior for convenience of differential diagnosis. While various methods for dividing the mediastinum exist, a commonly used method is to define the compartments as follows:
 Anterior mediastinum as the compartment between the sternum and an imaginary line drawn directly anterior to the trachea and posterior to the inferior vena cava. The differential for anterior mediastinal masses is usually headed by thymic lesions (thymoma and germ cell tumors) and lymphoma.
Anterior mediastinum as the compartment between the sternum and an imaginary line drawn directly anterior to the trachea and posterior to the inferior vena cava. The differential for anterior mediastinal masses is usually headed by thymic lesions (thymoma and germ cell tumors) and lymphoma.
 Middle mediastinum as the compartment from the trachea to a vertical line drawn 1 cm behind the anterior edge of the vertebral bodies. The differential for middle mediastinal masses most commonly includes foregut duplication cysts (esophageal or bronchogenic) or lymphadenopathy, but a hiatal hernia should be considered if an air–fluid level is present.
Middle mediastinum as the compartment from the trachea to a vertical line drawn 1 cm behind the anterior edge of the vertebral bodies. The differential for middle mediastinal masses most commonly includes foregut duplication cysts (esophageal or bronchogenic) or lymphadenopathy, but a hiatal hernia should be considered if an air–fluid level is present.
 Posterior mediastinum as the remaining space. Most posterior mediastinal masses are neurogenic in nature usually schwannoma or neurofibroma.
Posterior mediastinum as the remaining space. Most posterior mediastinal masses are neurogenic in nature usually schwannoma or neurofibroma.
The Aorta
The aorta should also be evaluated on the CXR. All of its portions (ascending, arch, and descending) should be evaluated for enlargement (possible aneurysm), calcification (atherosclerotic disease), and tortuosity (hypertensive disease).
The Hila
The hila are then evaluated. Their shape, size, and density are important and may indicate the presence of disease. The left hilum should be higher than the right owing to the fact that the left pulmonary artery courses above the left mainstem bronchus and the right pulmonary artery arises below the right mainstem bronchus.
The Pleural and Extrapleural Spaces
• The pleural space (between the parietal and visceral pleurae) and extrapleural spaces (between the parietal pleura and chest wall) are also carefully inspected.
• First, the pleura along the diaphragm is inspected from the cardiophrenic to the costophrenic angles. Next, the pleura lining the lateral margin of the lung is followed upward to the apex, and then over and down the mediastinal contour to the cardiophrenic angle where the inspection began.
• By following the pleural markings, the fissures of the lungs (including fluid collecting or tracking into them) and even accessory fissures can be evaluated.
• Careful examination of these spaces allows for the detection of small pleural effusions, pneumothoraces, pleural thickening or calcification, and masses.
• LAT films are more sensitive than PA films for the detection of small pleural effusions. Whereas ∼175 mL of fluid is needed to produce blunting of the costophrenic angles on PA views, as little as 75 mL can be detected in the costophrenic angle on an LAT view.
Extrapulmonary Masses
• Extrapulmonary masses (pleural and extrapleural) can be difficult to distinguish from pulmonary masses on PA films.
• A number of features may assist in differentiating between the two types of masses.
 First, a second view can be obtained (a mass overlying the lungs on a PA view may be noted to be extrapulmonary on an LAT view).
First, a second view can be obtained (a mass overlying the lungs on a PA view may be noted to be extrapulmonary on an LAT view).
 Second, the interface between the lesion and the lung is sharp with an extrapulmonary mass because they are superimposed structures.
Second, the interface between the lesion and the lung is sharp with an extrapulmonary mass because they are superimposed structures.
 Third, the angle between the chest wall and an extrapulmonary lesion is obtuse (>90 degrees).
Third, the angle between the chest wall and an extrapulmonary lesion is obtuse (>90 degrees).
• The incomplete border sign can be useful as well. In this sign, only 270 degrees of a round mass are seen. This comes from the fact that the last 90 degrees is the portion that is arising from the pleura or chest wall. As a general rule this sign denotes an extrapulmonary mass.
Medical Devices
Medical devices should also be carefully evaluated. Commonly encountered medical appliances include endotracheal tubes (ETs), nasogastric tubes, central venous catheters (including dialysis catheters), Swan–Ganz catheters, pacing and defibrillating devices, coronary artery stents, chest tubes, various peritoneal shunts, and surgical staple lines or wires.
Endotracheal Tubes
ET tips should be assessed for proper location, ideally 4 cm from the carina in the midtrachea with a minimal safe distance of 2 cm from the carina. Malpositioned ET tubes may ventilate only one lung if advanced too far, leading to contralateral lung collapse, or may enter the pharynx or dislodge into the esophagus if placed too superiorly. ET tubes move with changes in chin position. When the patient flexes, the tip advances. In other words, the “hose follows the nose.”
Nasogastric Tubes
Nasogastric tubes should be evaluated for proper positioning.
Central Access Devices
• Central venous catheters need to be evaluated for proper course and tip placement in the superior vena cava, with special attention for pneumothorax after placement.
• Swan–Ganz catheter tips should be assessed for proper location in the pulmonary artery, and should not be advanced any more distally than the proximal interlobar pulmonary arteries (tip should remain within mediastinal shadow). Improper placement can lead to complications such as pulmonary infarction, pulmonary artery perforation, or pneumothorax.
Lungs
The lungs are the last to be evaluated. A focused, consistent approach is best. Working from bottom to top, the lungs are compared to each other. With the exception of the slightly elevated right hemidiaphragm and the asymmetric cardiac shadow, the lungs should be similar in appearance at each level of inspection. Any differences in the density of the film or the vascular markings are an indication of possible pulmonary pathology.
Final Steps
Again, it must be emphasized that once the evaluation is complete, it is essential to evaluate old films and compare them with the current study. This comparison allows for a more detailed understanding of the pathology being evaluated and may affect management in a significant fashion (e.g., a rapidly growing mass will be managed differently than a mass that has been stable for a number of years). Before concluding the CXR assessment, the study should be reviewed with a radiologist or the final report should be reviewed. This way any subtle findings can be addressed and reviewed.
COMMONLY USED FINDINGS FOR EVALUATING LUNG DISEASE
Radiographic Densities
• The key to understanding findings on a CXR relies on understanding the five main densities detected by radiography. Air, Fat, Fluid, Calcium, Metal. The densities are listed from darkest (air) on a radiograph to the whitest (metal). Metal attenuates the x-ray beam the most while air attenuates it the least.
• Only by juxtaposing two different densities, (e.g., heart and lung) can one see borders. Knowledge of normal borders allows for distinction from pathology. When a normal border is lost or a new border is present, pathology is suspected.
Radiographic Signs
Another basic tenet is the understanding that certain findings are frequently associated with a specific disease process. This association is often referred to as a sign.
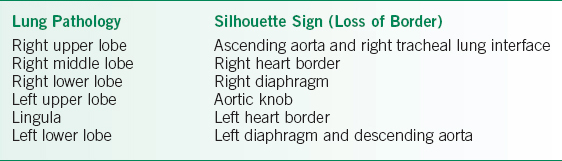
TABLE 1-1 ANATOMIC LOCATIONS OF SILHOUETTE SIGNS
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


