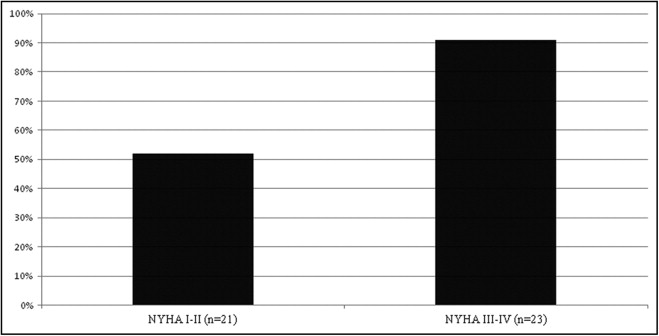
There is strong evidence to suggest that heart failure (HF) is an independent risk factor for cognitive impairment (CI). The combination of CI and HF is associated with increased mortality, repeat hospitalization, and poor quality of life. The purpose of this pilot study was to determine the presence of CI in older patients with HF using the Montreal Cognitive Assessment (MoCA), a brief screening instrument for CI. We conducted a cross-sectional descriptive study using the MoCA in outpatients with HF who were ≥65 years of age. Forty-four patients (mean ± SD 76 ± 6.6 years of age) completed the MoCA. More than 70% of patients scored below the MoCA cutoff score of 26, suggesting the presence of CI. However, 91% of patients with New York Heart Association classes III to IV versus 52% of patients with classes I to II had a MoCA score <26 (p = 0.004). Patients with a recent hospital admission were more likely to have a MoCA score <26 versus patients without a recent hospital admission (89% vs 62%, respectively, p <0.045). Cognitive domain subscores showing significant differences (p <0.01) were short-term memory, visuospatial function, executive function, and language. In conclusion, this study sample represented a group of older patients with HF and no suspected or documented CI, but screening with the MoCA detected CI in >70% of the sample. The presence of CI was significantly more common in patients with advanced HF symptoms or a recent hospitalization. Future studies need to determine if the MoCA can identify the presence of CI that is predictive of adverse clinical outcomes in the HF population.
To date the most widely used instrument to assess cognitive status in the heart failure (HF) population is the Mini Mental State Examination. The Mini Mental State Examination is adequate for detecting moderate to severe cognitive impairment (CI) associated with dementia but is less sensitive in detecting mild CI (MCI). The Montreal Cognitive Assessment (MoCA) was designed as a rapid screening instrument specifically to identify patients with MCI and recommended as the cognitive screening tool of choice for cardiovascular patients. The MoCA assesses 8 different cognitive domains and takes <10 minutes to administer, making it an ideal screening instrument for MCI in a busy clinical setting and minimizing respondent burden. Despite these valuable attributes, the MoCA is not often administered to outpatients with HF. The purpose of this study was to determine the presence of cognitive deficits associated with MCI using the MoCA in older patients with HF without clinically obvious or documented CI while attending a tertiary care outpatient HF clinic.
Methods
Using a cross-sectional descriptive design, consecutive patients with HF who were ≥65 years of age attending the outpatient heart function clinic at the Hamilton Health Sciences, Ontario were screened for inclusion. Patients with documented CI, residing in a long-term care facility, unable to communicate in English, receiving active treatment for major depression, or failing the visual or Whisper tests before MoCA administration were excluded. Written informed consent was obtained from all patients. The study protocol was approved by the research ethics board at Hamilton Health Sciences and McMaster University and conformed to the Declaration of Helsinki.
The MoCA was administered in a standardized format by a trained occupational therapist. Testing lasted approximately 10 minutes per patient. Information on patient demographics, left ventricular ejection fraction, estimated glomerular filtration rate calculated with the Cockcroft-Gault formula, current New York Heart Association (NYHA) class, blood pressure, cardiac medications, and medication administration (own, caregiver assistance, pharmacy dosette) were collected from the patient’s health record.
The MoCA is a screening instrument and assesses 8 different cognitive domains that include attention and concentration, executive function, memory, language, visual/constructional skills, conceptual thinking, calculations, and orientation. Although all sections are brief, each contains items selected from longer psychometric instruments. The maximum possible score is 30 points. An extra point is added to the total score for patients with grade <12 education. In the initial MoCA validation study by Nasreddine et al, scores from patients with MCI were 19.0 to 25.2. Scores <19 are associated with dementia. Using a cut-off score of 26 of 30, the MoCA had a sensitivity of 90% and a specificity of 78% for MCI.
Descriptive statistics for patient demographic data, medical history, medications, and blood pressure were determined using mean ± SD for continuous variables and frequency for categorical variables. Comparisons between patients with normal versus abnormal MoCA scores were conducted using Student’s t test for continuous variables and chi-square test for categorical variables. For exploratory purposes, post hoc comparisons for various cognitive domain subscores between patients with normal and abnormal total MoCA scores were conducted using Student’s t test (normal distribution) or Mann–Whitney nonparametric test (skewed distribution). Statistical tests were 2-sided and a p value ≤0.05 was considered statistically significant. Results are presented as mean ± SD and results for the MoCA were presented as median and interquartile ranges because these were not normally distributed. Data were analyzed using the SPSS 16.0 (SPSS, Inc., Chicago, Illinois).
Results
From January 2008 through April 2008, 99 consecutive patients were screened and 57 patients met eligibility criteria. Reasons for exclusion were language barrier (n = 18), documented CI (n = 13), long-term care residence (n = 4), active treatment for major depression (n = 2), missed opportunity (n = 4), and failed Whisper test (n = 1). Thirteen patients declined, resulting in a final study sample of 44 patients. There were no statistical differences for age, gender, NYHA class, or left ventricular ejection fraction between patients who enrolled versus declined. Baseline characteristics of the 44 patients enrolled are presented in Table 1 .
| Variable | |
|---|---|
| Age (years) | 76 ± 6.4 |
| Men | 24 (55%) |
| Education grade ≥12 | 30 (68%) |
| Living arrangement | |
| With family/caregiver | 30 (68%) |
| Alone | 14 (32%) |
| Medication organization | |
| Organize own | 30 (68%) |
| Caregiver responsible | 5 (11%) |
| Pharmacy dosette | 9 (20%) |
| History of hypertension | 26 (59%) |
| History of hyperlipidemia | 29 (66%) |
| Diabetes mellitus | 25 (34%) |
| History of smoking | 21 (48%) |
| Atrial fibrillation (current) | 15 (34%) |
| Left ventricular ejection fraction (%) | 37 ± 16 |
| Ischemic cardiomyopathy | 25 (57%) |
| New York Heart Association classes | |
| I–II | 21 (48%) |
| III–IV | 23 (52%) |
| Duration of heart failure (years), median (interquartile range) | 2.8 (5.3) |
| Hospitalization in previous 6 months | 18 (41%) |
| Angiotensin-converting enzyme inhibitor or angiotensin receptor blocker | 40 (91%) |
| β Blocker | 35 (80%) |
| Systolic blood pressure (mm Hg) | 122 ± 18 |
| Diastolic blood pressure (mm Hg) | 68 ± 11 |
| Estimated glomerular filtration rate (ml/min/1.73 m 2 ) | 51.0 ± 21.6 |
More than 70% of patients scored below the MoCA cut-off score of 26, suggesting the presence of MCI in most of these patients. Within this cohort 2 patients (4%) scored <19 on the MoCA. There was no difference between patients with normal versus abnormal MoCA scores with respect to age, gender, left ventricular ejection fraction, estimated glomerular filtration rate, cardiovascular risk factors, blood pressure, or cardiac medications.
In the cohort with normal MoCA scores, only 17% of patients (2 of 12) were hospitalized in the previous 6 months, whereas in the cohort with abnormal MoCA scores, 50% (16 of 32) were hospitalized in the previous 6 months, and this difference between groups was statistically significant (p = 0.05). Most patients (10 of 12, 83%) with normal MoCA scores had NYHA class I to II symptoms, whereas most patients (21 of 32, 66%) with abnormal MoCA scores had NYHA class III to IV symptoms. This difference between groups was statistically significant (p = 0.004; Figure 1 ). In other words, 91% of patients (2 of 23) with NYHA class III to IV symptoms had abnormal MoCA scores versus 52% of patients (11 of 21) with NYHA class I to II symptoms.
Comparisons in subscores for various cognitive domains between patients with normal and abnormal total MoCA scores are presented in Table 2 . These data are reported as median scores with interquartile ranges. Cognitive domains showing significant differences in subscores are short-term memory, visuospatial ability, executive function, and language.
| Cognitive Domain | MoCA Items | Total Possible Score | MoCA | MoCA ≥26 | MoCA <26 | p Value |
|---|---|---|---|---|---|---|
| (n = 44) | (n = 12) | (n = 32) | ||||
| Short-term memory | delayed recall | 5 | 3.0 (3) | 4.0 (2) | 2.0 (3) | <0.0001 |
| Visuospatial function | clock, cube | 4 | 3.0 (1) | 4.0 (0) | 3.0 (1) | <0.0001 |
| Executive function | trails, fluency, abstraction | 4 | 2.0 (2) | 4.0 (1) | 2.0 (1) | <0.0001 |
| Attention, concentration, working memory | digit, serial 7, letter | 6 | 6.0 (1) | 6.0 (0) | 6.0 (1) | 0.06 |
| Language | naming, sentence repetition, fluency | 6 | 5.0 (1) | 6.0 (1) | 4.0 (2) | <0.001 |
| Orientation | orientation | 6 | 6.0 (0) | 6.0 (0) | 6.0 (0) | 0.77 |
Results
From January 2008 through April 2008, 99 consecutive patients were screened and 57 patients met eligibility criteria. Reasons for exclusion were language barrier (n = 18), documented CI (n = 13), long-term care residence (n = 4), active treatment for major depression (n = 2), missed opportunity (n = 4), and failed Whisper test (n = 1). Thirteen patients declined, resulting in a final study sample of 44 patients. There were no statistical differences for age, gender, NYHA class, or left ventricular ejection fraction between patients who enrolled versus declined. Baseline characteristics of the 44 patients enrolled are presented in Table 1 .
| Variable | |
|---|---|
| Age (years) | 76 ± 6.4 |
| Men | 24 (55%) |
| Education grade ≥12 | 30 (68%) |
| Living arrangement | |
| With family/caregiver | 30 (68%) |
| Alone | 14 (32%) |
| Medication organization | |
| Organize own | 30 (68%) |
| Caregiver responsible | 5 (11%) |
| Pharmacy dosette | 9 (20%) |
| History of hypertension | 26 (59%) |
| History of hyperlipidemia | 29 (66%) |
| Diabetes mellitus | 25 (34%) |
| History of smoking | 21 (48%) |
| Atrial fibrillation (current) | 15 (34%) |
| Left ventricular ejection fraction (%) | 37 ± 16 |
| Ischemic cardiomyopathy | 25 (57%) |
| New York Heart Association classes | |
| I–II | 21 (48%) |
| III–IV | 23 (52%) |
| Duration of heart failure (years), median (interquartile range) | 2.8 (5.3) |
| Hospitalization in previous 6 months | 18 (41%) |
| Angiotensin-converting enzyme inhibitor or angiotensin receptor blocker | 40 (91%) |
| β Blocker | 35 (80%) |
| Systolic blood pressure (mm Hg) | 122 ± 18 |
| Diastolic blood pressure (mm Hg) | 68 ± 11 |
| Estimated glomerular filtration rate (ml/min/1.73 m 2 ) | 51.0 ± 21.6 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


