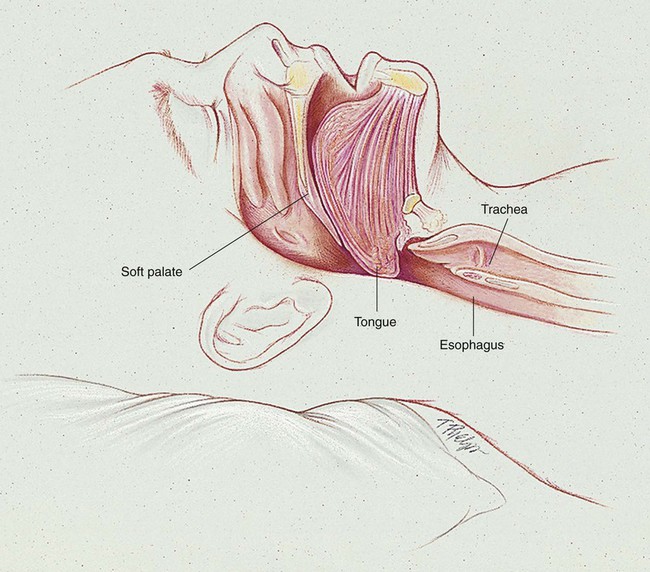
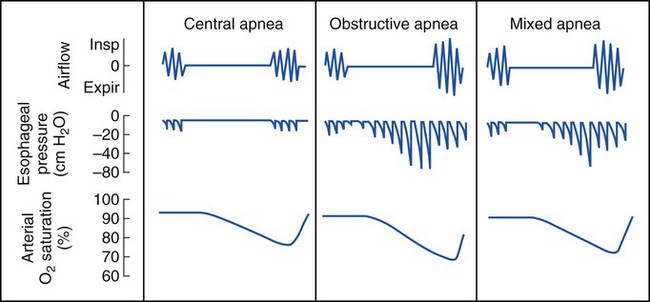
After reading this chapter, you will be able to: • List the anatomic alterations of the lungs associated with sleep apnea. • Describe the causes of sleep apnea. • Describe how a sleep study is performed. • List the cardiopulmonary clinical manifestations associated with sleep apnea. • Describe the meaning of the apnea-hypopnea index and oxygen desaturation index. • Describe the general management of sleep apnea. • Describe the clinical strategies and rationales of the SOAPs presented in the case study. • Define key terms and complete self-assessment questions at the end of the chapter and on Evolve. The following terminology (nosology) is now recommended to define the stages of sleep: REM sleep periods last 5 to 40 minutes and recur approximately every 60 to 90 minutes. The REM sleep periods lengthen and become more frequent toward the end of a night’s sleep. REM sleep constitutes about 20% to 25% of the total sleep time. Most studies show that it is more difficult to awaken a subject during REM sleep. Table 30-1 provides an overview of the electroencephalographic findings in the various stages of sleep. Table 30-1 It is estimated that more than 12 million people in the United States have OSA. OSA is caused by an anatomic obstruction of the upper airway in the presence of continued ventilatory effort (see Figure 30-1). During periods of obstruction, patients commonly appear quiet and still, as though they are holding their breath, followed by increasingly desperate efforts to inhale. Often the apneic episode ends only after an intense struggle. A snorting sound called “fricative breathing” may be heard at the end of the apneic periods. In severe cases, the patient may suddenly awaken, sit upright in bed, and gasp for air. These events are called confusional arousals. Patients with OSA usually demonstrate perfectly normal and regular breathing patterns during the wakeful period. In fact, a large number of patients with OSA demonstrate what is commonly called the Pickwickian syndrome (named after a character in Charles Dickens’s The Posthumous Papers of the Pickwick Club, published in 1837). Dickens’s description of Joe, “the fat boy” who snored and had excessive daytime sleepiness, included many of the classic features of what is now recognized as the sleep apnea syndrome. Box 30-1 provides common signs and symptoms associated with OSA. However, many patients with sleep apnea are not obese, and therefore clinical suspicion should not be limited to this group. Table 30-2 provides the more common risk factors associated with OSA. Table 30-2 Risk Factors Associated with Obstructive Sleep Apnea CSA is associated with cardiovascular, metabolic, and central nervous system disorders. A few brief central apneas normally occur with the onset of sleep or the onset of REM sleep. CSA, however, is diagnosed when the frequency of the apnea or hypopnea episodes is excessive (more than 30 in a 6-hour period). Box 30-2 provides a listing of clinical disorders associated with CSA.
Sleep Apnea
Normal Sleep Stages
REM Sleep
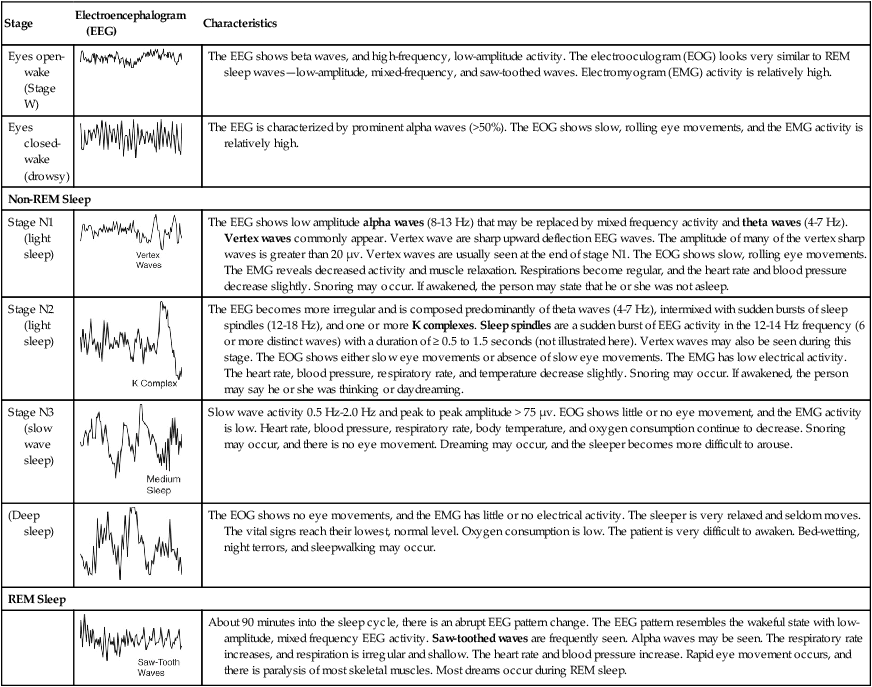
Stage
Electroencephalogram (EEG)
Characteristics
Eyes open-wake (Stage W)
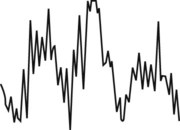
The EEG shows beta waves, and high-frequency, low-amplitude activity. The electrooculogram (EOG) looks very similar to REM sleep waves—low-amplitude, mixed-frequency, and saw-toothed waves. Electromyogram (EMG) activity is relatively high.
Eyes closed-wake (drowsy)

The EEG is characterized by prominent alpha waves (>50%). The EOG shows slow, rolling eye movements, and the EMG activity is relatively high.
Non-REM Sleep
Stage N1 (light sleep)
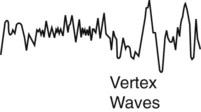
The EEG shows low amplitude alpha waves (8-13 Hz) that may be replaced by mixed frequency activity and theta waves (4-7 Hz). Vertex waves commonly appear. Vertex wave are sharp upward deflection EEG waves. The amplitude of many of the vertex sharp waves is greater than 20 µv. Vertex waves are usually seen at the end of stage N1. The EOG shows slow, rolling eye movements. The EMG reveals decreased activity and muscle relaxation. Respirations become regular, and the heart rate and blood pressure decrease slightly. Snoring may occur. If awakened, the person may state that he or she was not asleep.
Stage N2 (light sleep)
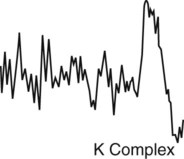
The EEG becomes more irregular and is composed predominantly of theta waves (4-7 Hz), intermixed with sudden bursts of sleep spindles (12-18 Hz), and one or more K complexes. Sleep spindles are a sudden burst of EEG activity in the 12-14 Hz frequency (6 or more distinct waves) with a duration of ≥ 0.5 to 1.5 seconds (not illustrated here). Vertex waves may also be seen during this stage. The EOG shows either slow eye movements or absence of slow eye movements. The EMG has low electrical activity. The heart rate, blood pressure, respiratory rate, and temperature decrease slightly. Snoring may occur. If awakened, the person may say he or she was thinking or daydreaming.
Stage N3 (slow wave sleep)
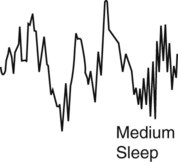
Slow wave activity 0.5 Hz-2.0 Hz and peak to peak amplitude > 75 µv. EOG shows little or no eye movement, and the EMG activity is low. Heart rate, blood pressure, respiratory rate, body temperature, and oxygen consumption continue to decrease. Snoring may occur, and there is no eye movement. Dreaming may occur, and the sleeper becomes more difficult to arouse.
(Deep sleep)
The EOG shows no eye movements, and the EMG has little or no electrical activity. The sleeper is very relaxed and seldom moves. The vital signs reach their lowest, normal level. Oxygen consumption is low. The patient is very difficult to awaken. Bed-wetting, night terrors, and sleepwalking may occur.
REM Sleep
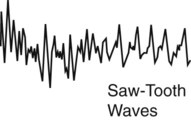
About 90 minutes into the sleep cycle, there is an abrupt EEG pattern change. The EEG pattern resembles the wakeful state with low-amplitude, mixed frequency EEG activity. Saw-toothed waves are frequently seen. Alpha waves may be seen. The respiratory rate increases, and respiration is irregular and shallow. The heart rate and blood pressure increase. Rapid eye movement occurs, and there is paralysis of most skeletal muscles. Most dreams occur during REM sleep.
Types of Sleep Apnea
Obstructive Sleep Apnea
Excess weight
More than 50% of the patients diagnosed with obstructive sleep apnea are overweight. It is suggested that fat deposits around the upper airway may obstruct breathing.
Neck size
Obstructive sleep apnea is often seen in the patients with large neck size. A neck circumference greater than 17 inches increases the risk for obstructive sleep apnea.
Hypertension
Obstructive sleep apnea is commonly seen in patients with high blood pressure.
Anatomic narrowing of upper airway
Common causes of anatomic narrowing of the upper airway include excessive pharyngeal tissue, enlarged tonsils or adenoids, deviated nasal septum, laryngeal stenosis, and vocal cord dysfunction.
Chronic nasal congestion
Obstructive sleep apnea occurs twice as often in patients with chronic nasal congestion from any cause.
Diabetes
Patients with diabetes are three times more likely to have obstructive sleep apnea than healthy individuals.
Male sex
Men are twice as likely to have obstructive sleep apnea as women.
Age older than 65 years
Obstructive sleep apnea is two to three times greater in people older than 65 years.
Age under 35 years, and black, Hispanic, or Pacific Islander heritage
Among individuals under the age of 35, the incidence of obstructive sleep apnea is greater in blacks, Hispanics, and Pacific Islanders.
Menopause
The risk of obstructive sleep apnea is greater after menopause.
Family history of sleep apnea
Individuals who have one or more family members who have obstructive sleep apnea are also at greater risk for developing obstructive sleep apnea.
Alcohol, sedatives, or tranquilizers
Depressive agents relax the muscles of the upper airway.
Smoking
Smokers are almost three times more likely to develop obstructive sleep apnea.
Central Sleep Apnea
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree