Rupture after EVAR from Endoleak
DANIEL FREMED and PETER L. FARIES
Based on chapter in previous edition by Peter L. Faries, Rajeev Dayal, Scott Hollenbeck, Albeir Mousa, and K. Craig Kent
Presentation
The patient is a 72-year-old man who complains of increasing left-sided abdominal pain of 48 hours’ duration. He had undergone elective endovascular aneurysm repair (EVAR) 2 years prior but has since been lost to follow-up. On physical examination, the patient is in visible discomfort. His blood pressure is 115/35 mm Hg with a heart rate of 110 beats per minute. His abdomen is distended with a palpable, tender, left-sided pulsatile mass. There is no flank ecchymosis. There are well-healed transverse groin incisions bilaterally. Peripheral pulses are palpable. The patient denies chest pain, shortness of breath, or syncopal episodes.
Differential Diagnosis
The patient presents with tachycardia, acute abdominal findings, and a pulsatile mass; however, he reports having undergone prior endovascular abdominal aortic aneurysm (AAA) repair. The differential should therefore include ruptured abdominal aortic aneurysm but should also include diverticulitis, renal lithiasis, intestinal perforation, pancreatitis, and spontaneous retroperitoneal hematoma. The differential diagnosis may also include rare aneurysms, including splenic and other visceral artery aneurysms, as well as para-anastomotic aneurysms with or without infection. In this instance, physical examination is consistent with a ruptured AAA despite prior EVAR.
Workup
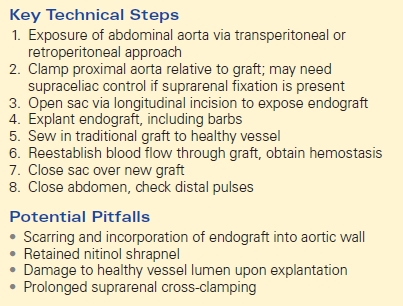
The most accurate method of diagnosing ruptured AAA is computerized tomography (CT) with intravenous contrast. CT findings consistent with rupture include extravasation of contrast outside of the aorta, retroperitoneal hematoma, and retroperitoneal stranding. In patients with a history of EVAR, CT may provide the etiology of likely endoleak. Imaging may reveal endograft position in relation to native aorta, presence of significant lumbar arteries or patent inferior mesenteric artery (IMA), and degree of component overlap in multibody devices. In addition to making the diagnosis of rupture, CT scan can be used to evaluate multiple organ systems to exclude other diagnoses in the differential (Fig. 1).
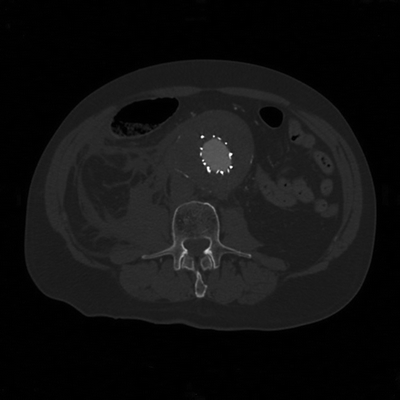
FIGURE 1 CT image of infrarenal aortic endograft with evidence of rupture.
Diagnosis and Treatment
Based on history, physical exam, and CT findings of retroperitoneal bleeding in the setting of aortic disruption, the most likely diagnosis is ruptured AAA despite prior EVAR.
The goal of treatment is identification and exclusion of the source of rupture. Continued arterial perfusion of the aneurysm sac after endovascular repair has been termed an endoleak. Endoleaks result in continued pressurization of the aneurysm sac. The significance of the continued perfusion is determined by the source of the endoleak. Endoleaks that result in direct arterial flow into the aneurysm sac cause systemic pressurization of the aneurysm. These leaks may occur at the sites of attachment of the stent graft to the native arterial wall, the seal, or implantation zones (type I endoleak). Direct antegrade endoleaks may also occur at junction sites between different endovascular stent graft components (type III endoleak). Types I and III endoleaks are the most common causes of rupture after EVAR (Fig. 2).
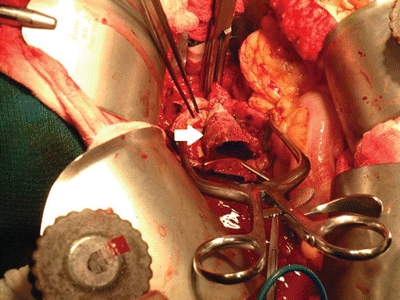
FIGURE 2 Exposure of aneurysm sac revealing embedded endovascular stent graft (arrow).
Surgical Approach
When an untreated or unrecognized endoleak results in aneurysm rupture, immediate surgical intervention is necessary to prevent exsanguination and death. Several approaches may be used, including placement of an occlusion balloon in the aorta proximal to the aneurysm, immediate standard surgical repair, and endovascular aneurysm repair. The choice is based on anatomic suitability of the aorta on CTA, as well as surgeon comfort with each type of intervention.
Open Approach
Patients presenting with rupture are taken to the operating room emergently. The patient is prepped and draped in the supine position prior to induction general anesthesia. The aorta is exposed via a traditional transperitoneal or retroperitoneal approach.
The site of proximal cross-clamping is dependent on the type of previously placed endograft. Infrarenal clamping of the aorta is preferred in endografts without suprarenal fixation. The aorta may be clamped above the renal arteries in the presence of suprarenal endograft fixation. Distal control is obtained bilaterally by cross-clamping the iliac arteries.
Once systemic anticoagulation is achieved, proximal and distal control is obtained. The sac is opened via a longitudinal incision exposing the endograft. The endograft is then carefully removed. If the barbs of the device are well incorporated in the aortic wall, the lateral wall can be longitudinally incised with or without endarterectomy. Once the graft is explanted, a traditional unibody or bifurcated graft is sewn into nondiseased portions of proximal and distal vessel. In cases where complete graft removal is not feasible, the standard graft may be sewn to residual well-incorporated endograft. To do so, the stent graft may be divided sharply and the suprarenal component incorporated with the proximal suture line. Similarly, the distal iliac limbs may not be readily amenable to removal without causing injury to the iliac arteries. In such instances, the bifurcated aortic graft may be sewn to the iliac limbs of the stent graft.
Proximal and distal clamps are removed, and suture lines are inspected for hemostasis. The fascial layers of the abdomen are closed in usual fashion provided there is little tension. The abdomen may be left open if closure proves difficult or results in abdominal compartment syndrome (Table 1).
TABLE 1. Rupture after EVAR from Endoleak