21 Small Vessel and Diffuse Disease
 Pathophysiologic Considerations
Pathophysiologic Considerations
in which ΔP is the pressure difference across the stenosis, r is the minimal lumen radius of the stenotic segment, η is blood viscosity, and l is the length of the lesion.1 Because flow across the lesion varies in proportion to the fourth power of radius but only as a first power of length, lesion length would be expected to exert relatively little impact on trans-lesional flow for discrete (e.g., <5 mm long) stenoses. However, as the length of a stenosis increases, for example, from 5 to 25 mm, a fivefold drop in blood flow across the stenosis would occur. It is essential that physicians performing coronary angiography or angioplasty understand this basic concept.2 Poiseuille’s law relates to flow of fluids through cylindrical tubes in well-controlled experimental settings. It does not take into consideration complexities of human coronary artery disease (CAD) such as plaque irregularity and eccentricity, nonlaminar and pulsatile flow, vasoactive properties of the arterial wall, and the potential for compensatory dilation. There is experimental evidence that lesion length has an important physiologic significance. Short, 40% to 60% coronary narrowings in a canine model, with no major resting hemodynamic effects, significantly reduced flows when stenosis length was increased to 10 and 15 mm. The hemodynamic effects of a 15-mm long, 40% to 60% stenosis were similar to those of a discrete 90% narrowing.3
Comparison of Various Stent Designs for Treatment of Long Lesions
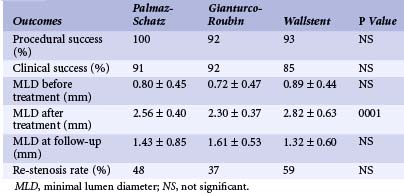
Data on the relative short-term and long-term efficacies of multiple overlapping stents versus placement of a single long stent are currently lacking, although the latter approach certainly provides potential advantages from the standpoint of procedure duration. The relationship between stent design and re-stenosis rates also remains incompletely defined. In an attempt to address these issues, the acute and chronic outcomes of various stents (Palmaz-Schatz, Gianturco-Roubin, and Wallstent) implanted in 148 lesions longer than 20 mm at Kokura Memorial Hospital between June 1990 and December 1995 were analyzed. Cases involving bypass grafts and acute myocardial infarction (MI) were excluded; only lesions that could be fully covered by the stent(s) were considered. Because the conventional Palmaz-Schatz stent was available only in short lengths, all Palmaz-Schatz stents included in this analysis involved the use of multiple stents. Palmaz-Schatz stents were used to treat 70 lesions, the Gianturco-Roubin stent was used for 38 lesions, and the Wallstent was used for 40 lesions. Although the average lesion length was greater than 30 mm for all stents, the Wallstent was typically used for lesions greater than 40 mm. In this nonrandomized comparison, the reference diameter was significantly greater in the Wallstent group, and Gianturco-Roubin stents were used most frequently for failed percutaneous transluminal coronary angioplasty (PTCA). The use of multiple stents was undertaken in 100% of the Palmaz-Schatz group, 44% of the Gianturco-Roubin group, and 40% of the Wallstent group. Procedural success (>50% improvement in vessel narrowing) and freedom from in-hospital complications were independent of stent design. Stent thrombosis occurred in 4.3% of the Palmaz-Schatz group but was not observed in either the Gianturco-Roubin or the Wallstent group. Quantitative angiography demonstrated a significantly larger immediate postprocedural minimum luminal diameter (MLD) in the Wallstent group, consistent with the larger reference vessel diameter in these patients. Six-month angiography, conducted in 97% of patients, demonstrated no significant differences in MLD among the groups. Binary re-stenosis rates were high in all groups: 48% for the Palmaz-Schatz stent, 37% for the Gianturco-Roubin stent, and 59% for the Wallstent groups. Repeat target lesion revascularization (TLR) was required in 31%, 20%, and 40%, respectively. Analysis of MLD demonstrated that late loss indices for the Palmaz-Schatz stent and the Wallstent were uniformly high, even though the initial acute gain was large. In contrast, the smaller acute gain in the Gianturco-Roubin group was compensated for by a more moderate degree of late loss (Table 21-1). In summary, although acute results with all stents in the treatment of lesions greater than 20 mm in length were acceptable, the incidence of late renarrowing was substantial regardless of the type of stent examined. A wide variety of newer stent designs are currently undergoing clinical testing. Follow-up studies are needed to determine if these new designs afford re-stenosis benefits over those of the first-generation stents.
New Generation Long Stents
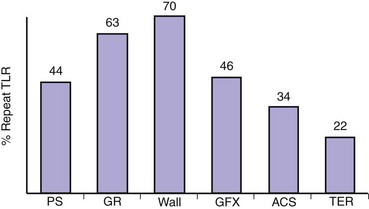
The late outcomes of various new long stents (GFX, ACS multi-link, Terumo) implanted in 211 lesions greater than 20 mm at the Kokura Memorial Hospital between January 1997 and December 2000 were analyzed. GFX long stents (30 mm) were used to treat 76 lesions, the acute coronary syndrome (ACS) multi-link long stent (35 mm) was used for 42 lesions, and the Terumo long stent was used for 93 lesions (30 mm: 65 lesions, 40 mm: 28 lesions). Binary re-stenosis rates remained high when compared with short lesions in all groups: 40.6% for the GFX long stent, 37.5% for the ACS multi-link long stent, and 33.3% for the Terumo long stent. Full-cover stenting of long lesions is likely to give rise to diffuse ISR. Treatment of diffuse ISR remains exceedingly problematic. Recurrent rates of 42% to 80% frequently necessitate multiple additional PTCA procedures and often bypass surgery.4,5 The diffuse ISR was an independent predictor of long-term outcome after coronary stenting. Angiographically discernible diffuse ISR was observed in 44% of the multiple Palmaz-Schatz stent group, 50% of the Gianturco-Roubin stent group, 59% of the Wallstent group, 64% of the GFX long stent group, 39% of the ACS long stent group, and 38% of the Terumo long stent group. Thus, repeat TLR was required in 44%, 63%, 70%, 46%, 34% and 22%, respectively (Fig. 21-1).
Full-Cover Stenting versus Spot Stenting for Treatment of Long Lesions
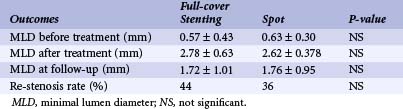
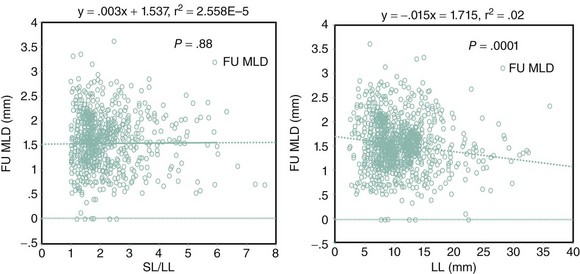
Colombo and colleagues have described a strategy to treat discrete high-grade disease within moderately diseased vessels; this strategy, called spot stenting, consists of implantation of a short stent only in discrete segments of a long lesion, where intracoronary ultrasound criteria were not satisfied (cross-sectional area >5.5 mm2). With this technique, 96% procedural success and a re-stenosis rate of 17% were obtained.6 The long-term outcomes of patients with lesions greater than 20 mm undergoing single (spot stenting) or multiple stent (full-cover stenting) therapy at the Kokura Memorial Hospital were analyzed. Of 95 consecutive patients treated with the Palmaz-Schatz stent, multiple stents were used in 62 and single stents in 33. Although there were no significant differences among the two groups with regard to patient and lesion characteristics, the single-stent group contained significantly more emergency cases, and the final dilation pressures were also significantly lower. Postprocedure MLD for the multiple-stent and single-stent groups did not differ significantly, and late angiography also showed no significant differences. Neither re-stenosis rates (44% and 36%) nor the rates of the need for repeat TLR (17% and 17%) were significantly different (Table 21-2). Many reports found that long stent length was associated with an increased frequency of late ISR.7 If stent length was the only determinant of re-stenosis, spot stenting might be advantageous and would be an appropriate treatment. Conversely, if lesion length is also a factor, using long stents to completely cover the diseased segment might be preferable. NACI investigators have suggested that stenting of long coronary lesions (>20 mm) involves significantly higher rates of the need for repeat TLR than more discrete lesions.8 In the series by Kastrati and colleagues, multivariate analysis of both binary re-stenosis and late lumen loss demonstrated that lesion length was an independent risk factor for re-stenosis. The risk was further increased by the multiplicity of implanted stents.9 To evaluate the impact of stent length on late angiographic outcome with coronary stent implantation, 6-month follow-up quantitative coronary angiograms (QCAs) of all consecutive 926 lesions, disregarding length treated with a single coronary stent in native arteries, between September 1999 and March 2000 at the Kokura Memorial Hospital was analyzed. There was no significant relation between the stent length–lesion length ratio and late angiographic outcome; the late angiographic outcome did correlate significantly to lesion length rather than to stent length (Fig. 21-2). Thus, covering the lesion with the least number of nonoverlapping stents might reduce the risks of re-stenosis.
Summary
From currently available observational data, stent implantation in long stenoses is associated with re-stenosis rates twice as high as those seen when single stents are used to treat discrete lesions. This fact might be the cause of the lower rate of event-free survival of patients receiving multiple stents.10,11 Long lesions are also significantly more prone to re-stenosis compared with short lesions following balloon angioplasty, but when re-stenosis occurs within stents, the prospects for successful long-term control are poorer. Although still incompletely defined, recurrent re-stenosis rates as high as 80% have been reported following balloon angioplasty for diffuse ISR. Despite these concerns, the use of multiple stents to treat long lesions is a commonplace occurrence in current interventional practice, and several long (>15 mm) stents of various designs have recently been approved for use in the United States. Randomized clinical trials are clearly needed to document the superiority of this yet-untested approach to traditional long balloon angioplasty.
 Adjunctive Pharmacologic Treatment for Long Lesions
Adjunctive Pharmacologic Treatment for Long Lesions
Despite the various mechanical approaches discussed earlier, percutaneous revascularization of long lesions continues to be associated with increased risks of peri-procedural complications and late recurrence. It stands to reason that the potential benefits afforded by a variety of novel and emerging strategies aimed at increasing the safety of angioplasty, its long-term efficacy, or both may be especially evident in the setting of more complex lesion morphologies such as long lesions. A series of prospective clinical trials has recently demonstrated the efficacy of potent antagonists of the glycoprotein (GP) IIb/IIIa receptor for patients undergoing percutaneous revascularization. Administration of abciximab has significantly reduced the occurrence of acute ischemic events in the setting of both high-risk and low-risk PTCA; and the benefits persist at 3-year follow-up.12–15 Results of the IIb/IIIa Platelet Receptor Antagonist 7E3 in Preventing Ischemic Complications (EPIC) Trial have been analyzed partially. The benefits of abciximab during angioplasty are not diminished by the presence of adverse lesion characteristics, including lesion length. Because of their propensity to increased late luminal loss, long lesions may be especially responsive to locally delivered ionizing radiation therapy. According to preliminary clinical data, it appears to be especially effective in reducing neointimal hyperplasia following arterial wall injury.16
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree