Salivary Gland-Type Tumors of the Lung
Marie-Christine Aubry, M.D.
Allen P. Burke, M.D.
General
Salivary gland-type tumors of the lung are rare tumors with a reported frequency of 0.1% to 0.2% of all primary lung tumors. They are thought to arise from the submucosal glands of the bronchi and are morphologically identical to their salivary gland counterparts. Mucoepidermoid carcinoma (MEC) and adenoid cystic carcinoma (ACC) are the most common type of salivary gland-type tumors of the lung,1,2,3 followed by epithelial-myoepithelial carcinoma (EMC).1,4,5,6 Pleomorphic adenoma, carcinoma ex pleomorphic adenoma, and acinic cell carcinoma have also rarely been described.7,8
Salivary gland-type tumors usually occur in adults, in their fourth to sixth decade, but they are also reported in children, particularly MEC.1,4,9,10 There is no gender predilection.1,4,9,10 Causal relationship with cigarette smoking is controversial, but in one series, nearly half of patients with MEC and 70% of patients with ACC were former or current smokers.1 Because of their location, patients often present with symptoms of airway involvement and obstruction such as cough, hemoptysis, wheezing, and obstructive pneumonia.1,3,9,10,11
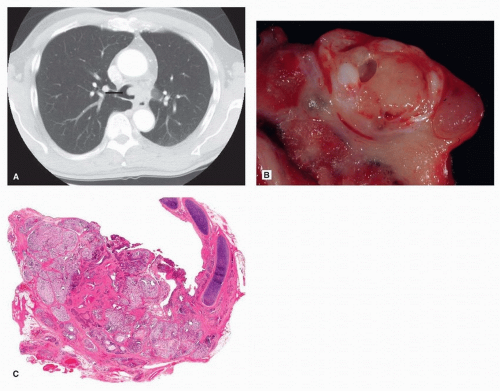
These tumors typically arise in the tracheobronchial tree, forming central endobronchial polypoid tumors1,12 (Fig. 84.1). Size is variable, ranging between 0.5 and 6.0 cm. These tumors are usually well circumscribed with smooth contours. On cut section, the tumors are gray-white, tan, and variably solid-cystic. MEC and pleomorphic adenoma often appear mucoid. These tumors are readily identified on CT scan as endobronchial masses but can also manifest as circumferential thickening of the airway or thick-walled cyst13 (Fig. 84.1). Obstructive pneumonia or atelectasis is a common finding, seen in up to 50% of patients.13,14 Punctate calcifications and secondary localized bronchiectasis are additional findings.13,14 These tumors are usually PET avid, and thus, PET/CT is useful for detection of metastasis.13,15,16
Distinguishing primary salivary gland-type tumors of the lung from primary salivary gland metastasis is important as lung is a favored site of metastasis for these tumors and can occur many years after the initial diagnosis. The presence of peripheral or multiple nodules should lead to a thorough search for a primary salivary gland tumor.
Surgery is the treatment of choice, usually lobectomy, followed by tracheal or sleeve resection based on the airway involved.1,3,4,10 Lymph node sampling is recommended for high-grade MEC and ACC. As in the salivary glands, ACC often tracks along nerve bundles, and resection margins are not uncommonly positive.1,3,4 Adjuvant chemotherapy or radiation may be offered for incompletely resected or advancedstage disease.4,9,17 There are rare case reports of EGFR TKI response in MEC.18,19 KIT kinase inhibitor, imatinib, has been used in the treatment of ACC with rare reports of moderate sustained response.20
Mucoepidermoid Carcinoma
Clinical
MEC tends to occur at a younger age compared to other salivary gland-type tumors and low-grade MEC occurring in younger patients compared to high-grade MEC.4,9,10 MEC rarely presents with locoregional lymph node involvement or distant metastasis, usually seen in high-grade tumors (2% to 15%).1,3,4 Long-term survival for MEC is good, with reported 3-year survival of 94% and 5 and 10 years of 87%, although reported survival for high-grade MEC, more advanced stage, or incompletely resected is lower (66% at 4 years).1,9,10
Pathologic Findings
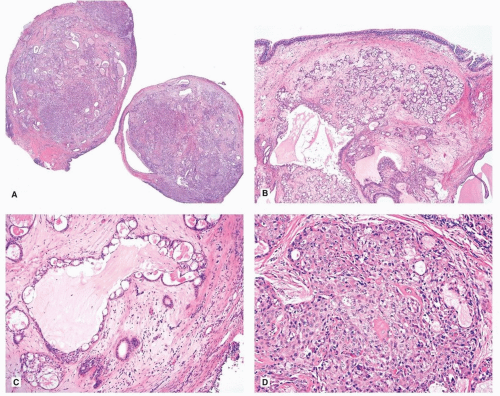
Histologically, MEC is defined by the presence of mucous cells admixed with squamous-, clear-, and intermediate-type cells in various proportions9,12 (Fig. 84.2). The intermediate cells are often predominant and range in size from small basaloid in appearance to larger polygonal cells with more abundant eosinophilic cytoplasm. The mucous cells by definition contain intracytoplasmic mucin, which may occasionally be only appreciated with a mucin stain and may line cystic glands. The squamous cells can be single or form small nests, and typically nonkeratinizing. In some cases, oncocytic cells may predominate.9 Occasionally, the stroma may be dense, hyalinized, and amyloid like with calcifications.9,12
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree