20 Role of Transesophageal Echocardiography in Mitral Valve Repair
Mitral Valve Diagrams
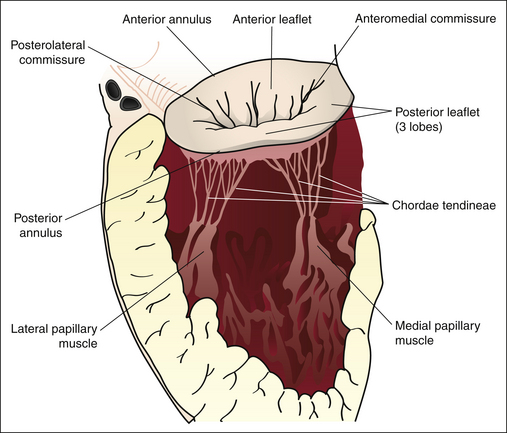
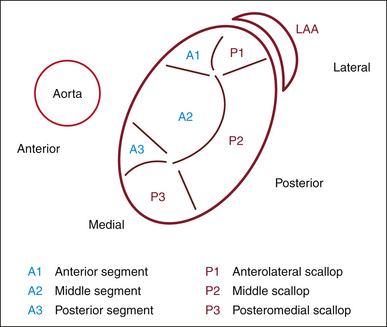
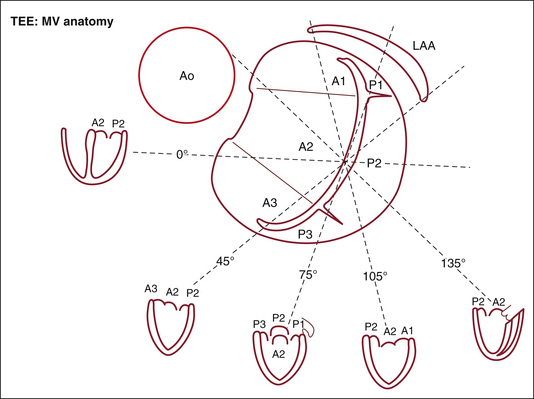
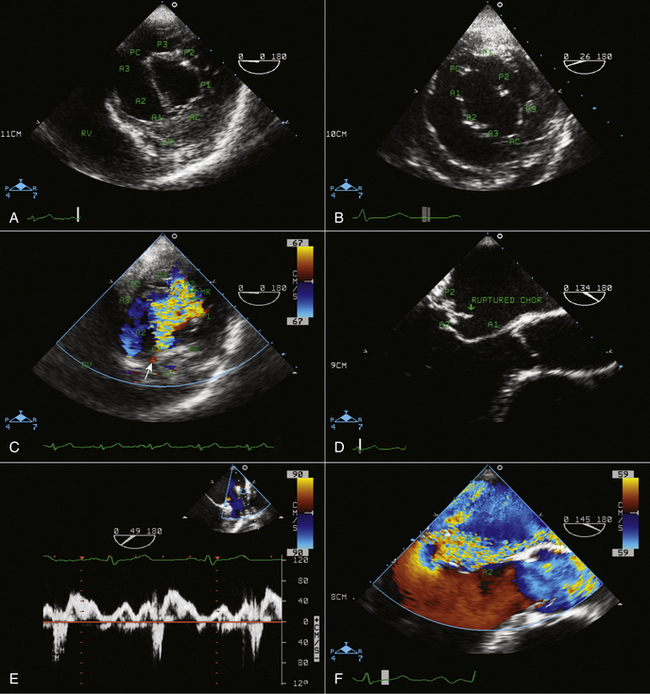
Figures 20-1 through 20-5 present the anatomy of the mitral valve.
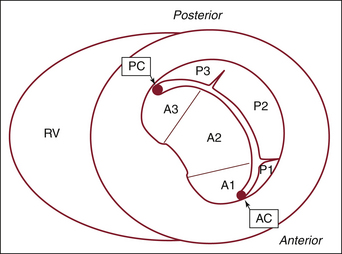
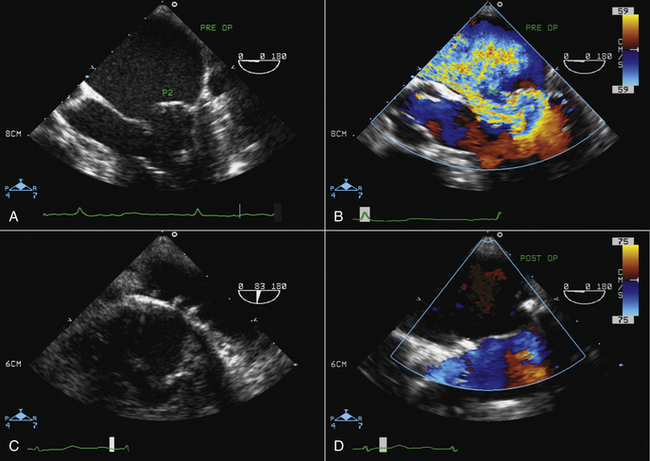
Figure 20-4 Transgastric short-axis view of the mitral valve at the level of the base of the left ventricle. This diagram was designed in the Toronto General Hospital Echocardiography Laboratory using the same classification as the illustration in Figure 20-3. Note the anterior (anterolateral) commissure (AC) at the bottom of the illustration and the posterior (posteromedial) commissure (PC) at the top. On this view, the site of origin of the mitral regurgitation can be defined by color Doppler flow mapping. A1, anterior segment; A2, middle segment; A3, posterior segment; P1, anterolateral scallop; P2, middle scallop; P3, posteromedial scallop; RV, right ventricle.
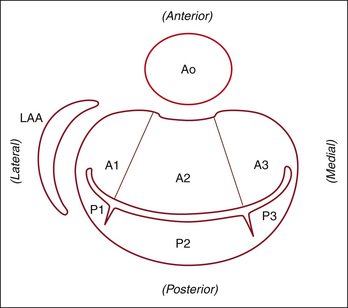
Figure 20-5 The same view as Figure 20-4, rotated 90 degrees to mimic the surgical view of the mitral valve looking from the left atrium toward the left ventricle. A1, anterior segment; A2, middle segment; A3, posterior segment; Ao, aorta; LAA, left atrial appendage; P1, anterolateral scallop; P2, middle scallop; P3, posteromedial scallop.