Cardiovascular magnetic resonance (CMR) with extensive late gadolinium enhancement (LGE) is a novel marker for increased risk for sudden death (SD) in patients with hypertrophic cardiomyopathy (HC). Small focal areas of LGE confined to the region of right ventricular (RV) insertion to ventricular septum (VS) have emerged as a frequent and highly visible CMR imaging pattern of uncertain significance. The aim of this study was to evaluate the prognostic significance of LGE confined to the RV insertion area in patients with HC. CMR was performed in 1,293 consecutive patients with HC from 7 HC centers, followed for 3.4 ± 1.7 years. Of 1,293 patients (47 ± 14 years), 134 (10%) had LGE present only in the anterior and/or inferior areas of the RV insertion to VS, occupying 3.7 ± 2.9% of left ventricular myocardium. Neither the presence nor extent of LGE in these isolated areas was a predictor of adverse HC-related risk, including SD (adjusted hazard ratio 0.82, 95% confidence interval 0.45 to 1.50, p = 0.53; adjusted hazard ratio 1.16/10% increase in LGE, 95% confidence interval 0.29 to 4.65, p = 0.83, respectively). Histopathology in 20 HC hearts show the insertion areas of RV attachment to be composed of a greatly expanded extracellular space characterized predominantly by interstitial-type fibrosis and interspersed disorganized myocyte patterns and architecture. In conclusion, LGE confined to the insertion areas of RV to VS was associated with low risk of adverse events (including SD). Gadolinium pooling in this region of the left ventricle does not reflect myocyte death and repair with replacement fibrosis or scarring.
Contrast-enhanced cardiovascular magnetic resonance (CMR) with extensive late gadolinium enhancement (LGE) has emerged as a novel marker for identifying patients with hypertrophic cardiomyopathy (HC) at increased risk for adverse disease consequences. Utility of LGE as a risk marker is predicated on quantifying the amount of LGE relative to overall left ventricular (LV) mass although the significance attached to specific patterns or locations of LGE remains incompletely resolved. Since the initial descriptions of LGE in HC, 1 contrast-enhanced pattern has been of particular note, in which LGE is confined exclusively to the insertion areas of the right ventricle (RV) into anterior and/or inferior ventricular septum (VS). Indeed, this specific LGE pattern continues to be of interest given the increasing penetration of CMR into clinical cardiovascular practice. Therefore, in this substudy, we systematically assessed our large HC-CMR database to define the prevalence, clinical profile, and prognostic significance of this unique LGE pattern to patients with HC. To characterize the morphology of the LV wall at the point of RV wall insertion, histopathologic examination was performed in an independent group of hearts with HC and in appropriate controls.
Methods
We evaluated 1,669 patients with HC who were initially considered for CMR study at 7 HC centers from November 2001 to February 2010. A total of 376 patients were excluded from the cohort based on the following criteria: previous implantation of an internal cardioverter defibrillator (ICD) or other incompatible device, history of sustained ventricular tachycardia (VT)/ventricular fibrillation (VF), claustrophobia, known as associated obstructive coronary artery disease (including history of myocardial infarction or acute coronary event associated with increased cardiac enzymes or Q waves), other myocardial diseases, septal myectomy or alcohol ablation performed before CMR, and when complete follow-up could not be obtained (n = 7). Therefore, the final study group comprised 1,293 patients referred and eligible for CMR. This substudy is specifically confined to study the significance of LGE in the areas of RV wall insertion to LV and were selectively compared with a subgroup of patients without LGE, also taken from our large HC-CMR database, in which other aspects related to LGE in HC have been reported.
Follow-up of 3.4 ± 1.7 years was to the most recent evaluation (annual clinic visit or telephone interview) or death, as of January 2012. All CMR analyses were performed by the investigators blinded to clinical outcomes. This study was approved by the internal review board of the respective participating institutions, with patients agreeing to the use of their medical information for research purposes. All investigators had full access to and take full responsibility for the integrity of the data and have read and agreed to the manuscript as written.
Diagnosis of HC was based on CMR documentation of a hypertrophied and nondilated LV (LV wall thickness ≥15 mm in adults and the equivalent relative to body surface area in children) in the absence of another cardiac or systemic disease capable of producing a similar magnitude of hypertrophy. LV outflow tract obstruction was defined as a peak systolic instantaneous outflow gradient ≥30 mm Hg, assessed by continuous-wave Doppler echocardiography under conditions at rest.
Adverse HC-related events included sudden death (SD) events defined as unexpected collapse in patients who had previously had a relatively uneventful clinical course, appropriate ICD interventions triggered by VF or rapid VT (rate ≥180 beats/minute), symptom progression during follow-up to the New York Heart Association (NYHA) functional class III or IV (including heart transplant recipients), or HC-related heart failure death.
LV volume, mass, and ejection fraction were measured using standard volumetric techniques and analyzed with commercially available software (QMASS, v7.4; Medis Inc., Leiden, The Netherlands). LV chamber was assessed according to the American Heart Association 17-segment model. Maximal LV wall thickness was defined as the greatest dimension at any site within LV myocardium.
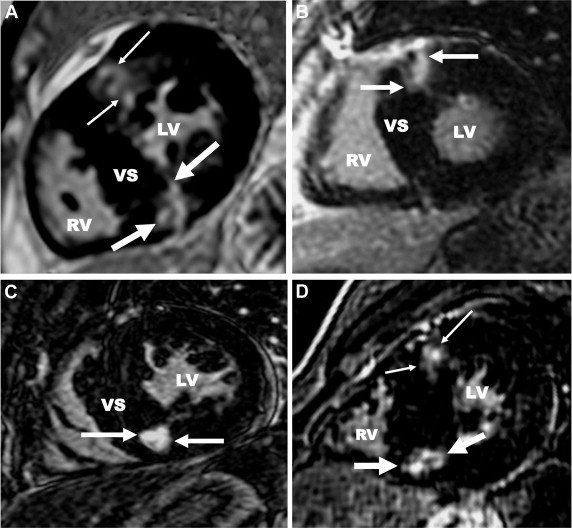
Images from all centers were transferred to a core laboratory (PERFUSE, Boston, Massachusetts) for centralized and blinded analysis. LGE images were first assessed visually for the presence and location of LGE by 2 experienced readers (RHC and EA), blinded to patient profiles and clinical outcome, with any disagreement adjudicated by a third expert reader (WJM). RV insertion point LGE was defined as a focal area confined to the junction of RV wall into anterior and/or posterior septum, as identified on the LV short-axis image stack ( Figure 1 ). Quantification of LGE in this region was performed by 1 expert reader (RHC) by manually adjusting a gray scale threshold to define areas of visually identified LGE. These areas were then summed to generate a total volume of LGE and expressed as a proportion of total LV myocardium (% LGE).
Twenty postmortem hearts from patients with HC and SD were examined, separate from the present clinical study cohort (age 25 ± 10 years; 16 men; heart weights, 481 ± 189 g). In addition, 20 control hearts (age 29 ± 8 years; 10 men; heart weights, 356 ± 80 g) from patients who died of a variety of cardiac (coronary artery disease in 6; valve disease in 2; conduction disease in 3; and anomalous origin of the coronary in 1 and myocarditis in 1) or noncardiac diseases (sepsis in 4 and cancer in 3) were examined.
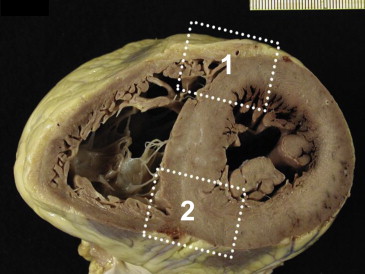
Full wall thickness tissue blocks were taken from the LV at the anterior and inferior areas of anatomic attachment of RV wall to VS ( Figure 2 ). Tissue was embedded in paraffin and sectioned at 8-μm thickness, stained with Masson’s trichrome, and inspected by light microscopy. The severity of interstitial fibrosis and myocyte disarray were assessed semiquantitatively on a scale of 0 to 3+.
Continuous and categorical data are expressed as mean (±SD) or n (%), respectively. Comparisons between groups were assessed with unpaired Student’s t , Wilcoxon rank-sum, chi-square, or Fisher’s exact test where appropriate. The prespecified primary clinical end point was a composite of adverse HC-related events including SD (including aborted cardiac arrest or appropriate ICD discharge for VT/VF) and adverse heart failure event (including symptom progression to NYHA class III/IV during the follow-up period, heart failure death, or heart transplantation).
Event-free survival curves were constructed using the Kaplan-Meier method, and differences between groups were examined using the log-rank test for equality of survivor functions. The relation between the presence or extent of LGE and the likelihood of subsequent events was further evaluated using univariate and multivariable Cox proportional hazards models. Variables entered into the multivariable model were age, maximal LV wall thickness, and ejection fraction. The proportional hazards assumption was tested graphically and with time-dependent covariates before proceeding. All analyses were performed with SAS 9.3 (SAS Institute, Cary, North Carolina).
Results
LGE was confined to the insertion area of RV wall and VS in 134 of 1,293 patients (10%) including 50 (4%) with LGE only at anterior septum, 36 (3%) only at posterior (inferior) septum, and 48 (3%) with LGE in both sites ( Table 1 , Figure 1 ). Extent of LGE in these 134 patients was 3.7 ± 2.9% of LV myocardial mass.
| Variable | RV Insertion Area LGE | Without LGE | P-Value |
|---|---|---|---|
| Number of patients | 134 | 745 | |
| Age (years) | 47±14 | 47±18 | 0.67 |
| Male | 88 (66%) | 468(63%) | 0.50 |
| Body surface area (g/m 2 ) | 2.0 ± 0.2 | 1.9±0.3 | 0.07 |
| NYHA class | 0.67 | ||
| I | 78 (58%) | 438(59%) | |
| II | 39 (29%) | 204(27%) | |
| III/IV | 17 (13%) | 103(14%) | |
| Atrial fibrillation | 23 (17%) | 72 (10%) | 0.02 |
| Basal LVOT gradient ≥ 30 mmHg | 37 (28%) | 182 (26%) | 0.66 |
| Number of HC risk factors | 0.6 ± 0.7 | 0.34±0.54 | <0.0001 |
| No conventional risk factors | 63 (47%) | 488 (69%) | |
| Nonsustained VT (ambulatory Holter) | 29 (22%) | 60 (9%) | |
| Unexplained syncope | 16 (12%) | 61 (9%) | |
| Family history of HC-SD | 30 (22%) | 114 (16%) | |
| LV thickness ≥ 30 mm | 10 (7%) | 8 (1%) | |
| ICD implantation | 24 (18%) | 88 (12%) | 0.09 |
| Ejection fraction | 66 ± 8 | 69±8% | <0.001 |
| LV wall thickness (mm) | 22 ± 5 | 18.1±4.0 | <0.001 |
| LV mass (g) | 163 ± 60 | 147±61 | 0.006 |
| LV mass index (g/m 2 ) | 82 ± 28 | 76±28 | 0.02 |
| LVED dimension (mm) | 53 ± 7 | 54±7 | 0.24 |
| LGE (g) | 5.7 ± 4.6 | N/A | NA |
| % LV with LGE | 3.7 ± 2.9 | N/A | NA |
| Location of LGE | N/A | NA | |
| RV at anterior septum only | 50 (37%) | ||
| RV at posterior septum only | 36 (27%) | ||
| RV at anterior and posterior insertion | 48 (36%) | ||
| Major clinical events in follow-up | NS | ||
| HC-related SD | 1 (0.8%) | 6 (0.9%) | |
| Aborted cardiac arrest | 2 (1.5%) | 2 (0.3%) | |
| ICD discharge (VT/VF) | 1 (0.8%) | 3 (0.4%) | |
| Heart failure death | 1 (0.8%) | 0 (0%) | |
| Heart transplant | 0 | 2 (0.3%) | |
| Progression to NYHA III/IV | 8 (6%s) | 59 (8%) |
The 134 study patients were 47 ± 14 years old (range 14 to 79); 88 (66%) were men ( Table 1 ). At baseline, most were asymptomatic or mildly symptomatic (n = 117 [87%] in NYHA functional classes I/II). Thirty-seven patients (28%) had LV outflow tract gradients of ≥30 mm Hg at rest.
Over the follow-up period, adverse disease-related events occurred in 13 patients (10%) with RV insertion area LGE, including 4 with SD events, 2 of whom had ≥1 conventional high-risk markers ( Table 1 ). Nine patients developed progressive heart failure symptoms to class III/IV or heart failure death (7%), including 2 with LV outflow obstruction (gradients 49 and 52 mm Hg, respectively; Table 1 ). In comparison, of 745 patients without LGE in the overall CMR cohort, adverse disease-related events occurred in 65 (9%).
Kaplan-Meier analysis showed no significant difference in the risk of adverse HC-related disease events between patients with RV insertion point LGE and those without LGE (log-rank p = 0.71; Figure 3 ). With multivariable analysis, after adjusting for a number of relevant demographic and disease-related variables known to influence risk in HC (i.e., age, maximal LV wall thickness, and LV ejection fraction), neither the presence nor extent of RV insertion LGE was an independent predictor for HC adverse events (adjusted hazard ratio [HR adj ] 0.82, 95% confidence interval [CI] 0.45 to 1.50, p = 0.53; HR adj 1.16/10% LGE, 95% CI 0.29 to 4.65, p = 0.83, respectively). There was also no difference in risk between those patients with LGE confined to either of the 2 RV insertion areas compared with patients with LGE present at both insertion points (HR 0.98, 95% CI 0.32 to 3.01; p = 0.98).
LV myocardium at the intersection of the RV wall and VS showed similar morphology in HC and in control hearts ( Figure 4 ). These areas were characterized by a loss of compact myocardium and markedly expanded extracellular space occupied predominantly by numerous myocytes in patterns of disarray embedded within areas of interstitial fibrosis ( Figure 4 ). Such anatomic features were not present in compact areas of the LV wall. Semiquantitative estimates of the degree and amount of cellular disorganization in HC exceeded that in controls for both the anterior (2.2 ± 0.7 vs 1.1 ± 0.3, p <0.001) and posterior (2.5 ± 0.6 vs 1.6 ± 0.5, p <0.001) RV insertion areas. Also, amounts of interstitial fibrosis were significantly greater in HC hearts than controls for anterior (1.5 ± 6 vs 0.5 ± 0.5, p <0.001) and inferior (1.7 ± 0.6 vs 1.0 ± 0.6, p <0.001) RV insertion areas ( Table 2 ).




