67 Sleep Disorders and the Cardiovascular System
Sleep-Related Breathing Disorders
Sleep can be disrupted by several disorders (Box 67-1), many of which have not been extensively studied for their relationships to cardiovascular health. Patients presenting to a sleep disorders center are typically those with sleep-related breathing disorders. Common sleep problems including obstructive sleep apnea (OSA), central sleep apnea (CSA), and obesity hypoventilation can adversely impact cardiovascular health. Sleep-related breathing patterns, such as Cheyne-Stokes respiration (CSR), may reflect underlying cardiovascular issues. These disorders offer an opportunity to identify predisposing and exacerbating factors of cardiovascular disease and improve long-term risks.
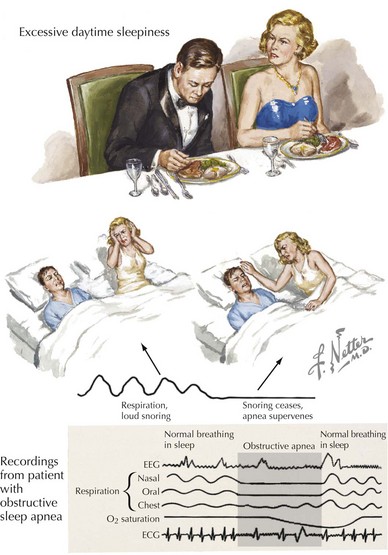
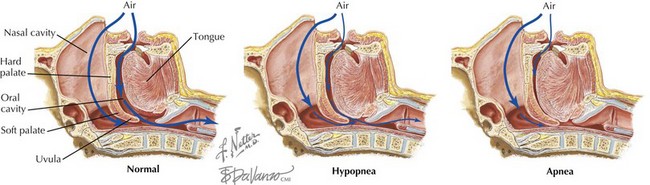
Obstructive Sleep Apnea
OSA is defined by repetitive collapse of upper airway structures for 10 seconds or longer, causing cessation of airflow in the setting of continued respiratory effort (Fig. 67-1). These events are commonly accompanied by a decrease in the blood oxygen saturation and a constellation of clinical symptoms (Box 67-2). Significant pathophysiology is also seen with hypopnea events, defined as airflow diminished by more than 30% and oxygen desaturation of at least 4%. The number of apnea and hypopnea events per hour, termed apnea-hypopnea index (AHI), is used to determine disease severity (Table 67-1). Population studies estimate that 1 in 5 individuals has at least mild disease, being more prevalent in males. The mechanisms for both obstructive apnea and hypopnea are linked to airway compromise at one of three levels: the nose, the retroglossal and retropalatal regions, and the pharynx (Box 67-3; Fig. 67-2). Common factors associated with increased risk of OSA include male sex, older age, obesity, anatomically small airway, and others (Box 67-4).
| AHI | Apnea Severity |
|---|---|
| 0–5 | Normal |
| 5–15 | Mild |
| 15–29 | Moderate |
| ≥30 | Severe |
AHI, apnea-hypopnea index.