High-density lipoprotein (HDL) cholesterol levels are a strong, independent inverse predictor of cardiovascular disease. The present study aimed to determine whether serum HDL cholesterol levels correlated with disease severity and clinical outcomes in patients with idiopathic pulmonary arterial hypertension (IPAH). The serum HDL cholesterol levels were measured in 76 Chinese patients with IPAH and 45 healthy controls, together with other clinical variables. Univariate and multivariate Cox proportional hazards analysis was performed to assess the prognostic value of HDL cholesterol and event-free survival. Event-free survival was estimated using the Kaplan-Meier method. Serum HDL cholesterol levels were significantly decreased in patients with IPAH compared with controls (1.0 ± 0.3 vs 1.5 ± 0.3 mmol/L; p <0.001). The serum HDL cholesterol levels decreased in proportion to the severity of World Health Organization functional class. Compared to the high HDL cholesterol group, the low HDL cholesterol group demonstrated a significantly lower 6-minute walking distance, cardiac index, mixed venous saturation, and arterial carbon dioxide pressure but significantly greater pulmonary vascular resistance and serum uric acid levels. The serum HDL cholesterol levels correlated positively with the cardiac index (r = 0.42; p = 0.002) and negatively with the pulmonary vascular resistance (r = −0.25; p = 0.04). Serum HDL cholesterol was independently related to event-free survival on multivariate Cox proportional hazards analysis. Kaplan-Meier survival curves according to the median HDL cholesterol value showed that lower HDL cholesterol levels were associated with lower event-free survival. In conclusion, serum HDL cholesterol levels might serve as an indicator of disease severity and prognosis in patients with IPAH.
Population studies have consistently shown that high-density lipoprotein (HDL) cholesterol levels are a strong, independent inverse predictor of cardiovascular disease. The protective effects of HDL cholesterol are most likely multifactorial, including reverse cholesterol transport to the liver, antioxidant properties, anti-inflammatory properties, protection of the endothelium, anticoagulant effects, and enhancement of the half-life of prostacyclin. Except for reverse cholesterol transport, all these mechanisms relate to the pathophysiology of pulmonary arterial hypertension (PAH). Recently, HDL cholesterol has been found to be lower in patients with PAH and to be associated with worse clinical outcomes. Dyslipidemia is a common metabolic disorder that results from the increasing prevalence of obesity. Compared with Western populations, Chinese patients have less obesity. If a lower HDL cholesterol level is simply a consequence of obesity, the potential relationship between HDL cholesterol and PAH in Chinese patients could be different. The aim of the present study was to determine whether circulating HDL cholesterol levels are depressed and associated with clinical outcomes in a cohort of Chinese patients with idiopathic PAH (IPAH).
Methods
The patients were recruited from Shanghai Pulmonary Hospital, which had a large number of “incident” patients with IPAH diagnosed from 2007 to 2009. IPAH was diagnosed according to the updated Dana Point clinical classification. A total of 82 patients with IPAH were referred to our institute from April 2008 to December 2009. Of these patients, 6 were excluded because of coronary risk factors (hypertension in 2 patients, coronary heart disease in 3, and hyperlipidemia in 1). The remaining 76 patients were enrolled in the present prospective cohort study. The demographic information, body mass index, systemic arterial pressure, 6-minute walking distance (6MWD), World Health Organization (WHO) functional class, echocardiographic parameters, serum markers, and hemodynamic parameters were determined at baseline during hospitalization. A total of 45 age-matched healthy volunteers served as controls.
The institutional ethics committee of Shanghai Pulmonary Hospital approved the study protocol, and all participants provided informed consent.
For measurement of serum HDL cholesterol, triglycerides, total cholesterol, uric acid, creatinine, fasting glucose, and total bilirubin, venous blood samples were drawn after an overnight fast within 1 week of the first diagnostic catheterization. No changes in the patients’ clinical status or PAH-active therapies occurred between blood sampling and cardiac catheterization. The serum HDL cholesterol levels were determined enzymatically using a commercial kit (Wako HDL cholesterol, Wako Pure Chemical Industries, Osaka, Japan). Low-density lipoprotein cholesterol was calculated using the Friedewald formula.
Right-sided heart catheterization was performed in all patients during hospitalization. The baseline hemodynamic variables, including systemic blood pressure, mean pulmonary arterial pressure, mean right atrial pressure, and mean pulmonary capillary wedge pressure, were measured in all patients. Cardiac output was measured in triplicate using the thermodilution technique with ice-cold isotonic sodium chloride solution. The cardiac index was calculated by dividing cardiac output by body surface area. Pulmonary vascular resistance was calculated by dividing mean pulmonary arterial pressure minus mean pulmonary capillary wedge pressure by cardiac output.
Event-free survival was estimated from the date of blood sampling to June 30, 2011 or cardiopulmonary death. Data were obtained during visits to the outpatient clinic or by telephone interview. Four end points were prospectively assessed: cardiopulmonary death, transplantation, hospitalization for right heart failure, and the addition of another active therapy for clinical worsening or a switch from oral PAH-active therapy to inhaled or intravenous iloprost for clinical worsening.
SPSS, version 13.0, software (SPSS, Chicago, Illinois) was used for statistical analysis. Numeric values are expressed as the mean ± SD. Comparisons of variables between 2 groups were made using unpaired t tests. Comparisons of serum HDL cholesterol levels among the study groups were made using 1-way analysis of variance, followed by Scheffe’s multiple comparison test. Correlations between the HDL cholesterol levels and hemodynamic or laboratory variables were calculated using Pearson’s correlation coefficients. Categorical data were assessed using a chi-square test or Fisher’s exact test, as appropriate. Univariate Cox proportional hazards analysis was performed to assess the prognostic value of each variable and event-free survival. Using a forward stepwise multivariate model, the prognostic power of the serum HDL cholesterol levels was compared with that of other significant parameters on univariate analysis. Event-free survival (defined as cardiopulmonary death, transplantation, hospitalization for right-heart failure, addition of another active therapy for clinical worsening or a switch from oral PAH-active therapy to inhaled or intravenous iloprost for clinical worsening) grouped by the median HDL cholesterol value was estimated using the Kaplan-Meier method and analyzed with the log-rank test. A p value ≤0.05 was considered significant.
Results
A total of 76 patients with IPAH and 45 control subjects were studied. No significant difference was found in age or body mass index between the 2 study groups. The demographic and clinical characteristics of the 2 groups at study entry are listed in Table 1 .
| Characteristic | IPAH (n = 76) | Control subjects (n = 45) | p Value |
|---|---|---|---|
| Age (years) | 37 ± 11 | 41 ± 7 | 0.06 |
| Women | 56 (74%) | 20 (56%) | 0.002 |
| Body mass index (kg/m 2 ) | 22 ± 3 | 22 ± 2 | 0.29 |
| 6-Minute walking distance (m) | 398 ± 114 | ND | — |
| World Health Organization functional class: | |||
| II | 43 (57%) | ND | — |
| III | 24 (32%) | ND | — |
| IV | 9 (12%) | ND | — |
| Mean pulmonary arterial pressure (mm Hg) | 63 ± 18 | ND | — |
| Mean right atrial pressure (mm Hg) | 8 ± 6 | ND | — |
| Cardiac index (L/min/m 2 ) | 2.5 ± 0.8 | ND | — |
| Pulmonary vascular resistance (Wood units) | 16 ± 7 | ND | — |
The mean duration of follow-up was 24 ± 9 months (median 25, range 1 to 39). No patient received a lung or heart–lung transplant during the follow-up period. No patient switched to another active therapy owing to adverse effects of the compound itself. Overall, 16 patients died; 8 patients died in our hospital from acute right heart failure with severe dyspnea, distention of the jugular vein, and fluid retention. Six patients died in their local hospitals with cardiogenic shock, and two patients died in their local hospitals from severe cardiac arrhythmias diagnosed by electrocardiography. Six patients were lost to follow-up, for a follow-up rate of 92%.
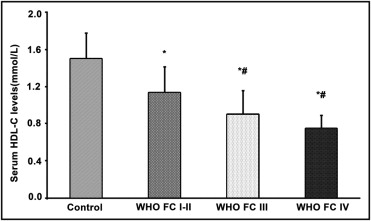
The serum HDL cholesterol levels were significantly decreased in patients with IPAH compared to those of the control subjects (1.0 ± 0.3 vs 1.5 ± 0.3 mmol/L, p <0.001). The serum HDL cholesterol levels were decreased in proportion to the severity of the WHO functional class ( Figure 1 ). The triglyceride/HDL cholesterol ratio was significantly increased in patients with IPAH compared to the control subjects (1.4 ± 0.9 vs 0.9 ± 0.6, p <0.001). The demographic characteristics, hemodynamic variables, biochemical markers, 6MWD, and blood gas data for patients with IPAH grouped according to the median serum HDL cholesterol value (1.02 mmol/L) are summarized in Table 2 . No significant differences were found between the high HDL cholesterol group (≥1.02 mmol/L) and the low HDL cholesterol group (<1.02 mmol/L) for age, gender, body mass index, serum creatinine, serum triglycerides, low-density lipoprotein, glucose, and PAH-active therapy (including vardenafil, sildenafil, bosentan, and iloprost). However, the 6MWD was significantly lower in the low HDL cholesterol group than in the high HDL cholesterol group, and the serum total bilirubin and serum uric acid levels were significantly higher ( Table 2 ). Echocardiography demonstrated that the prevalence of pericardial effusion was greater in the low HDL cholesterol group than in the high HDL cholesterol group. In addition, the heart rate and pulmonary vascular resistance were significantly greater in the low HDL cholesterol group, and the cardiac index, mixed venous oxygen saturation, and arterial carbon dioxide pressure were significantly lower in the low HDL cholesterol group than in the high HDL cholesterol group.
| Variable | HDL cholesterol (mmol/L) | p Value | |
|---|---|---|---|
| <1.02 (n = 37) | ≥1.02 (n = 39) | ||
| Age (years) | 39 ± 12 | 35 ± 10 | NS |
| Gender | NS | ||
| Male | 9 | 11 | |
| Female | 28 | 28 | |
| Body mass index (kg/m 2 ) | 22 ± 3 | 22 ± 4 | NS |
| Six-minute walking distance (m) | 351 ± 121 | 436 ± 92 | 0.001 |
| Serum total bilirubin (μmol/L) | 29 ± 18 | 20 ± 10 | 0.011 |
| Serum creatinine (μmol/L) | 74 ± 16 | 71 ± 17 | NS |
| Serum uric acid (μmol/L) | 454 ± 117 | 384 ± 115 | 0.013 |
| Blood glucose (mmol/L) | 4.7 ± 0.7 | 4.6 ± 0.8 | NS |
| Serum total cholesterol (mmol/L) | 3.5 ± 0.9 | 4.1 ± 0.8 | 0.002 |
| Serum triglyceride (mmol/L) | 1.4 ± 0.6 | 1.2 ± 0.5 | NS |
| Low-density lipoprotein (mmol/L) | 2.3 ± 0.8 | 2.5 ± 0.7 | NS |
| Serum triglyceride/high-density lipoprotein cholesterol ratio | 1.9 ± 1.0 | 1.0 ± 0.4 | <0.001 |
| Left ventricular end-diastolic dimension (mm) | 36 ± 6 | 38 ± 7 | NS |
| Left ventricular ejection fraction (%) | 65 ± 3 | 66 ± 5 | NS |
| Pericardial effusion | 11 (30%) | 4 (10%) | 0.045 |
| Heart rate (beats/min) | 88 ± 11 | 80 ± 16 | 0.02 |
| Mean right atrial pressure (mm Hg) | 9 ± 7 | 7 ± 5 | NS |
| Mean pulmonary arterial pressure (mm Hg) | 64 ± 17 | 61 ± 18 | NS |
| Mean pulmonary capillary wedge pressure (mm Hg) | 9 ± 4 | 9 ± 3 | NS |
| Cardiac index (L/min/m 2 ) | 2.1 ± 0.6 | 2.8 ± 0.8 | 0.001 |
| Pulmonary vascular resistance (Wood units) | 18 ± 7 | 14 ± 6 | 0.009 |
| Partial pressure of oxygen (mm Hg) | 67 ± 15 | 72 ± 15 | NS |
| Partial pressure of carbon dioxide (mm Hg) | 27 ± 4 | 31 ± 5 | 0.001 |
| Mixed venous oxygen saturation (%) | 55 ± 6 | 63 ± 7 | <0.001 |
| Active therapy | NS | ||
| Vardenafil | 9 (24%) | 13 (33%) | |
| Sildenafil | 19 (51%) | 16 (41%) | |
| Bosentan | 2 (5.4%) | 3 (7.7%) | |
| Iloprost | 4 (11%) | 2 (5.1%) | |
The serum HDL cholesterol levels correlated positively with the cardiac index (r = 0.42; p = 0.002) and 6MWD (r = 0.38; p = 0.001) and negatively with pulmonary vascular resistance (r = −0.25; p = 0.04; Figure 2 ). Although the serum HDL cholesterol levels did not correlate significantly with mean pulmonary arterial pressure or mean pulmonary capillary wedge pressure, they correlated positively with mixed venous oxygen saturation (r = 0.39; p = 0.01) and arterial carbon dioxide pressure (r = 0.43; p <0.001).

On univariate Cox proportional hazards analysis, WHO functional class, 6MWD, serum uric acid levels, and serum HDL cholesterol levels were related to event-free survival in patients with IPAH. However, age, gender, body mass index, and hemodynamic variables were not predictors of event-free survival.
On multivariate forward stepwise Cox proportional hazards analysis of gender, age, WHO functional class, 6MWD, serum uric acid levels, serum HDL cholesterol levels, and mean right atrial pressure, only the HDL cholesterol level was an independent predictor of event-free survival ( Table 3 ).
| Variable | Univariate Analysis | Multivariate Analysis | ||
|---|---|---|---|---|
| HR (95% CI) | p Value | HR (95% CI) | p Value | |
| Age | 0.995 (0.964–1.026) | 0.737 | — | — |
| Gender | 0.869 (0.407–1.857) | 0.717 | — | — |
| Body mass index | 0.991 (0.895–1.097) | 0.862 | — | — |
| World Health Organization functional class | 1.949 (1.238–3.068) | 0.004 | ||
| Six-minute walking distance | 0.997 (0.994–1.000) | 0.030 | ||
| Heart rate | 1.015 (0.991–1.041) | 0.224 | — | — |
| Mean right atrial pressure | 1.043 (0.984–1.105) | 0.156 | — | — |
| Mean pulmonary arterial pressure | 0.995 (0.976–1.015) | 0.627 | — | — |
| Cardiac index | 0.962 (0.535–1.733) | 0.898 | — | — |
| Pulmonary vascular resistance | 1.020 (0.970–1.072) | 0.439 | — | — |
| Serum uric acid | 1.003 (1.000–1.006) | 0.049 | ||
| Serum high-density lipoprotein cholesterol | 0.148 (0.037–0.591) | 0.007 | 0.172 (0.040–0.735) | 0.018 |
| Partial pressure of carbon dioxide | 0.959 (0.893–1.029) | 0.247 | ||
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


