The optimal management strategy for patients with ST-elevation myocardial infarction (STEMI) and multivessel disease has not been well established. In the present cohort study, we sought to examine the safety and efficacy of inhospital staged PCI for patients with STEMI and multivessel disease. We identified all patients with STEMI referred for primary PCI who were found to have multivessel disease (stenosis ≥50% in nonculprit vessel) and compared clinical outcomes in relation to the management strategy, staged versus culprit-only PCI, for nonculprit vessel disease. The primary outcome was mortality at 180 days, and secondary outcomes included mortality during the index hospitalization and at 30 days, myocardial infarction, stent thrombosis, stroke, and bleeding. Of the 1,038 patients with STEMI meeting inclusion criteria, 259 (25%) underwent staged PCI and 779 (75%) culprit-only PCI during the index admission. Mortality at 180 days was 0.8% in patients with staged PCI and 5.0% in patients with culprit-only PCI (p = 0.003). The association between staged PCI and reduced mortality persisted after adjusting for baseline differences in patient characteristics and angiographic variables between the 2 cohorts (odds ratio 0.2, 95% confidence interval 0.04 to 0.77, p = 0.02). The rates of inhospital reinfarction in the staged and culprit-only PCI cohorts were 0.8% versus 1.3% (p = 0.50), respectively, stent thrombosis 0.8% versus 1.3% (p = 0.50), and stroke 0.4% versus 1.3% (p = 0.31). There were no inhospital adverse events related to acute occlusion of a nonculprit vessel in either cohort. Staged PCI during index admission is a safe and effective revascularization strategy for patients with STEMI and multivessel disease.
Primary percutaneous coronary intervention (PCI) is currently the standard revascularization strategy for the infarct-related artery in ST-elevation myocardial infarction (STEMI). A substantial number of patients with STEMI are also found to have significant stenosis in nonculprit vessels during primary PCI. The optimal strategy for the management of these lesions has not been well established. Two recent randomized controlled trials have demonstrated improved outcomes with multivessel revascularization in patients with STEMI and multivessel disease. However, the optimal timing of multivessel revascularization after STEMI was not directly addressed in these trials and, thus, remains an area of active research and debate. In the most recent STEMI guidelines, multivessel revascularization during primary PCI for the management of STEMI with multivessel disease ranges from a class III to IIb indication. In the present study, we sought to examine clinical outcomes in patients with STEMI and multivessel disease in relation to the management strategy, staged inhospital versus culprit-only PCI, for nonculprit vessel disease. We also assessed the safety and efficacy of revascularizing patients with STEMI and multivessel disease at a time other than the index primary PCI (i.e., staged PCI) by examining the incidence, timing, and nature of inhospital adverse events and their association with nonculprit arteries.
Methods
The University of Ottawa Heart Institute (UOHI) STEMI program serves a catchment area of >1.3 million patients in eastern Ontario and provides treatment for >500 patients with STEMI annually. The UOHI STEMI registry is a prospective database of patients managed through different STEMI pathways and contains demographic, therapeutic, and outcome data for all patients cared for at the UOHI from July 2004 to June 2011. During this time interval, the standard of care was to intervene only on the infarct-related artery during primary PCI for STEMI as per the American College of Cardiology/American Heart Association (ACC/AHA) guidelines.
In the present study, we examined baseline characteristics, management, and outcomes of patients with STEMI who underwent primary PCI and were found to have multivessel coronary disease on their index coronary angiogram. Specifically, we examined outcomes in relation to the revascularization strategy for nonculprit lesions, culprit-only versus staged PCI, during the index admission. To address survival bias when assessing inhospital mortality, patient charts were reviewed to determine the intended revascularization strategy for nonculprit disease after primary PCI. We defined STEMI as the presence of ST elevation ≥1 mm in 2 contiguous leads on a 12-lead electrocardiogram and multivessel disease as angiographic evidence of stenosis of ≥50% in a nonculprit vessel. We excluded patients treated with fibrinolysis or balloon angioplasty only, previous coronary artery bypass grafting, mechanical complications of myocardial infarction, cardiogenic shock on admission, out-of-hospital cardiac arrest meeting criteria for therapeutic hypothermia, left main disease (stenosis of ≥50%), and those referred for coronary artery bypass grafting during the index admission. All patients were treated with aspirin 160 mg, clopidogrel 600 mg, and unfractionated heparin 60 U/kg (maximum 4,000 U) intravenously before PCI.
The primary outcome of our analysis was mortality at 180 days. Secondary outcomes included mortality during index hospitalization, after discharge, and at 30 days and the incidence of reinfarction, stent thrombosis, stroke, and cardiogenic shock. Reinfarction was defined as recurrent chest pain with new ST-segment changes, associated increase in cardiac biomarkers, or angiographic documentation of new thrombus involving either the infarct-related artery or a nonculprit artery. Stroke was defined as a new neurologic deficit of ≥24 hours in duration confirmed as ischemic or hemorrhagic stroke by the treating neurologist. Safety outcomes included peak creatinine, and minor and major bleeding as defined by the Thrombolysis In Myocardial Infarction classification.
We present categorical variables using percentages or frequencies, and continuous variables using means (±SD) or medians (interquartile range), when appropriate. We compared categorical variables using the chi-square test (or Fisher’s exact test when appropriate), and continuous variables using the student’s t test and Mann-Whitney U test for normally and non-normally distributed variables, respectively. We provided odds ratios and 95% confidence intervals for all outcomes examined. Because of the nonrandomized nature of this analysis, we performed a multivariable logistic regression analysis to adjust for baseline differences in key patient and angiographic variables. The dependent variable in our model was mortality at 180 days, controlled for differences in baseline variables with p <0.10 by univariable analysis. We then performed a conditional logistic regression analysis comparing the incidence of the primary outcome in the 259 patients who underwent staged PCI to a 1-to-1 propensity score–matched sample from the culprit-only PCI cohort. Variables used to generate the propensity score were those potentially associated with the decision to pursue staged PCI. Statistical analyses were conducted using SAS, version 9.13 (SAS Institute, Cary, North Carolina). Two-sided p values <0.05 were considered statistically significant.
Results
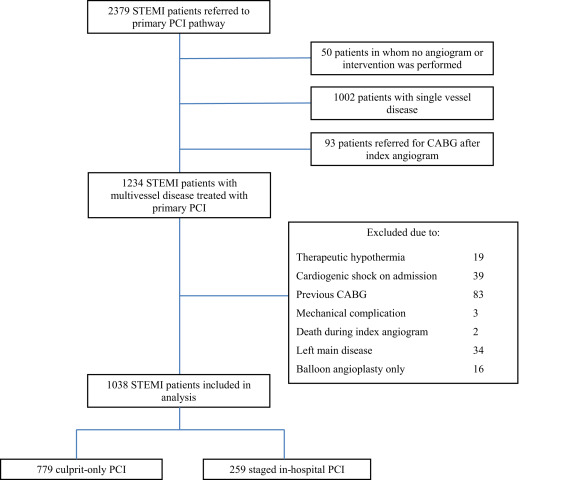
Of 2,379 consecutive patients with STEMI referred to the UOHI primary PCI pathway during the registry interval, 1,038 patients with multivessel disease were eligible for the current analysis. Of these patients, 259 (25%) received staged PCI during the index admission and 779 (75%) had culprit-only PCI ( Figure 1 ). There were no instances of multivessel revascularization during the index primary PCI among eligible patients in our database. Baseline patient and angiographic characteristics are summarized in Tables 1 and 2 , respectively. Compared with patients who received culprit-only PCI, patients who underwent staged PCI during the index admission were younger and more likely to be men. All other baseline patient characteristics were similar between the 2 cohorts. With regard to angiographic and procedural variables, patients with staged PCI had a greater prevalence of triple-vessel disease compared with those who underwent culprit-only PCI and were more likely to have received glycoprotein IIb/IIIa inhibitors during primary PCI. At discharge, aspirin was prescribed for 98.8% of patients in the staged PCI cohort and 98.4% of patients in the culprit-only PCI cohort (p = 0.77); clopidogrel for 100% versus 99.2% (p = 0.35); β blockers for 98.2% versus 94.0% (p = 0.01); angiotensin-converting enzyme inhibitors for 88.8% versus 83.4% (p = 0.04); angiotensin receptor blockers for 3.9% versus 5.7% (p = 0.26); and statins for 96.5% versus 98.3% (p = 0.09), respectively.
| Characteristic | Staged PCI (n=259) | Culprit-only PCI (n=779) | p value |
|---|---|---|---|
| Age (years) | 60.9 ±12 | 64.6 ±13 | 0.01 |
| Women | 47 (18.2%) | 217 (27.9%) | 0.002 |
| Hypertension | 124 (48.3%) | 406 (52.4%) | 0.25 |
| Diabetes mellitus | 54 (20.9%) | 151 (19.4%) | 0.61 |
| Current smoker | 103 (39.9%) | 295 (38.1%) | 0.60 |
| Hyperlipidemia | 108 (43.2%) | 327 (42.9%) | 0.94 |
| Atrial fibrillation | 7 (2.7%) | 28 (3.6%) | 0.49 |
| Previous myocardial infarction | 24 (9.3%) | 93 (12.0%) | 0.23 |
| Previous stroke or transient ischemia attack | 12 (4.7%) | 59 (7.6%) | 0.10 |
| Previous percutaneous coronary intervention | 21 (8.2%) | 72 (9.3%) | 0.59 |
| Body mass index (kg/m 2 ) | 27.9 ± 5 | 27.6 ± 5 | 0.97 |
| Heart rate (beats/min) | 77 ± 18 | 76 ± 19 | 0.72 |
| Systolic blood pressure (mmHg) | 139 ± 27 | 139 ± 29 | 0.27 |
| Anterior ST-elevation | 79 (30.5%) | 273 (35.1%) | 0.17 |
| Killip class | 0.23 | ||
| I | 235 (90.7%) | 711 (91.4%) | |
| II | 23 (8.9%) | 55 (7.1%) | |
| III | 1 (0.4%) | 12 (1.5%) | |
| Creatinine clearance (ml/min) | 75.3 ± 22 | 70.9 ± 23 | 0.32 |
| Peak creatine kinase (units/L) | 1844 ± 1435 | 1621 ± 1516 | 0.30 |
| Variable | Staged PCI (n=259) | Culprit-only PCI (n=779) | p value |
|---|---|---|---|
| Symptom onset-to-balloon time (minutes) † | 219 (150, 358) | 222 (152, 351) | 0.97 |
| Door-to-balloon time (minutes) † | 96 (71, 133) | 97 (69, 130) | 0.80 |
| Infarct related coronary artery | 0.31 | ||
| Left anterior descending | 82 (31.7%) | 282 (36.2%) | |
| Left circumflex | 46 (17.8%) | 109 (14.0%) | |
| Right | 131 (50.6%) | 386 (49.6%) | |
| Unknown | 0 (0%) | 2 (0.3%) | |
| Triple-vessel coronary disease | 134 (51.7%) | 286 (36.7%) | <0.001 |
| Baseline infarct-related artery TIMI flow | 0.53 | ||
| 0 | 144 (55.6%) | 414 (53.2%) | |
| 1 | 21 (8.1%) | 70 (9.0%) | |
| 2 | 33 (12.7%) | 126 (16.2%) | |
| 3 | 61 (23.6%) | 169 (21.7%) | |
| Final infarct-related artery TIMI flow | 0.64 | ||
| 0 | 0 (0%) | 4 (0.5%) | |
| 1 | 0 (0%) | 3 (0.4%) | |
| 2 | 10 (3.9%) | 24 (3.1%) | |
| 3 | 247 (96.1%) | 740 (96.0%) | |
| Glycoprotein IIb/IIIa inhibitor use | 96 (37.1%) | 230 (29.5%) | 0.02 |
| Contrast dye volume (ml) | 233 ± 68 | 239 ± 78 | 0.01 |
∗ Plus–minus values are means ± standard deviation.
Table 3 illustrates clinical outcomes among the 2 treatment cohorts. Follow-up was available for 1,019 patients (98%) at 180 days. The incidence of the primary outcome, all-cause mortality at 180 days, was 0.8% in the staged PCI group and 5.0% in the culprit-only PCI group (p = 0.003). Compared with patients treated with culprit-only PCI, patients who underwent staged PCI also had lower mortality rates during their index admission and at 30 days. The incidence of stent thrombosis, reinfarction, stroke, and bleeding events was similar between the 2 cohorts. In the culprit-only PCI cohort, 11 patients (1.4%) had reinfarctions during the index hospitalization, with 100% of cases being secondary to stent thrombosis in the infarct-related artery. In the staged PCI cohort, 2 patients (0.4%) experienced reinfarction during the index hospitalization, with both cases resulting from stent thrombosis in the infarct-related artery. Reinfarction was associated with a 15% risk of inhospital mortality. There were no documented cases of reinfarction, cardiogenic shock, or death presumed to be related to a nonculprit artery.
| Variable | Staged PCI (n=259) | Culprit-only PCI (n=779) | p value |
|---|---|---|---|
| In-hospital events | |||
| Mortality | 1 (0.4%) | 20 (2.6%) | 0.03 |
| Reinfarction | 2 (0.8%) | 10 (1.3%) | 0.50 |
| Stent thrombosis | 2 (0.8%) | 10 (1.3%) | 0.74 |
| Congestive heart failure | 24 (9.7%) | 69 (9.3%) | 0.85 |
| Cardiogenic shock | 1 (0.4%) | 20 (2.6%) | 0.03 |
| Stroke | 1 (0.4%) | 10 (1.3%) | 0.31 |
| TIMI major bleeding | 7 (2.7%) | 24 (3.1%) | 0.76 |
| TIMI minor bleeding | 32 (12.4%) | 72 (9.2%) | 0.15 |
| Length of stay (days) ∗ | 6 (4,7) | 4 (3,6) | <0.001 |
| Readmission with PCI | 2 (1.7%) | 27 (9.3%) | 0.006 |
| Mortality at 30 days | 1 (0.4%) | 22 (2.9%) | 0.02 |
| Mortality after discharge | 1 (0.4%) | 18 (2.4%) | 0.06 |
| Mortality at 180 days | 2 (0.8%) | 38 (5.0%) | 0.003 |
After adjustment for baseline differences in patient and angiographic variables, inhospital staged PCI remained associated with improved survival at 180 days compared with a culprit-only strategy ( Figure 2 ). Explanatory variables in our regression model consisted of treatment assignment (staged vs culprit-only PCI), age, gender, glycoprotein IIb/IIIa inhibitor use, triple-vessel disease, and right coronary artery involvement. The c-statistic was 0.78. Among explanatory variables, only treatment assignment and age were independently associated with mortality at 180 days. In our propensity score–matched analysis, inhospital staged PCI remained associated with lower odds of mortality at 180 days compared with the propensity score–matched culprit-only PCI cohort (odds ratio 0.2, 95% confidence interval 0.04 to 0.91, p = 0.04). Variables used to generate the propensity score are listed in Table 4 .




