We sought to determine the clinical and physiologic significance of electrocardiographic complete right bundle branch block (CRBBB) and incomplete right bundle branch block (IRBBB) in trained athletes. The 12-lead electrocardiographic and echocardiographic data from 510 competitive athletes were analyzed. Compared to the 51 age-, sport type-, and gender-matched athletes with normal 12-lead electrocardiographic QRS complex duration, the 44 athletes with IRBBB (9%) and 13 with CRBBB (3%) had larger right ventricular (RV) dimensions, as measured by the basal RV end-diastolic diameter (CRBBB 43 ± 3 mm, IRBBB 38 ± 6 mm, normal QRS complex 35 ± 4 mm, p <0.001) and RV end-diastolic area (CRBBB 33 ± 5, IRBBB 27 ± 7, and normal QRS complex 23 ± 3 cm 2 ; p <0.001). Athletes with CRBBB also had a relative reduction in the RV systolic function at rest as assessed by the RV fractional area change and peak systolic tissue velocity. Finally, QRS prolongation was associated with parallel increases in interventricular dyssynchrony (basal RV to basal lateral left ventricular peak systolic tissue velocity time difference: CRBBB 112 ± 15, IRBBB 73 ± 33, normal QRS complex 43 ± 39 ms, p <0.001). Despite these findings, no athlete with CRBBB or IRBBB was found to have pathologic structural cardiac disease. In conclusion, among trained athletes, CRBBB and IRBBB appear to be markers of a structural and physiological cardiac remodeling triad characterized by RV dilation, a relative reduction in the RV systolic function at rest, and interventricular dyssynchrony.
At present, sparse data are available characterizing the disease prevalence, cardiac structure, and cardiac function in athletic patients with complete right bundle branch block (CRBBB) and incomplete right bundle branch block (IRBBB). We, therefore, conducted the present study with the following objectives. First, we determined the prevalence of CRBBB and IRBBB and their relations to underlying cardiac disease in a large cohort of collegiate athletes. Second, we compared the cardiac structure and function, including mechanical interventricular synchrony, among disease-free athletes with CRBBB, IRBBB, and normal 12-lead electrocardiographic QRS complex duration.
Methods
The present study population included United States university athletes previously enrolled to examine preparticipation cardiovascular disease screening. In brief, newly matriculated university athletes ≥18 years of age underwent a noninvestigational focused medical history and physical examination in accordance with the current American College of Cardiology/American Heart Association guidelines. Each participant provided a designation of primary ethnicity and underwent electrocardiography and transthoracic echocardiography at enrollment, as detailed in the following paragraphs. The training volume (hours/week) and training type (endurance vs strength) during the 8 weeks before enrollment was assessed for each participant. Prestudy period endurance activity was defined as running, cycling, swimming, rowing, or aerobic machine use at an effort sustainable for ≥20 minutes, and strength activity was defined as weight lifting, plyometric exercise, and sprint running drills. All participants had provided written consent before enrollment, and the Partners Human Research Committee had approved all aspects of the present study.
The echocardiographic and electrocardiographic (ECG) data were used to identify those with suspected underlying cardiac pathologic findings relevant to sport participation, as outlined in the Thirty-Sixth Bethesda Conference criteria and recent European Society of Cardiology guidelines. Those participants with suspected pathologic features underwent individualized, noninvestigational evaluation at the discretion of their physicians to confirm or exclude true cardiac disease. The prevalence of CRBBB and IRBBB and their relations to the underlying cardiac pathologic features were determined in the overall cohort.
A nested case-control approach was then used to compare the myocardial structure and function among disease-free participants with CRBBB, IRBBB, and normal QRS complex duration. Specifically, each participant with either CRBBB or IRBBB and with technically adequate echocardiographic images for complete assessment was matched to a participant with normal QRS complex duration of a similar age, gender, and sport type by a study investigator who was unaware of the echocardiographic and ECG results, other than the CRBBB/IRBBB status.
Electrocardiography was performed using standard 12-lead placement and equipment (MAC 5500, GE Healthcare, Milwaukee, Wisconsin) and was assessed by a study clinician who was unaware of the athlete sport type or echocardiographic data. Quantitative ECG measurements were made manually using calipers and included the heart rate, PR interval, and QRS duration. The QRS axis was measured automatically at acquisition and was confirmed by manual inspection.
Using the QRS duration, the participants were subdivided into the following categories: (1) CRBBB, (2) IRBBB, (3) non–RBBB QRS prolongation, and (4) normal QRS complex duration. CRBBB was defined as a QRS complex of ≥0.12 second in duration with an rSR′ morphology in lead V 1 and a qRS in lead V 6 . IRBBB was defined as a QRS duration of >0.1 but <0.12 second, with the same QRS morphology criteria. In each case, CRBBB and IRBBB morphology were inspected for features suggestive of the Brugada syndrome and arrhythmogenic right ventricular (RV) cardiomyopathy. Those with non–RBBB QRS prolongation, defined as a QRS duration of >0.1 second with morphology not meeting the CRBBB or IRBBB criteria, was excluded from the present analysis.
A commercially available system (Vivid-I, GE Healthcare) was used for all echocardiographic studies. All measurements were performed off-line with commercially available image processing software (EchoPac, version 6.5, GE Healthcare) in accordance with the current guidelines. The left ventricular (LV) end-diastolic volume, LV end-systolic volume, and LV ejection fraction were calculated using the modified Simpson’s biplane technique. The LV mass was estimated using the area-length method. The LV mass was also indexed to the body surface area, with the body surface area calculated using the Mosteller formula. The RV size was assessed in the apical 4-chamber view by measurement of the basal diameter, end-diastolic area, and end-systolic area. The RV fractional area change was calculated as the difference between the RV end-diastolic and RV end-systolic area divided by the RV end-diastolic area. The normal reference values for RV size and RV fractional area change were in accordance with the current guidelines. Examination of RV morphology was performed to identify features suggestive of arrhythmogenic RV cardiomyopathy in all participants. The myocardial tissue velocities were measured off-line from 2-dimensional color-coded tissue Doppler images, as detailed, and are reported as the average of 3 consecutive cardiac cycles. The echocardiographic evaluation was performed without knowledge of the ECG or clinical findings.
Interventricular synchrony was assessed as follows. The peak systolic longitudinal myocardial velocity (S m ) was measured by tissue Doppler imaging using a sampling window of 6 mm × 2 mm. The peak systolic longitudinal myocardial velocity was measured in the basal and mid-wall segments of the lateral left ventricle, interventricular septum, and the RV free wall using an apical 4-chamber view. The interval to peak myocardial systolic velocity (T s ) for each region was measured during the systolic ejection phase with reference to the onset of the QRS complex. Regional comparisons of the interval to the peak myocardial systolic velocity were made using the basal interventricular septum as the reference point.
The measurements are reported as the mean ± SD, unless otherwise specified. The prevalence of CRBBB and IRBBB was calculated as the percentage of the total cohort. Group-wise comparisons of the parameters among those with CRBBB, IRBBB, and normal QRS complex duration were performed using 1-way analysis of variance. Post hoc between-group comparisons were performed using Bonferroni’s method, and an adjusted p value of <0.01 was considered significant.
Results
The demographic, ethnic, and sport-type participation data are summarized in Table 1 . The cohort included 510 participants (311 men and 199 women), with a mean age of 19.0 ± 0.3 years and was primarily white (68%) in ethnicity. The participants performed 5.1 ± 2.2 hours/week of exercise training during the 8 weeks before enrollment, with the male participants as a group reporting more exercise training than the women. Sport-type participation was diverse and typical for a university-level competitive athletics program.
| Variable | Men (n = 311) | Women (n = 199) | Total |
|---|---|---|---|
| Age (years) | 19.0 ± 0.6 (18.0–22.1) | 18.8 ± 0.4 (18.0–21.4) | 19.0 ± 0.3 |
| Height (m) | 1.80 ± 0.15 (1.60–2.03) | 1.68 ± 0.09 (1.52–1.85) ⁎ | 1.76 ± 0.11 |
| Weight (kg) | 82 ± 16 (59–118) | 59 ± 12 (47–80) ⁎ | 73 ± 18 |
| Body mass index (kg/m 2 ) | 25.4 ± 1.8 (23.0–28.6) | 21.4 ± 1.6 (20.3–24.6) ⁎ | 24.1 ± 1.9 |
| Ethnicity | |||
| White | 205 (66%) | 143 (72%) | 349 (68%) |
| Asian | 32 (10%) | 28 (14%) | 60 (12%) |
| Black | 40 (13%) | 13 (7%) | 53 (10%) |
| Hispanic/Latino | 19 (6%) | 6 (3%) | 25 (5%) |
| Other | 15 (5%) | 8 (4%) | 23 (5%) |
| Preseason training exposure | |||
| Total training time (h/wk) | 5.5 ± 2.4 (0.0–12.5) | 4.3 ± 2.6 (0.0–11.9) ⁎ | 5.1 ± 2.2 |
| Strength training time (h/wk) | 3.1 ± 2.3 (0.0–10.4) | 1.1 ± 2.0 (0.0–5.5) ⁎ | 2.6 ± 2.3 |
| Aerobic training time (h/wk) | 2.4 ± 3.1 (0.0–12.0) | 3.2 ± 4.1 (0.0–10.8) | 2.5 ± 3.0 |
| Sport discipline | |||
| Football | 101 (32%) | 0 ⁎ | 101 (20%) |
| Crew | 62 (20%) | 26 (13%) ⁎ | 88 (17%) |
| Track-and-field | 38 (12%) | 21 (11%) | 59 (12%) |
| Soccer | 34 (11%) | 21 (11%) | 55 (11%) |
| Swimming | 27 (9%) | 23 (12%) | 50 (10%) |
| Ice hockey | 26 (9%) | 19 (10%) | 45 (9%) |
| Basketball | 26 (9%) | 17 (9%) | 43 (8%) |
| Lacrosse | 27 (9%) | 15 (8%) | 42 (8%) |
| Baseball | 25 (8%) | 0 ⁎ | 25 (5%) |
| Field hockey | 0 | 20 (10%) ⁎ | 20 (4%) |
| Softball | 0 | 16 (8%) ⁎ | 16 (3%) |
| Other | 12 (4%) | 6 (3%) | 18 (4%) |
CRBBB was documented in 13 (3%) of the 510 participants and IRBBB was found in 44 (9%). Of the 57 participants with CRBBB or IRBBB, 6 were excluded from additional analysis because of technically inadequate images for complete assessment (1 with CRBBB and 5 with IRBBB). Those with a normal QRS complex duration and matched for age, gender, and sport type (n = 51) were selected as a control group for the remaining eligible participants (12 with CRBBB and 39 with IRBBB).
The demographics, previous training volume, and quantitative ECG data for the 3 groups are listed in Table 2 . The groups had a similar mean age, gender composition, body surface area, and heart rate at rest. The CRBBB group had completed more exercise training than either the IRBBB or the normal QRS complex duration group before enrollment. The CRBBB group included rowers (n = 5), distance runners (n = 3), soccer players (n = 2), lacrosse players (n = 2), and American-style football (n = 1). The IRBBB group included rowers (n = 16), distance runners (n = 8), soccer players (n = 6), ice hockey players (n = 6), lacrosse players (n = 4), and American-style football players (n = 4). As expected, the mean QRS duration differed significantly across the groups. The mean QRS axis and PR interval durations were within the normal range for all groups but were both significantly greater among those with CRBBB than among those with IRBBB or a normal QRS complex duration.
| Variable | NQRS (n = 51) | IRBBB (n = 39) | CRBBB (n = 12) | p Value ⁎ |
|---|---|---|---|---|
| Age (years) | 19.3 ± 1.0 | 19.6 ± 0.6 | 19.7 ± 1.2 | NS |
| Men | 42/51 | 34/39 | 8/12 | NS |
| Body surface area (m 2 ) | 1.9 ± 0.2 | 2.0 ± 0.2 | 1.9 ± 0.2 | NS |
| Heart rate (beats/min) | 56 ± 8 | 57 ± 7 | 53 ± 3 | 0.008 |
| 12-Lead electrocardiographic QRS complex duration (ms) | 92 ± 8 | 107 ± 5 † | 125 ± 5 † ‡ | <0.001 |
| QRS axis (°) | 20 ± 11 | 32 ± 8 | 73 ± 12 † ‡ | <0.001 |
| PR interval (ms) | 152 ± 21 | 159 ± 28 | 189 ± 15 † ‡ | <0.001 |
| Previous training § (hours/wk) | 4.6 ± 1.2 | 5.0 ± 1.4 | 9.3 ± 1.8 † ‡ | <0.001 |
⁎ p Value derived from 1-way analysis of variance.
No participant with CRBBB or IRBBB had morphologic QRS features suggestive of Brugada syndrome or arrhythmogenic RV cardiomyopathy. Of the total 510 participants, 3 (0.6%) were found to have cardiac pathologic features that met the criteria for sport restriction; however, none of these participants had CRBBB or IRBBB. No cardiovascular events occurred during the ≥2 years of organized athletic participation after enrollment in any of the 507 participants cleared for sport.
The cardiac structural dimensions are listed in Table 3 . All 3 subgroups demonstrated an enlarged RV internal end-diastolic diameter compared to the normal reference values. Furthermore, an enlarging RV size, as reflected by the RV internal end-diastolic diameter and RV end-diastolic area paralleled the increases in QRS duration ( Figure 1 ). A nonsignificant trend was seen toward an increased LV wall thickness and LV chamber size as the QRS duration increased. These trends toward an increased LV wall thickness and chamber size were accompanied by significant increases in the LV mass across the 3 groups ( Figure 1 ) but no significant increases in LV relative wall thickness.
| Variable | Reference Value ⁎ | NQRS (n = 51) | IRBBB (n = 39) | CRBBB (n = 12) | p Value † |
|---|---|---|---|---|---|
| Right ventricular measurements | |||||
| Right ventricular basal internal dimension at end-diastole (mm) | 20–28 | 35 ± 4 | 38 ± 6 ‡ | 43 ± 3 ‡ § | <0.001 |
| Right ventricular end-diastolic area (cm 2 ) | 11–28 | 23 ± 3 | 27 ± 7 ‡ | 33 ± 5 ‡ § | <0.001 |
| Right ventricular end-systolic area (cm 2 ) | 7.5–16 | 13 ± 2 | 14 ± 4 | 21 ± 5 ‡ § | <0.001 |
| Left ventricular measurements | |||||
| Interventricular septum (mm) | 6.0–10.0 | 9.6 ± 0.6 | 9.9 ± 0.9 | 10.6 ± 0.9 | NS |
| Posterior wall thickness (mm) | 6.0–10.0 | 9.4 ± 0.6 | 9.6 ± 0.8 | 10.4 ± 0.6 | NS |
| Relative wall thickness | ≤0.42/≤0.42 | 0.39 ± 0.02 | 0.38 ± 0.01 | 0.38 ± 0.02 | NS |
| Left ventricular basal internal dimension at end-diastole (mm) | ≤53/≤59 | 49 ± 6 | 52 ± 4 | 55 ± 6 | NS |
| Left ventricular mass (g) | ≤162/≤224 | 211 ± 25 | 240 ± 29 ‡ | 281 ± 28 ‡ § | <0.001 |
| Left ventricular mass/body surface area (g/m 2 ) | ≤95/≤115 | 111 ± 17 | 121 ± 14 ‡ | 139 ± 16 ‡ § | <0.001 |
† p Values derived from 1-way analysis of variance.
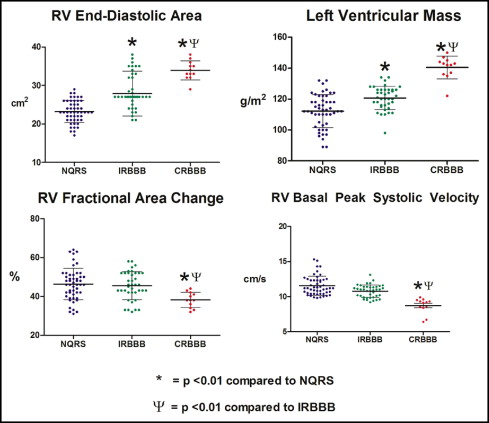
The indexes of RV and LV function are summarized in Table 4 . The LV ejection fraction and peak systolic longitudinal myocardial velocity of the basal and mid LV lateral wall were similar across the groups. In contrast, those with CRBBB had a significantly lower RV fractional area change and peak basal RV systolic longitudinal myocardial velocity than the participants with either IRBBB or a normal QRS complex duration ( Figure 1 ). Similarly, the peak systolic longitudinal myocardial velocity of the basal and mid-interventricular septum was significantly reduced across the groups with increasing QRS duration.
| Variable | Reference Value ⁎ | NQRS (n = 51) | IRBBB (n = 39) | CRBBB (n = 12) | p Value † |
|---|---|---|---|---|---|
| Right ventricular measurements | |||||
| Right ventricular fractional area change (%) | 32–60 | 46 ± 8 | 46 ± 9 | 38 ± 7 ‡ § | 0.02 |
| Right ventricular base peak systolic tissue velocity (cm/s) | NA | 11.4 ± 1.9 | 10.8 ± 1.7 | 8.8 ± 1.5 ‡ § | <0.001 |
| Right ventricular mid-peak systolic tissue velocity (cm/s) | NA | 9.5 ± 1.4 | 8.8 ± 2.0 | 6.3 ± 0.9 ‡ § | <0.001 |
| Left ventricular measurements | |||||
| Left ventricular ejection fraction (%) | >55% | 62 ± 4 | 62 ± 6 | 59 ± 5 | NS |
| Basal septum peak systolic tissue velocity (cm/s) | NA | 6.9 ± 1.0 | 6.1 ± 1.7 ‡ | 5.3 ± 1.1 ‡ § | 0.002 |
| Mid-septum peak systolic tissue velocity (cm/s) | NA | 5.3 ± 1.0 | 4.8 ± 1.1 | 3.2 ± 0.9 ‡ § | 0.005 |
| Basal lateral left ventricular peak systolic tissue velocity (cm/s) | NA | 7.0 ± 1.4 | 6.5 ± 1.9 | 6.1 ± 0.8 | NS |
| Mid lateral left ventricular peak systolic tissue velocity (cm/s) | NA | 6.9 ± 1.8 | 5.9 ± 2.0 | 5.5 ± 0.7 | NS |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


