Lack of health insurance is associated with interfacility transfer from emergency departments for several nonemergent conditions, but its association with transfers for ST-elevation myocardial infarction (STEMI), which requires timely definitive care for optimal outcomes, is unknown. Our objective was to determine whether insurance status is a predictor of interfacility transfer for emergency department visits with STEMI. We analyzed data from the 2006 to 2011 Nationwide Emergency Department Sample examining all emergency department visits for patients age 18 years and older with a diagnosis of STEMI and a disposition of interfacility transfer or hospitalization at the same institution. For emergency department visits with STEMI, our multivariate logistic regression model included emergency department disposition status (interfacility transfer vs hospitalization at the same institution) as the primary outcome, and insurance status (none vs any [including Medicare, Medicaid, and private insurance]) as the primary exposure. We found that among 1,377,827 emergency department STEMI visits, including 249,294 (18.1%) transfers, patients without health insurance (adjusted odds ratio 1.6, 95% CI 1.5 to 1.7) were more likely to be transferred than those with insurance. Lack of health insurance status was also an independent risk factor for transfer compared with each subcategory of health insurance, including Medicare, Medicaid, and private insurance. In conclusion, among patients presenting to United States emergency departments with STEMI, lack of insurance was an independent predictor of interfacility transfer. In conclusion, because interfacility transfer is associated with longer delays to definitive STEMI therapy than treatment at the same facility, lack of health insurance may lead to important health disparities among patients with STEMI.
Insurance status itself, particularly lack of insurance, is a risk factor for suboptimal clinical outcomes. For example, patients without insurance had 43% higher odds of ruptured appendicitis and have nearly 30% higher odds of death from intracerebral hemorrhage. As this group is already at risk for poor clinical outcomes due to a lack of health insurance, the introduction of additional delays as a result of interfacility transfer may further jeopardize outcomes for this vulnerable population. Therefore, we sought to evaluate the association between insurance status and interfacility transfer for patients diagnosed with ST-elevation myocardial infarction (STEMI) in United States emergency departments. Our hypothesis was that lack of health insurance was an independent risk factor for increased transfer.
Methods
Our data source was the Nationwide Emergency Department Sample (NEDS), a publicly available administrative database from the Healthcare Cost and Utilization Project and the largest available source of national emergency department data. NEDS was constructed using the Healthcare Cost and Utilization Project State Emergency Department Databases and State Inpatient Databases. It includes a 20% sample of all emergency department visits in the United States and contains weighting variables to calculate national estimates from this sample. Using deidentified data, NEDS tracks geographic, hospital and patient characteristics, including diagnosis codes for each patient visit. NEDS contains between 25 and 30 million unweighted emergency department visits for each year between 2006 and 2011. The Vanderbilt University Institutional Review Board approved this study as nonhuman research with waiver of informed consent.
For the present study, we included adult (patient age ≥18 years) emergency department visits from 2006 to 2011 with an NEDS diagnosis of STEMI ( International Classification of Diseases, Ninth Revision, Clinical Modification codes: 410.01, 410.11, 410.21, 410.31, 410.41, 410.51, 410.61, 410.81, or 410.91).
We constructed a multivariate logistic regression model to evaluate the association between health insurance status and the odds of interfacility transfer for emergency department patients with STEMI. The primary exposure variable was the patient’s health insurance status at the time of the emergency department visit for STEMI. Insurance status was categorized into 4 mutually exclusive groups based on the primary payer for the emergency department visit: no health insurance; Medicare; Medicaid; and private health insurance. Emergency department visits with an unknown insurance status in NEDS were excluded. The primary comparison was between patients with no health insurance and those with any health insurance (Medicare, Medicaid, or private insurance). We also compared patients with no health insurance separately to those with Medicare, Medicaid, and private insurance.
The primary outcome was disposition from the emergency department, categorized as admission at the same facility or transfer to another facility. Emergency department visits with a disposition listed as death in the emergency department were excluded because these patients did not have an opportunity for admission or transfer. We also excluded STEMI emergency department visits with an unknown disposition and those resulting in emergency department discharge. These visits resulting in emergency department discharge were excluded because this represents atypical care of patients with STEMI and likely reflects special patient circumstances (e.g., palliative care wishes or leaving against medical advice).
Several potential confounders were included as covariates, including: patient age, gender, year of presentation (2006 to 2011), United States geographic region (West, Northeast, Midwest, and South), annual emergency department patient volume, household median income in the patient’s home zip code by quartiles, weekend presentation to the emergency department, trauma center designation (nontrauma center vs any trauma center designation), and urban/rural status (urban vs rural). Cubic spline functions were applied to patient age and annual emergency department patient volume ; both of these covariates had knots located at the 10th, 50th, and 90th percentiles. In addition, a fourth knot was placed at 65 years old for patient age because this is the typical age Americans qualify for Medicare services. All statistical analyses were conducted using SAS 9.4.
As some patients who lack insurance may be more or less likely to present to facilities that have primary percutaneous coronary intervention (pPCI) capabilities, we planned to examine whether a facility’s interfacility transfer rate influenced our results. To explore the association between insurance status and transfer specifically in hospitals that transfer some, but not all patients with STEMI, we performed 2 secondary analyses by limiting the study population to hospitals that transfer (1) between 5% and 95% of emergency department STEMI patients and (2) between 10% and 90% of emergency department STEMI patients. The rationale for these secondary analyses was to identify patients who were simultaneously at risk for both admission to the local hospital and interfacility transfer during their emergency department visit.
Results
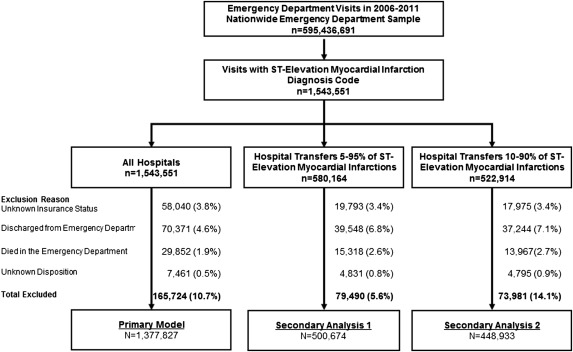
From 2006 to 2011, there were an estimated 595,436,691 total adult emergency department visits in the United States, including 1,543,551 (0.3%) visits for STEMI. Among these 1,543,551 STEMI visits, we excluded 165,724 visits (10.7%) from our analysis, including 58,040 (3.8%) with an unknown insurance status, and 70,371 (4.6%) discharged from the emergency department, 29,852 (1.9%) who died in the emergency department, and 7,461 (0.5%) emergency department visits with an unknown disposition. Secondary analyses included 500,674 and 448,933 emergency department visits at hospitals with interfacility transfer rates between 5% and 95%, and 10% and 90%, respectively. A flow diagram for case selection in the primary model and planned secondary analyses can be seen in Figure 1 .
After these exclusions, 1,377,827 STEMI emergency department visits were included in the multivariate analysis, 110,321 (8.0%) of these visits were for patients without health insurance ( Table 1 and Supplementary Table 1 ). Compared with patients with insurance, those without insurance were younger, more likely to be men, and more likely to live in a zip code where the median household income was in the bottom quartile nationally. Among the 1,267,506 STEMI emergency department visits for patients with insurance, Medicare (n = 747,565 [59.0%]) was the most common insurance type, followed by private insurance (n = 433,542 [34.2%]) and Medicaid (n = 86,399 [6.8%]).
| Variable | Health Insurance | |
|---|---|---|
| No (n =110,321) | Yes (n = 1,267,506) | |
| Age Group, years | ||
| 18-34 | 4,189 (3.8%) | 11,800 (0.9%) |
| 35-44 | 18,167 (16.5%) | 60,144 (4.8%) |
| 45-54 | 42,291 (38.3%) | 188,233 (14.9%) |
| 55-64 | 39,275 (35.6%) | 266,815 (21.1%) |
| 65-74 | 3,853 (3.5%) | 278,454 (22.0%) |
| 75-84 | 1,725 (1.6%) | 269,185 (21.2%) |
| 85+ | 821 (0.7%) | 192,876 (15.2%) |
| Sex | ||
| Male | 83,638 (75.8%) | 768,130 (60.6%) |
| Female | 26,655 (24.2%) | 499,204 (39.4%) |
| Timing of Emergency Department Presentation | ||
| Weekday | 79,030 (71.6%) | 906,940 (71.6%) |
| Weekend | 31,282 (28.4%) | 360,484 (28.4%) |
| Year | ||
| 2006 | 17,999 (16.3%) | 247,676 (19.5%) |
| 2007 | 18,943 (17.2%) | 227,475 (18.0%) |
| 2008 | 18,389 (16.7%) | 217,455 (17.2%) |
| 2009 | 16,939 (15.4%) | 198,953 (15.7%) |
| 2010 | 20,370 (18.5%) | 194,002 (15.3%) |
| 2011 | 17,681 (16.0%) | 181,944 (14.4%) |
| Median Household Income Quartiles | ||
| $1-$40,999 | 37,603 (35.2%) | 335,188 (27.0%) |
| $41,000-$50,999 | 31,973 (29.9%) | 346,310 (27.9%) |
| $51,000-$66,999 | 23,690 (22.2%) | 300,534 (24.2%) |
| $67,000+ | 13,611 (12.7%) | 258,222 (20.8%) |
| U.S. Region of the Hospital | ||
| West | 15,479 (14.0%) | 236,989 (18.7%) |
| Northeast | 13,215 (12.0%) | 208,850 (16.5%) |
| Midwest | 25,589 (23.2%) | 335,304 (26.5%) |
| South | 56,037 (50.8%) | 486,364 (38.4%) |
| Hospital Trauma Center Designation | ||
| Nontrauma center | 82,155 (74.5%) | 940,031 (74.2%) |
| Trauma center | 28,165 (25.5%) | 327,475 (25.8%) |
| Hospital Urban-Rural Location | ||
| Rural | 22,579 (20.5%) | 249,909 (19.7%) |
| Urban | 87,742 (79.5%) | 1,017,597 (80.3%) |
| Annual ED Volume Quartiles | ||
| < 25 percentile | 4,971 (4.5%) | 67,351 (5.3%) |
| [25, 50) percentile | 14,163 (12.8%) | 172,558 (13.6%) |
| [50, 75) percentile | 28,871 (26.2%) | 363,821 (28.7%) |
| >=75 percentile | 62,315 (56.5%) | 663,776 (52.4%) |
| Inter-facility Transfer | 29,522 (26.8%) | 219,772 (17.3%) |
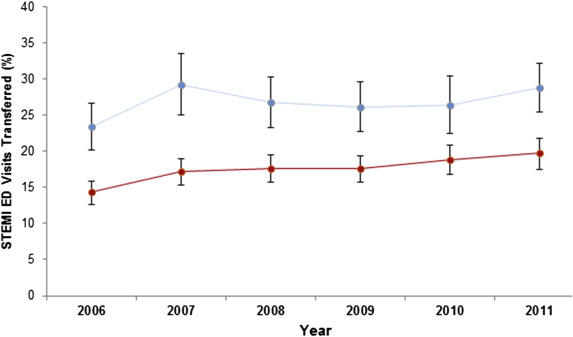
During the 6-year study period, 249,294 (18.1%) of the included emergency department STEMI visits resulted in interfacility transfer. Of the 110,321 STEMI emergency department visits by patients without insurance, 29,522 (26.8%) resulted in transfer, compared with 219,772 (17.3%) transfers among the 1,267,506 STEMI visits by patients with health insurance (p <0.001). Overall, the percentage of STEMI emergency department visits resulting in interfacility transfer increased over the study period, ranging from 14.9% in 2006 to 20.1% in 2011. Transfer was more common for STEMI visits by patients without health insurance than those with insurance during each year of the study ( Figure 2 ).
In the primary multivariate logistic regression model, lack of health insurance was an independent risk factor for interfacility transfer (adjusted odds ratio for no health insurance compared with any health insurance 1.6, 95% CI 1.5 to 1.7; Table 2 ). Having no health insurance was also an independent risk factor of interfacility transfer when separately compared with Medicare, Medicaid, and private health insurance ( Table 2 ).
| Predictor Variable | Adjusted Odds Ratio | 95% Confidence Interval | |
|---|---|---|---|
| Health insurance status | |||
| None vs. Any | 1.6 | 1.5 | 1.7 |
| None vs. Medicare | 1.8 | 1.6 | 2.0 |
| None vs. Medicaid | 1.8 | 1.6 | 2.0 |
| None vs. Private | 1.3 | 1.2 | 1.4 |
| Male (vs female) | 1.2 | 1.2 | 1.2 |
| Presentation on weekend (vs weekday) | 1.1 | 1.0 | 1.1 |
| Study year (continuous variable 2006 – 2011) | 1.1 | 1.1 | 1.2 |
| U.S. geographic region | |||
| West | Referent | ||
| Northeast | 1.8 | 1.3 | 2.5 |
| Midwest | 1.5 | 1.1 | 2.0 |
| South | 1.5 | 1.1 | 2.0 |
| Rural hospital (vs urban hospital) | 2.4 | 2.0 | 3.0 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


