Sinus Dysfunction
Sinus Arrhythmia
Sinus arrhythmia occurs in young and healthy individuals and is not a form of sinus node dysfunction. Sinus arrhythmia is characterized by variation in cardiac cycle length. Variation in cycle length is defined as a 120-msec or 10% change between the shortest and longest cycles.1 Usually, the P-wave morphology is invariable, and the PR interval is constant.
Sinus arrhythmia can cause light-headedness and syncope if pauses between sinus beats are long enough.
Sinus arrhythmia is classified into respiratory and nonrespiratory types.
Respiratory Sinus Arrhythmia
Inhibition of vagal tone during inspiration causes shortening of cardiac cycle length. On expiration, the cycle lengthens.
Nonrespiratory Sinus Arrhythmia
Phasic variation in cycle length is unrelated to the respiratory cycle. This may occur in patients who are taking digitalis.
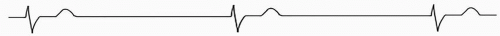
Wandering Atrial Pacemaker
This is considered a variant of sinus arrhythmia in which the dominant pacemaker gradually wanders from the sinus node to a latent pacemaker in the atrium or AV junction. This is considered normal physiology.
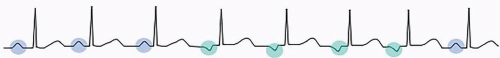 FIGURE 2.2 ECG appearance of a wandering atrial pacemaker. Changes in P-wave morphology and cycle length are typically more gradual than what is depicted here. |
As the cardiac cycle lengthens, the PR interval shortens, and the P wave changes morphology to become negative. As the cardiac cycle shortens, the sinus node takes over again, and the sinus P wave reappears.
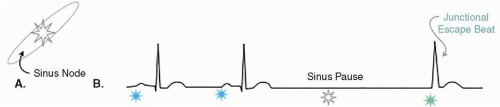
Sinus Arrest
In sinus arrest, the sinus node fails to spontaneously fire and produce an impulse. This results in a pause (absent P-QRS-T). The pause can be terminated by an escape beat. The escape beat occurs at a random time, resulting in a pause that is not a multiple of the preceding P-P interval. Technically, a pause requires at least a 2-second period during which sinus node activity (P waves) is absent.
The sinus node may consistently fail to fulfill its role as pacemaker. Ventricular activation then comes from pacemaker cells in the AV junction or ventricles. The resultant rhythm is typically a junctional or ventricular escape rhythm.
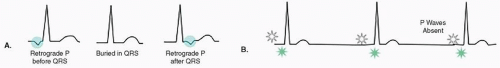
Junctional Escape Rhythm
The QRS complexes in a junctional escape rhythm are narrow. The rate is typically 40 to 60 bpm. P waves may be absent or appear inverted as retrograde P waves before or after QRS complexes.
Sinoatrial Exit Block
The sinus node may generate an impulse, but this impulse may fail to propagate to the atria and appear on the ECG as a dropped P-QRS-T complex.
Causes
Increased vagal tone, medications, myocardial infarction, fibrosis, and myocarditis can cause SA exit block.1
Subtypes
Like conduction block classification in the AV node, sinoatrial block can be classified into first, second (types I and II), and third degree block.
First Degree SA Block
The time from the sinus impulse to exit to the atrium is prolonged. Because the sinus impulse itself is not represented on the EKG, there is no way to diagnose this electrocardiographically.
Second Degree SA Block
Type I
A progressive prolongation of sinoatrial conduction is represented by a shortening of the P-P interval prior to a pause. The duration of the pause is less than twice the duration of the shortest cycle length. The cycle following the pause is longer than that preceding the pause. Persistent type 1 second degree AV block can appear as grouped beating.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree