We describe a 47-year-old man who underwent heart transplantation (HT) for severe right-sided heart failure and periodic episodes of ventricular tachycardia (VT) 43 years after operative repair of tetralogy of Fallot (T of F). The right-ventricular outflow tract, the site where a patch had been placed 4 decades earlier, was aneurysmal. Such development decades after operative repair of T of F of both aneurysm and episodes of VT is probably more common than previously realized.
In July 2011 we reported a 41-year-old man who underwent heart transplantation (HT) because of severe right-sided heart failure and periodic ventricular tachycardia (VT) after operative repair of tetralogy of Fallot (T of F) at age 6. The present report was prompted by studying a similar patient, aged 47, who underwent HT also because of severe right-sided heart failure associated with periodic episodes of VT after operative repair of T of F at age 4. Both patients developed huge right ventricular outflow aneurysms.
Case Description
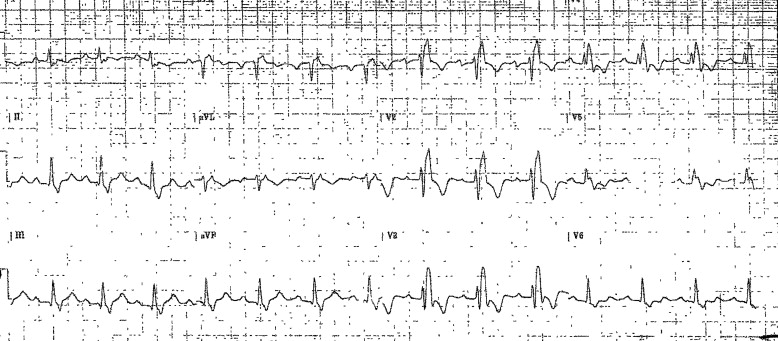
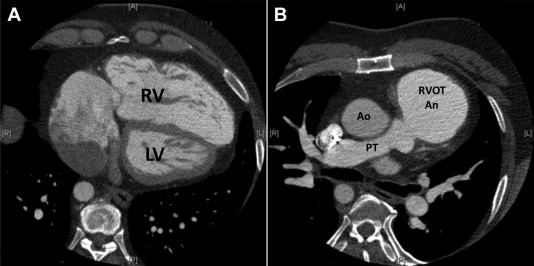
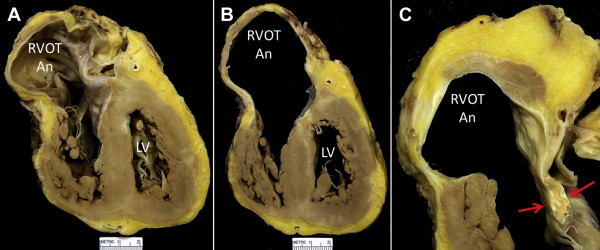
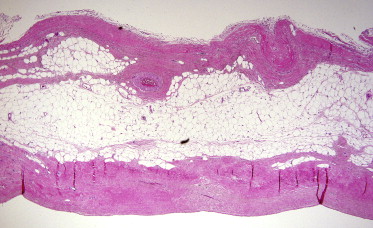
A 47-year-old male manual laborer had repair of T of F at 4 years of age. Thereafter, he was asymptomatic until age 33 years, when he had his first symptomatic episode of VT and an intracardiac defibrillator was inserted. Evidence of right-sided failure appeared about the same time and it gradually progressed thereafter. An electrocardiogram before an intracardiac defibrillator was inserted is shown in Figure 1 . A computed tomographic image of the heart just before HT is shown in Figure 2 . Three months after HT (January 2014) the patient was asymptomatic. Photographs of the explanted heart are shown in Figures 3 and 4 .
Discussion
Described herein is a patient who had HT at age 47 for severe right-sided heart failure and episodic VT occurring several decades after repair of T of F at age 4. The patient described is virtually identical to a patient reported 2 years earlier with a similar scenario ( Table 1 ). The earlier report also described a huge right ventricular outflow tract aneurysm involving the widening patch utilized when eliminating the subvalvular right ventricular outflow tract obstruction. To study 2 similar patients in a 2-year period suggests that aneurysmal formation in the right ventricular outflow tract several decades after repair of T of F may not be an uncommon occurrence but indeed potentially a common late occurrence. The development of episodes of VT with development of the right ventricular outflow aneurysm of course might be described as secondary or acquired arrhythmogenic right ventricular cardiomyopathy/dysplasia.
| Variable | Case 1 ∗ | Case 2 |
|---|---|---|
| Age (years) | ||
| At heart transplantation | 41 (November 2010) | 47 (January 2014) |
| At repair of tetralogy of Fallot | 6 | 4 |
| When RV outflow tract aneurysm first noted | 26 | 33 |
| At onset of heart failure | 26 | 33 |
| At onset of ventricular tachycardia | 26 | 33 |
| Right-sided aortic arch | 0 | + |
| Body mass index (kg/m 2 ) | 25 | 32 |
| Heart weight (g) | 653 | 505 |
| Calcium in RV outflow tract aneurysm | + | 0 |
| RV outflow patch | + (calcified) | + |
| Electrophysiology | ||
| Bundle branch block | Left | Right |
| Intracardiac defibrillator | + (age 36) | + (age 33) |
| Radiofrequency ablation | + | 0 |
| Hemodynamics (mm Hg) | ||
| Left ventricle (s/d) | 96/31 | 113/69 (indirect) |
| Pulmonary artery (s/d) | 33/13 | 44/21 |
| Right ventricle (s/d) | 45/19 | 45/8 |
| Lowest LV ejection fraction (%) | 10 | 50 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


