More patients who are receiving therapy with a left ventricular assist device (LVAD) also have an implantable cardioverter-defibrillator (ICD). The aim of the present study was to describe the outcomes and device interactions of simultaneous therapy with an ICD and a LVAD. We evaluated 76 patients with class IV heart failure (age 52 ± 12 years, left ventricular ejection fraction 0.13 ± 0.05%, 88% men, 61% nonischemic cardiomyopathy) with both an ICD and a LVAD. The median follow-up with both devices was 156 days. A LVAD with a pulsatile and continuous flow pump was used in 53 (70%) and 23 (30%) patients, respectively. Of the 76 patients, 12 (16%) received a total of 54 ICD therapies. Of the ICD therapies, 88% were appropriate. Of the 76 patients, 55 (72%) underwent heart transplantation a median of 146 days after LVAD implantation. Twelve patients (16%) died during simultaneous ICD and LVAD therapy. Interactions between the LVAD and ICD occurred in 2 patients (2.7%) with continuous flow pumps (HeartMate II). In both cases, telemetry failure occurred after LVAD implantation with 2 different models of ICDs from the same manufacturer. No ICD therapies occurred because of device-related interactions. In conclusion, simultaneous ICD and LVAD therapy in patients with severe congestive heart failure is safe and clinically feasible. Interactions between the devices are uncommon and appear limited to specific models of ICDs.
Nonpharmacologic advances have emerged to treat the most serious sequelae of congestive heart failure: the implantable cardioverter-defibrillator (ICD) to prevent sudden death from ventricular arrhythmias and left ventricular assist devices (LVADs) for advanced pump failure. During the past 25 years, the ICD has become the mainstay of sudden cardiac death prevention for patients with advanced congestive heart failure. More recently, LVADs have emerged as an important treatment option for advanced congestive heart failure, both as a bridge to cardiac transplantation and as destination therapy. It is becoming increasingly common for patients with LVADs to also have ICDs. The objective of the present study was to evaluate the outcomes of patients with both LVADs and ICDs and to determine the frequency of device-related interactions.
Methods
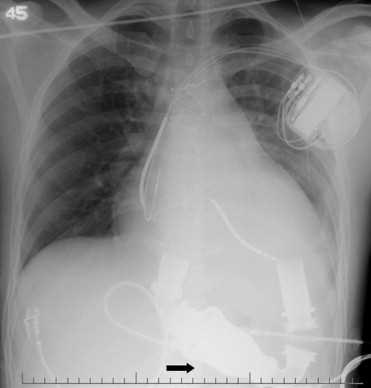
The present study was conducted at the University of Michigan Medical Center (Ann Arbor, Michigan). The University of Michigan institutional review board approved the study. The databases maintained by our institution were used to identify eligible patients from October 1996 to December 2007. All patients who had undergone LVAD therapy with a concomitant ICD were analyzed ( Figure 1 ). The data collected and analyzed included demographic and clinical variables, including New York Heart Association functional class, underlying heart failure etiology and duration, and device-specific information on the ICDs and LVADs.
The beginning of follow-up was the first day of simultaneous use of both devices. The last day of follow-up was December 31, 2007, the date of death, or the date of heart transplantation, whichever came first. The outcome variables analyzed were survival, ventricular arrhythmias, ICD therapies, and device-related complications and interactions. The number of hospitalizations and duration of hospitalization during simultaneous ICD-LVAD therapy were also analyzed. Sustained ventricular arrhythmias were defined as those that lasted >30 seconds or required cardioversion or defibrillation. All ventricular arrhythmias occurring after surgery were included. The initial hospitalization for LVAD placement (or ICD implantation if after LVAD implantation) was included for analysis, and hospitalization for orthotopic heart transplantation was excluded.
Continuous variables are presented as the mean ± standard deviation or as the median and interquartile range (IQR) in the case of a nongaussian distribution. For continuous variables, comparisons were made using Student’s t test or the Mann-Whitney U test, as appropriate. Discrete variables were compared using Fisher’s exact test. p Values <0.05 were considered statistically significant. Calculations were made using StatView software, version 5.0.1 (SAS Institute, Cary, North Carolina) and GraphPad Prism, version 5.0a (GraphPad Software, La Jolla, California).
Results
The data from 76 patients with both an ICD and LVAD were analyzed. The demographic data and clinical characteristics are summarized in Table 1 .
| Variable | Value |
|---|---|
| Age (years) | 52 ± 12 |
| Men | 67 (88%) |
| Body mass index (kg/m 2 ) | 27 ± 6 |
| Body surface area (m 2 ) | 2.1 ± 0.4 |
| Etiology of cardiomyopathy | |
| Ischemic | 30 (39%) |
| Nonischemic | 46 (61%) |
| New York Heart Association functional class IV | 76 (100%) |
| Heart failure duration (months) | |
| Mean ± SD | 70 ± 49 |
| Range | 3–210 |
| Left ventricular ejection fraction (%) | 13 ± 5 |
| Biventricular pacemaker | 25 (33%) |
| History of documented arrhythmia | |
| Sustained ventricular tachycardia or ventricular fibrillation | 20 (26%) |
| Nonsustained ventricular tachycardia | 26 (34%) |
| Atrial fibrillation | 11 (14%) |
Follow-up data were available for all 76 patients (100%). The median follow-up duration was 156 days (IQR 71 to 292). Of the 76 patients with an ICD implanted from July 1989 to May 2006, 57 (75%) received a dual-chamber ICD and 25 (33%) received an ICD with biventricular pacing. The ICD programming in the study population was not different from that for standard patients. The ICD manufacturers and models are listed in Table 2 .
| ICD | Patients (n) |
|---|---|
| Medtronic (Gem, Micro Jewel, InSync, Marquis, Entrust, Virtuoso) | 28 (37%) |
| Boston Scientific/Guidant/CPI (Contak, Ventak, Vitality) | 42 (55%) |
| Biotronik (Belos, Tachos) | 3 (4%) |
| St. Jude Medical/Ventritex (Atlas, Epic, Contour MD) | 3 (4%) |
Of the 76 patients, 71 (93%) received LVAD therapy a median of 591 days (IQR 183 to 946) after ICD implantation, and 5 (7%) received their ICD a median of 14 days (IQR 8 to 25) after LVAD placement.
Table 3 lists the types of LVADs implanted. Of the 76 patients, 53 (70%) received a pulsatile flow LVAD. Different versions of the HeartMate LVAD (Thoratec, Pleasanton, California) were used: the Vented Electric, its enhanced version, the XVE, and the Implantable Pneumatic version. These 3, as well as the Thoratec IVAD—all pulsatile flow pumps—were used.
| LVAD Model | Patients (n) |
|---|---|
| Pulsatile flow left ventricular assist device | 53 (70%) |
| HeartMateVE | 15 (20%) |
| HeartMate XVE | 34 (45%) |
| HeartMate IP-1000 | 1 (1%) |
| IVAD Thoratec | 3 (4%) |
| Continuous flow left ventricular assist device | 23 (30%) |
| HeartMate II | 22 (29%) |
| Micromed DeBakey | 1 (1%) |
Of the 76 patients, 23 (30%) received LVAD therapy using axial continuous flow pumps, such as the HeartMate II (Thoratec) and the Micromed DeBakey (MicroMed Technology, Houston, Texas). The first HeartMate II was implanted in August 2001.
Of the 76 patients, 55 (72%) underwent heart transplantation a median of 146 days (IQR 70 to 240) after LVAD implantation. Twelve patients (16%) died during simultaneous ICD and LVAD therapy. In these patients, circulation could be maintained, and the LVAD was turned off for medical reasons unrelated to pump failure, ventricular fibrillation, or a mechanical problem. The cause of death was renal failure in 4, multiorgan failure in 2, anoxic brain damage after LVAD implantation in 2, intracerebral hemorrhage in 1, ischemic stroke in 1, major gastrointestinal hemorrhage in 1, and death related to toxic megacolon due to Clostridium difficile in 1 patient.
The 76 patients in the series had a median of 2 hospitalizations during the follow-up period. No significant difference was found in the number of hospitalizations between the patients with pulsatile flow LVADs and those with continuous flow LVADs (p = 0.45). The overall median length of stay per patient was 35 days (IQR 19 to 79) in patients with pulsatile flow pumps compared to 27 days (IQR 17 to 59) in patients with continuous flow pumps (p = 0.28). The median percentage of days spent in the hospital compared to the follow-up duration was 34% (IQR 14% to 92%) in patients with pulsatile flow pumps and 16% (IQR 14% to 27%) in patients with continuous flow pumps (p = 0.02).
Of the 53 patients with pulsatile flow LVADs, 29 (55%) were rehospitalized after the initial LVAD implantation compared to 14 (61%) of 23 in the continuous flow LVAD group (p = 0.8). Of a total of 132 rehospitalizations, 40 (30%) occurred because of LVAD- or ICD-related problems. Table 4 summarizes the number and causes for rehospitalizations.
| Reason for Rehospitalization | Patients (n) |
|---|---|
| Total | 132 (100%) |
| Heart failure exacerbations | 10 (7.6%) |
| Implantable cardioverter-defibrillator therapies | 16 (12.1%) |
| Implantable cardioverter-defibrillator–related (without implantable cardioverter-defibrillator therapies) ⁎ | 6 (4.5%) |
| LVAD related † | 18 (13.6%) |
| Syncope/falls | 8 (6.1%) |
| Atrial fibrillation | 2 (1.5%) |
| Ventricular tachycardia/fibrillation | 4 (3.0%) |
| Gastrointestinal symptoms (bleeding, diarrhea, abdominal pain) | 11 (8.3%) |
| Renal failure | 5 (3.8%) |
| Anemia | 6 (4.5%) |
| Fever of unknown origin | 6 (4.5%) |
| Altered mental status | 4 (3.0%) |
| Cerebrovascular accident | 2 (1.5%) |
| Chest pain | 2 (1.5%) |
| Cellulitis | 2 (1.5%) |
| Hypoglycemia/hyperglycemia | 2 (1.5%) |
| Arteriovenous fistula | 3 (2.3%) |
| Other ‡ | 25 (18.9%) |
⁎ ICD-related rehospitalizations were due to generator replacement (n = 4) and pocket hematoma (n = 2).
† LVAD-related rehospitalizations were due to driveline infection (n = 6), replacement for end of life (n = 5), controller malfunction (n = 2), device malfunction (n = 1), device infection (n = 1), driveline dehiscence (n = 1), device-related bowel obstruction (n = 1), LVAD alarms (n = 1).
‡ Other hospitalizations were due to infections (pneumonia, urinary tract infections), admission for possible heart transplantation, heart catheterization, seizure, atrial fibrillation, radiofrequency ablation of ventricular tachycardia, clot in peripherally inserted central catheter.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


