We aimed to evaluate the feasibility and safety of performing percutaneous carotid stent implantation with a newly designed double-layer stent using transradial slender 5Fr techniques. We recruited 10 consecutive patients who underwent percutaneous carotid stenting using nitinol double-layer micromesh (Roadsaver) stents. Mean age of patients was 66 years. Seven patients had ≥2 high-risk criteria according to SAPPHIRE classification. Indication was neurologic symptoms in 7 and severe lesion without symptoms in 3 cases. Type 2 aortic arch was present in 8 patients and type 1 in 2 patients. Access was right radial artery in 9 cases and right ulnar artery in 1 case. Right carotid artery was stented in 4 cases and left carotid artery in 6 cases. Embolic protection device (EPD) was used in 6 cases. Nine stents were successfully delivered using 5Fr destination sheath (n = 7) or shuttle sheath (n = 2), and 1 was implanted using Mo-Ma 8Fr proximal EPD. Procedural success was obtained in all cases with only 1 case of temporary vasospasm due to distal EPD. Total procedural time was 21 minutes (13 to 30 minutes) with filter time of 5 ± 1 minutes. Fluoroscopy time was 8 minutes (5 to 12 minutes) and contrast volume was 150 ml (100 to 200 ml). Hospital stay was 1 ± 1 day with 4 patients discharged on the same day of the procedure. Using right transradial approach and slender 5Fr techniques, this new double-layer micromesh stent can be implanted in left and right carotid arteries with promising results.
In this preliminary report, we aimed to evaluate the feasibility and safety of using slender 5Fr techniques by radial or ulnar approach to deploy new nitinol double-layer micromesh stents in carotid arteries.
Methods
Patients scheduled for carotid stenting regardless to indication were eligible to be included in this observational study. The study was conducted in accordance with our local internal review board regulations, and a written informed consent was obtained from all patients. With the patient’s wrist slightly hyperextended on a dedicated arm board, the right radial or ulnar artery was cannulated, and 11-cm 5Fr sheaths (Terumo Medical, Leuven, Belgium) were initially inserted. After sheath insertion, distal forearm angiography was performed to assess radial and ulnar arteries anatomies and sizes, and 5-mg verapamil was routinely administered through the sheath as spasmolytic agent.
A 260-cm-long 0.035″ J-tipped guidewire was then inserted into the descending aorta, and diagnostic carotid angiography was performed using 5Fr 100-cm Simmons-2 catheters (Merit Medical, Maastricht, The Netherlands) or right Judkins-4 in 1 case as previously described. As per our routine, all patients were preloaded with dual-antiplatelet therapy (aspirin and 300–mg clopidogrel) before the procedure. After successful vascular access, a bolus of 5,000 IU of unfractionated heparin was administered intravenously. At the end of the procedure, all catheters were removed over the 260-cm 0.035″ J-wire and hemostasis obtained by application of TR-band (Terumo Medical, Leuven, Belgium) with minimal pressure to ensure hemostasis while limiting the risk of radial or ulnar artery occlusion.
For this series of carotid interventions, we used slender techniques with 5Fr sheaths in all but 1 case. After completion of diagnostic angiography and review of aortic arch and angulation between common carotid arteries and aortic arch, we selected 2 main strategies. As previously reported, for simple anatomies we used either the anchoring technique and for more complex anatomic situations, we used the telescopic technique.
For the anchoring technique, the initial diagnostic catheter was positioned into the external carotid artery over a 0.035″ wire 260-cm length (Advantage; Terumo Medical, Leuven, Belgium). Then, 5Fr diagnostic and short sheaths were removed and a 90-cm 5Fr Destination sheath (Terumo Medical, Leuven, Belgium) was advanced over the 0.035″ wire just distal to carotid arteries bifurcation. At that time, the lesion in internal carotid artery was crossed with extra-support 0.014-in coronary wire (IronMan; Abbott Vascular, Santa Clara, California). If embolic protection was deemed required, a distal embolic protection device (EPD; Emboshield NAV 6; Abbott Vascular, Santa Clara, California) was positioned 3 to 4 cm distally to main internal carotid lesion. To limit embolic distal inflation time, the Roadsaver (Terumo Medical, Leuven, Belgium) stents were flushed and prepared immediately before EPD deployment. Then, carotid stent was deployed over the 0.014-in wire with mild angiographic injections as required. After stent deployment, postdilation was eventually performed to optimize angiographic results. After final angiographic control, the whole system was removed. Patients were discharged with aspirin (100 mg/day) indefinitely and clopidogrel (75 mg/day) for 1 month.
For the telescoping technique, wiring the carotid external artery is basically the same. However, to gain more support, a long 125 cm braided Simmons-2 (Cook Medical, Limerick, Ireland) was used with shuttle sheath as mother-in-child technique. This technique is particularly helpful with extreme angle anatomies such as nonbovine left carotid or sharp take-off right carotid artery.
Depending on the anatomies between the common carotid artery and aortic arch, we used different strategies to optimally position the sheath. For simple anatomies, sheaths were either positioned using a direct approach or simple loop technique. As last resort, we used deep-loop technique where the wire and sheath looped on the aortic cusps. With this technique, a telescopic approach was used to ensure optimal support.
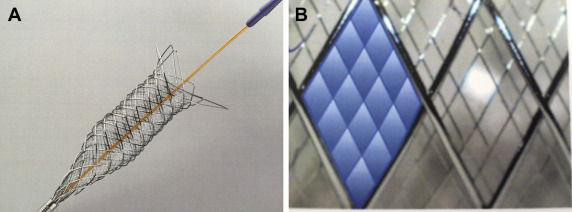
Patients were discharged the same day of the procedure or the next day. Clinical visit was scheduled at 30 days with complete neurologic examination. Roadsaver stents (Terumo Medical, Leuven, Belgium) are newly designed nickel–titanium (nitinol) stents with a double-layer micromesh architecture ( Figure 1 ). These self-expandable stents are mounted on low-profile 5Fr rapid exchange system. One macromesh cell contains 16 micromesh cells (375 to 500 μm), which offer optimized protection against tissue protrusion and embolization. Stents are available from 5- to 10-mm diameter and 25- to 43-mm length and can accommodate vessels 1 or 2 mm smaller in diameter than unconstrained conditions (maximal length 60 mm; Figure 1 ).
Categorical variables are expressed as numbers and percentages and continuous variables as the mean ± standard deviation or median (interquartile range). All calculations and statistical analysis were performed using JMP 10.0 software (SAS Institute, Cary, North Carolina).
Results
From February 19 to February 23, 2015 (3 working days), we recruited 10 consecutive patients. Eight patients were men, and most had several high-risk criteria for surgical endarterectomy according to SAPPHIRE criteria ( Table 1 ). Regarding cardiovascular risk factors, 9 patients were treated for hypertension, 4 had diabetes, 3 had hyperlipidemia, and 2 were still active smokers. Four patients had had previous myocardial infarction and 3 had multivessel coronary artery disease. Four patients had undergone previous carotid artery stenting, 2 previous percutaneous coronary intervention (PCI), and 7 patients were symptomatic before the index procedure. Type 2 aortic arch was present in 8 patients and type 1 in 2 cases. All procedures were successfully completed from the right wrist, right radial access in 9 cases and ulnar artery with previous radial artery occlusion in 1 case. In 4 cases, the right carotid was the target artery, and in 6 cases, the left internal carotid artery. In 5 cases, we used distal EPD and in 1 case, we used Mo-Ma 8Fr proximal embolic protection ( Figures 2 and 3 ). In 6 cases, we used Destination 5Fr 90-cm sheath; in 3 cases, 5Fr 90-cm Shuttle sheath for telescopic strategies; and in 1 case, we had to use a short 8Fr sheath in a right radial to allow the use of the Mo-Ma EPD. In 2 cases, we cannulated the carotid using a simple loop approach; in 2 cases, a direct common carotid cannulation; and in 1 case, we had to use a deep loop approach with telescopic strategy to secure enough support. Overall, anchoring technique was used in 7 cases and telescopic technique in 3 cases.
| Pt | Years | Man/ Woman | ∗ Sapphire criteria | Bilateral carotid disease | RICA/ LICA | Aortic arch type | Catheter size | Cannulation technique | Protection device |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 56 | Woman | 5 | YES | LICA | Type 2 | 5Fr | Anchoring | – |
| 2 | 59 | Man | 4,5 | NO | LICA | Type 2 | 5Fr | Telescopic | – |
| 3 | 60 | Woman | 4,5 | NO | LICA | Type 2 | 5Fr | Anchoring | DPD |
| 4 | 63 | Man | 2,3,4 | NO | LICA | Type 2 | 5Fr | Telescopic | DPD |
| 5 | 64 | Man | 5 | YES | RICA | Type 1 | 8Fr MO-MA | Anchoring | PPD |
| 6 | 64 | Man | 2,4,5 | NO | RICA | Type 2 | 5Fr | Anchoring | – |
| 7 | 67 | Man | 2,4 | YES | RICA | Type 2 | 5Fr | Anchoring | DPD |
| 8 | 76 | Man | 5 | NO | RICA | Type 2 | 5Fr | Anchoring | DPD |
| 9 | 82 | Man | 1,4 | NO | LICA | Type 1 | 5Fr | Anchoring | DPD |
| 10 | 82 | Man | 1,2,4 | YES | LICA | Type 2 | 5Fr | Telescopic | – |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


