To investigate the role of hydration to prevent contrast-induced nephropathy (CIN) in patients with ST-segment elevation myocardial infarction (STEMI) who underwent primary percutaneous coronary intervention (PPCI), we prospectively included 408 consecutive patients who were randomly assigned to receive either hydration with isotonic saline (1 ml/kg/h since the beginning of the procedure and for 24 hours after it: NS+ group) or not (NS− group). All patients received an iso-osmolar nonionic contrast medium. The primary end point was the development of CIN: ≥25% or ≥0.5 mg/dl increase in serum creatinine within 3 days after the procedure. CIN was observed in 14% of patients: 21% in the NS− group and 11% in the NS+ group (p = 0.016). CIN was significantly associated with death (15.2% vs 2.8%; p <0.0001) and need for dialysis (13.4% vs 0%; p <0.0001). In multivariate analysis, the only predictors of CIN were hydration (OR = 0.29 [0.14 to 0.66]; p = 0.003) and the hemoglobin before the procedure (OR = 0.69 [0.59 to 0.88]; p <0.0001). In conclusion, intravenous saline hydration during PPCI reduced the risk of CIN to 48%. Patients with CIN had increased mortality and need for dialysis. Given the higher incidence of CIN in emergent procedures, and its morbidity and mortality, preventive hydration should be mandatory in them unless contraindicated.
The incidence of contrast-induced nephropathy (CIN) in patients who underwent primary percutaneous coronary intervention (PPCI) for ST-segment elevation myocardial infarction (STEMI) is higher than in elective procedures. Paradoxically, in PPCI, CIN prevention measures are less applied than in elective PCI. At present, no preventive strategy has been recommended by current guidelines in patients with STEMI who undergo PPCI. The aim of this study was to evaluate the possible beneficial role of periprocedural intravenous volume expansion with isotonic saline in patients with STEMI who undergo PPCI.
Methods
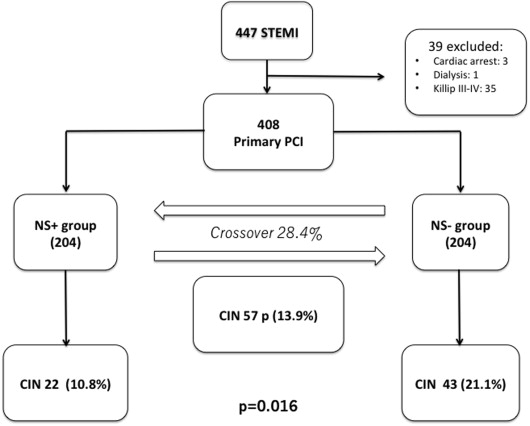
We included all consecutive patients who were admitted for STEMI and underwent a PPCI from July 2012 to November 2013 at our institution. Initial exclusion criteria were end-stage renal failure requiring dialysis, cardiac arrest, and severe heart failure (Killip III to IV) before starting PPCI. Eligible patients were randomly assigned in a 1:1 ratio to receive hydration (NS+ group) or not (NS− group).
Patients assigned to hydration received isotonic saline at an infusion rate of 1 ml/kg/h since the beginning of the procedure and during the following 24 hours.
Echocardiographic evaluation of left ventricular function was performed in all patients after PPCI. Hydration rate was reduced to 0.5 ml/kg/h in patients with left ventricular ejection fraction <40% or in those who became Killip class III to IV during or after PPCI. In addition, patients included in any group could also be changed to the other after randomization regarding clinical or hemodynamic condition (i.e., right ventricle myocardial infarction, pulmonary congestion, systemic hypotension).
In all cases, we used iodixanol (Visipaque; GE Healthcare Ltd, Amersham, United Kingdom), a nonionic, dimeric iso-osmolar contrast medium. Serum creatinine concentration was assessed at the time of hospital admission and on days 1, 2, 3, and the day of discharge. All tests were performed in the hospital laboratory with consistent methodology. All patients provided written informed consent before PPCI, and data were recorded in a dedicated database.
PPCI was performed by a 24-hour, on-call interventional team, according to standard clinical practice. All patients received a bolus of 300 mg aspirin and a loading dose of a P2Y12 inhibitor (clopidogrel 600 mg, prasugrel 60 mg, or ticagrelor 180 mg). Unfractionated heparin (70 to 100 U/kg body weight) or Bivalirudin (intravenous bolus of 0.75 mg/kg followed by an infusion of 1.75 mg/kg/h during the procedure and for 4 hours later) were used as anticoagulant agents. The use of the IIb/IIIa glycoprotein inhibitor abciximab was left to the operator’s decision. If it was administered, an intracoronary bolus of 20 mg was used, and the heparin dose was reduced (50 to 70 U/kg body weight).
The primary end point was the development of CIN, defined as a ≥25% or ≥0.5 mg/dl increase in serum creatinine within 3 days after administration of the contrast medium. Glomerular filtration rate (GFR) was estimated by applying the level-modified Modification of Diet in Renal Disease formula. Renal function was categorized according to the stages set by the National Kidney Foundation (United States), with GFR ≥90 ml/min considered normal, 60 to 89 ml/min mildly impaired, 30 to 59 ml/min moderately impaired, and ≤30 ml/min severely impaired. The nephropathy risk score was calculated as specified by Mehran et al. The administered contrast volume-to-GFR ratio was calculated using the method by Laskey et al. As secondary end points, we evaluated the association of CIN with all-cause mortality, need for dialysis, and duration of hospital stay.
The number of patients included in the study was based on previous trials of hydration in patients who underwent STEMI and on the results of a previous registry performed by our group in which the prevalence of CIN in patients who underwent STEMI treated with PPCI was 15%. To test our hypothesis with a power of 80%, and with a projected reduction of CIN of 30%, we planned to include a minimum of 150 patients in each group. Categorical variables were reported as absolute values and percentages and were analyzed by the chi-square analysis or Fisher’s exact test. Normal distributions of continuous data were tested using a Kolmogorov-Smirnov test, and variables are represented as mean ± SD or as medians (interquartile range). Independent t test and Wilcoxon tests were used to determine differences between normal and non-normally distributed quantitative variables, respectively. Multivariate logistic regression analysis was also performed, using all potentially relevant variables to identify independent predictors of CIN. As a significant crossover rate was expected because patients could be changed to the other group after randomization regarding their hemodynamic condition, exploratory analysis and an intention-to-treat analysis were performed. In addition, as it was difficult to mask patients or providers with regard to treatment assignments, during the outcomes analysis, the data analysts were blinded regarding treatment assignments. All analyses were performed with SPSS statistical software, version 20.0 (SPSS Inc, Chicago, Illinois). All probability values are 2 tailed, and statistical significance was defined as p ≤0.05.
Results
Of the 447 consecutive patients with STEMI who were considered eligible for the present study, 39 were excluded (1 because of end-stage renal failure requiring dialysis, 3 because they presented a cardiac arrest and need for cardiopulmonary resuscitation maneuvers, and 35 because of severe heart failure before starting PPCI). Thus, a total of 408 patients were randomly assigned (204 per group); 116 patients were changed after randomization (crossover rate of 28.4%): 74 patients initially included in NS− group were changed to the NS+ group because of severe hypotension and need of volume infusion, the majority of them in the context of right ventricle infarction; 42 patients were changed from NS+ to NS− group because they developed significant heart failure despite reducing the rhythm of the infusion.
Clinical and demographic characteristics are listed in Table 1 . Mean age was 63.1 ± 13.6 years, and 73.4% of the patients were men. Mean creatinine clearance was 88.8 ± 38.5 ml/min. All patients received iodixanol (mean volume 174 ± 72 ml). The administered contrast volume-to-GFR ratio was 1.97 ± 38.4. Mean isotonic saline volume administered to patients in NS+ group was 1720 ± 234 ml. There were no other significant differences between the 2 groups regarding baseline features ( Table 1 ) nor in the procedural characteristics ( Table 2 ).
| Variable | Overall (n=408) | Hydration | P value | |
|---|---|---|---|---|
| Yes (n=204) | No (n=204) | |||
| Male | 299 (73.4%) | 147 (72.1%) | 152 (74.5%) | 0.68 |
| Age (years) | 63.1 ± 13.6 | 61.7 ± 14 | 63.9 ± 12 | 0.25 |
| Body mass index (kg/m 2 ) | 27.8 ± 3.7 | 27.6 ± 4.1 | 27.9 ± 4.5 | 0.6 |
| Diabetes mellitus | 92 (22.5%) | 48 (23.5%) | 44 (21.6%) | 0.61 |
| Hypertension | 193 (47.3%) | 94 (46.1%) | 99 (48.5%) | 0.38 |
| GFR (ml/min/1.73m 2 ) | 89 ± 39 | 90 ± 21 | 88 ± 54 | 0.45 |
| GFR≤60 (ml/min/1.73m 2 ) | 51 (12.5%) | 26 (12.7%) | 25 (12.2%) | 0.98 |
| Anemia | 51 (12.5%) | 28 (13.7%) | 23 (11.8%) | 0.87 |
| Ejection Fraction | 49% ± 8% | 48% ± 6% | 51% ± 9% | 0.85 |
| Killip class >1 before PPCI | 60 (14.7%) | 27 (13.2) | 33 (16.1) | 0.65 |
| Right Ventricle infarction | 127 (31.1%) | 65 (31.9%) | 62 (30.4%) | 0.23 |
| Mehran risk score | 4.9 ± 1.7 | 5.1 ± 0.8 | 4.8 ± 1.3 | 0.42 |
| Variable | Overall (n=408) | Hydration | P value | |
|---|---|---|---|---|
| Yes (n=204) | No (n=204) | |||
| Contrast Volume (ml) | 174 ± 72 | 180 | 173 | 0.23 |
| Contrast volumen/ GFR | 1.9 ± 38.4 | 2.1 ± 0.3 | 1.9 ± 0.4 | 0.56 |
| Number of narrowed coronary arteries | 1.5 ± 0.9 | 1.5 ± 0.8 | 1.5 ± 0.7 | 0.56 |
| Radial approach | 92.1% | 93.6% | 91.2% | 0.83 |
| Abciximab | 246 (60.3%) | 125 (61.3%) | 121 (59.3%) | 0.25 |
| Intraaortic balloon pump | 9 (2.2%) | 4 (2%) | 5(2.4%) | 0.73 |
| Maximum Creatine-kinase | 2067 ± 687 | 1877 ± 187 | 1908 ± 230 | 0.93 |
The overall incidence of CIN was 14% (57 of 408): 21.1% (43 of 204) in the NS− group and 10.8% (22 of 204) in the NS+ group (p = 0.016; Figure 1 ). Intravenous hydration achieved a relative reduction of risk of CIN of 48.8%. Other predictors of CIN in the univariate analysis were female gender (p = 0.005), hypertension (p = 0.001), anemia (p = 0.028), older age (68.5 vs 62.7 years; p = 0.009), and a lower hemoglobin level before the procedure (13.1 vs 14.2 g/dl; p <0.0001; Table 3 ). In the multivariate analysis, we included the variables with significant association with CIN presentation in the univariate analysis and all potentially relevant variables that have been previously shown to increase the risk of CIN including diabetes, Killip class, contrast volume, and previous renal dysfunction. The only independent variables associated with CIN were hydration (OR = 0.29 [0.14 to 0.66]; p = 0.003) and a higher hemoglobin before the procedure (OR = 0.69 [0.59 to 0.88]; p <0.0001) ( Table 3 ). We also performed an exploratory analysis categorizing all patients into their received treatment group to compare it with the programmed intention-to-treat analysis and to appreciate the impact of crossover rate on primary outcome. In this exploratory analysis, the incidence of CIN was 21% in NS− group and 6.6% in NS+ group. The incidence of CIN was reduced 68%. In the multivariate analysis performed in these groups, the independent variables associated with CIN were the same than in the intention-to-treat analysis: hydration (OR = 0.3 [0.17 to 0.7]; p = 0.002) and the hemoglobin before the procedure (OR = 0.7 [0.6 to 0.9]; p <0.0001). The overall in-hospital mortality rate was 4.9% (20 patients), and as expected, the rate was higher in patients who developed CIN (15.2% vs 2.8%; p <0.0001). CIN was also associated with an increased need for dialysis (13.4% vs 0%; p <0.0001). CIN was not associated with a longer hospital stay (no CIN: 8.6 ± 3.7 days vs CIN: 11.6 ± 4.4 days; p = 0.18; Figure 2 ). There were no significant differences between both treatment groups regarding secondary end points: death (NS− 8 of 159 vs NS+ 7 of 153; p = 1), dialysis (NS− 2 of 153 vs NS+ 1 of 150; p = 1), and length of hospital stay (NS− 6 vs NS+ 8.2 days; p = 0.7).