Small Abdominal Aortic Aneurysm
G. MATTHEW LONGO and B. TIMOTHY BAXTER
Presentation
A 73-year-old male is referred to the vascular surgery clinic for evaluation of a small abdominal aortic aneurysm (AAA). He received a CT scan of the chest/abdomen/pelvis for follow-up of his asbestosis. On the CT scan, it was appreciated that there was a 4.4-cm infrarenal AAA. His past medical history is significant for hypertension, hypercholesterolemia, atrial fibrillation, a transient ischemic attack, and asbestosis. He previously smoked 0.5 to 1.0 packs of cigarettes/day for 60 years. He denies any history of abdominal or back pain and continues working as an administrator. His physical examination reveals palpable femoral, popliteal, and tibial pulses bilaterally. There is no palpable abdominal mass or tenderness.
Differential Diagnosis
Small AAAs are often recognized incidentally by ultrasound or CT scan. These studies are performed for other abdominal/back complaints or as part of a screening program, when the discovery of an aneurysm is made. An AAA is defined as an abnormal dilatation of the aorta, with an increase in diameter of 50% or greater compared to its baseline size. Due to the fact, the baseline size is difficult to ascertain, a maximal measurement of ≥30 mm is frequently utilized to define an AAA.
AAA prevalence increases with age, and studies have revealed that they are present in up to 9% of men over the age of 55. Besides male gender, other risk factors include a history of smoking and a family history of AAA in a first-degree relative. Physical examination is notoriously unreliable for detection of AAA. However, both abdominal ultrasound and CT angiography exhibit a high degree of accuracy in detection. Ultrasound is generally regarded as the screening study of choice, due to cost, a relatively high specificity and sensitivity for detection, and its noninvasive nature.
Workup
On initial presentation, the most important elements of the workup include a complete history and physical examination and a discussion with the patient regarding the diagnosis of an AAA and what this entails. The vast majority of individuals presenting with a small AAA have no symptoms that can be attributed to the aneurysm. At this point, patients are understandably concerned about this new diagnosis. Thus, a definition of an aneurysm, coupled with a discussion of the natural history of the disease process, and time points for intervention are generally provided. Conveying the gradual progression of the disease and the ability to safely monitor growth are helpful in allaying anxiety. The patient also needs to know the signs and symptoms of an expanding or rupturing aneurysm.
After obtaining a detailed history and physical, a review of the available imaging is done. If there has not been a CT angiogram performed, this is usually advisable since it removes the size variability of ultrasound measurements and enables the surgeon to evaluate the branch vessels of the aorta and the extent of the aneurysm. CT also will better define the relationship to the renal arteries and demonstrate internal iliac aneurysms that may not be found on ultrasound. A compete blood count and basic metabolic profile allow for assessment of renal function and hemoglobin, platelet, and electrolyte abnormalities.
Other important elements of the workup involve a discussion with the patient regarding long-term follow-up. It is known that AAAs enlarge over time, with pooled estimates of AAA growth of about 2.5 mm/year. However, among individual patients, there is marked variation. Baseline diameter (smaller aneurysms grow at slower rates) is the most important determinant of growth rate. Continued smoking increases growth rate by approximately 10%/year, while diabetes is associated with slower growth. Since the aneurysm will remain asymptomatic even as it expands, both the patient and the physician need to remain committed to a long-term follow-up plan.
In the present case of a 74-year-old male with a 4.4-cm AAA, his CT scan demonstrates a fusiform, 4.4-cm infrarenal AAA (Fig. 1). The size of the aneurysm indicates that it has a low risk of rupture, and the recommendation is for surveillance. The rates of progression of AAA were discussed, as were the various treatment options if his aneurysm grew to a size warranting repair. A long-term surveillance program was also explained to him. He was also informed of the signs and symptoms of aortic rupture.
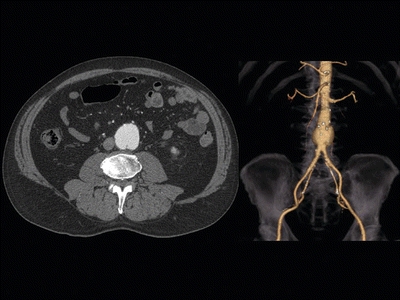
FIGURE 1 Axial cut of a CT scan documenting an infrarenal AAA and 3D reconstruction.



