Risk Factors and Risk Modifications
The aging process can bring multiple health problems. Many of these problems are now well-recognized risk factors for atherosclerosis that have important impact on and increase the risk of coronary artery disease as well as peripheral vascular diseases, such as lower-extremity occlusive disease and cerebrovascular disease (Fig. 7.1). Simply put, the older one gets, the higher the risk of atherosclerosis. When these factors are controlled well, the risk of both vascular disease progression and perioperative events are reduced. However, when these risk factors are not controlled they may work in concert in the development of vascular disease and perioperative events. This chapter focuses broadly on some of these cardiovascular risk factors and on counseling patients about how to minimize cardiovascular events around the time of vascular interventions. Specific pathways that can be used to stratify periprocedural risk once a specific vascular intervention is planned are addressed in Chapter 8.
I. Tobacco abuse.
Cigarette smoking has now clearly been identified as an independent predictor of vascular disease and failure of vascular operations or interventions. While smoking has notoriously been associated with coronary artery disease, the cerebrovascular and lower-extremity arteries appear to be more adversely affected by cigarette smoking than the coronary system. Smoking increases the risk of stroke at least twofold and the risk of lower-extremity occlusive disease four- to sixfold (two times that in the coronary arteries). Continued tobacco abuse is responsible for vascular disease progression, while smoking cessation mitigates these effects. Studies have shown that the risk of death, myocardial infarction (MI), amputation, and bypass graft failure are all lower in those who have stopped smoking compared with active smokers. The precise mechanisms of smoking’s harmful effects on the heart and blood vessels are not fully understood, due in part to the fact that the chemical milieu produced by the burning of tobacco produces over 8,000 chemical byproducts. It is generally accepted, however, that nicotine is the stimulant and addictive component of tobacco. Despite this addictive property, nicotine does not appear to participate in the adverse effects of smoking on the vascular system. In contrast, oxidizing agents in tobacco are known to cause vasoconstriction, hypertension, and endothelial dysfunction, which, in addition to inhibition of pros tacyclin, cause a hypercoagulable state. The effect of these oxidizing substances in cigarette smoke lead to augmented lipid deposition, platelet aggregation, and smooth muscle cell dysfunction. Collectively, these harmful effects encourage the formation of new atherosclerotic lesions and cause existing lesions to be less stable and more prone to thrombosis.
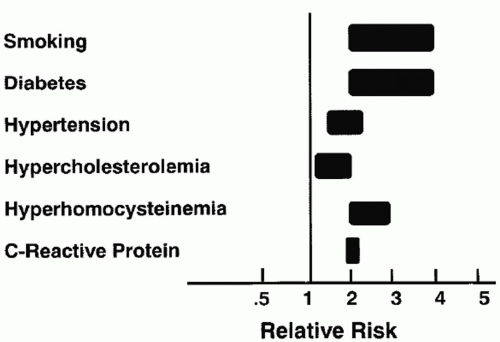 Figure 7.1. Range of independent impact of each atherosclerotic risk factor in the development of lower-extremity vascular disease. Smoking indicates comparison versus former smoking. (From Hirsch AT, Haskal ZJ, Hertzer NR, et al. for the writing committee. ACC/AHA 2005 guidelines for the management of patients with peripheral arterial disease [lower extremity, renal, mesenteric, and abdominal aortic]: A collaborative report from the AAVS/SVS/SCAI/SVMB/SIR and the ACC/AHA task force on practice guidelines. J Am Coll Cardiol. 2005;e1-e192, with permission.) |
It is no wonder that smoking cessation is critical to improving cardiovascular outcomes. Convincing smokers to quit is not easy, as most are affected by chemical addiction. The techniques available to help patients discontinue smoking will not succeed unless the patient really wants to stop. Those who are convinced that smoking is related to their vascular disease and have good motivation generally will stop smoking. Unfortunately, these individuals are in the minority and only 40% of men and 30% of women who quit smoking will remain free of tobacco one year later.
Most studies of smoking cessation pharmacotherapy have focused on nicotine as the addictive element in tobacco. Nicotine replacement therapy comes in several forms, including transdermal patches, gum, nasal spray, inhalers, and sticks meant to simulate cigarettes. A newer nicotinic receptor agonist based on the
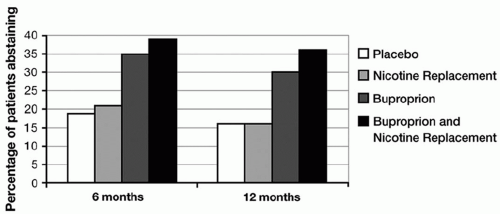
structure of cytosine, called varenicline (Chantix Pfizer, Inc., New York, NY, U.S.A.) has shown particular effectiveness in helping individuals to quit smoking. The antidepressant bupropion (Wellbutrin and Zyban, GlaxoSmithKline, Brentford, Middlesex, U.K.) has also been used with some success to reduce symptoms of withdrawal and achieve smoking cessation. Combination therapy consisting of bupropion and nicotine replacement has been shown in some studies to improve cessation rates compared to either therapy alone (Fig. 7.2). Interestingly, a new nicotine vaccine is being evaluated that in theory turns the body’s immune system against the chemical before it is able to reach the brain and cause its addictive effects. Most studies have found that the effectiveness of any of these medications in assisting with smoking cessation is increased if combined with formal counseling and/or psychotherapy sessions. Regardless of the method used, the best long-term results to date report cessation rates of only 20-25%, although evidence suggests that rates may be higher with the newer nicotine receptor agonists.
structure of cytosine, called varenicline (Chantix Pfizer, Inc., New York, NY, U.S.A.) has shown particular effectiveness in helping individuals to quit smoking. The antidepressant bupropion (Wellbutrin and Zyban, GlaxoSmithKline, Brentford, Middlesex, U.K.) has also been used with some success to reduce symptoms of withdrawal and achieve smoking cessation. Combination therapy consisting of bupropion and nicotine replacement has been shown in some studies to improve cessation rates compared to either therapy alone (Fig. 7.2). Interestingly, a new nicotine vaccine is being evaluated that in theory turns the body’s immune system against the chemical before it is able to reach the brain and cause its addictive effects. Most studies have found that the effectiveness of any of these medications in assisting with smoking cessation is increased if combined with formal counseling and/or psychotherapy sessions. Regardless of the method used, the best long-term results to date report cessation rates of only 20-25%, although evidence suggests that rates may be higher with the newer nicotine receptor agonists.
II. Hypertension.
The management and control of hypertension mitigates the development and progression of peripheral arterial disease and the risk of adverse periprocedural cardiac events defined as stroke, MI, and cardiovascular death. The risk of each of these events is two to four times higher in hypertensive patients compared with patients with normal blood pressure. Traditional guidelines have set a systolic blood pressure of 140 mm Hg or lower and diastolic pressure of 90 mm Hg or lower as “normal” target numbers. More recent information suggests that lower target numbers of 130/80 or lower are beneficial in patients with diabetes, renal insufficiency, and certain forms of heart disease.
Three common categories of antihypertensive medications are beta-receptor blockers, calcium channel blockers, and medications that alter the renin-angiotensin system, either through inhibition of the angiotensin-converting enzyme (ACE inhibitors) or through angiotensin receptor blockade (ARBs). Beta-blockers and ACE inhibitors have both been shown to reduce the incidence of MI and cardiovascular death in those with coronary disease, and ACE inhibitors have been shown to reduce these same adverse outcomes in patients with peripheral arterial disease. The effectiveness of beta-blocker therapy in reducing periprocedural and long-term cardiac events in those undergoing vascular interventions is so well established that it should be part of every patient’s medical management.
In addition to the benefits of reduced blood pressure levels, arterial wall and myocardial cell remodeling are favorably altered by medications that block the renin-angiotensin-aldosterone system. The specifics of these effects remain less well defined and represent an area of active research; however, these medications in particular may modify the cardiovascular system through a mechanism that is independent of their effects on blood pressure levels.
In addition to the categories of antihypertensive medications already mentioned, the central acting medication clonidine and the direct vasodilator hydralazine are useful in treating more significant hypertension in some individuals. Diuretics such as hydrochlorothiazide (often abbreviated HCTZ) and Lasix (furosemide) can be used alone or in combination with other antihypertensive agents to successfully treat high blood pressure. Importantly, improvements in blood pressure control can also be realized by healthy lifestyle modifications, such as an improved diet, weight loss, and initiation of an exercise program. If blood pressure measurements remain elevated and refractory despite months of treatment with multiple agents, renal artery occlusive disease (e.g., renovascular hypertension) should be considered as a possible etiology.
III. Hyperlipidemia.
Control of high serum lipids may slow the progression of atherosclerosis. In particular, statin medications or hydroxymethylglutaryl (HMG) CoA-reductase inhibitors not only control cholesterol but appear to halt atherogenesis and may even lead to plaque regression. They also have helpful effects on the endothelium and vascular smooth muscle and are antithrombotic. Their use has been shown to reduce all types of cardiovascular events. In the Scandinavian Simvastatin Trial, drug therapy for hypercholesterolemia was associated with a 38% reduction in the development or worsening of claudication. The Heart Protection Study has revealed significant reductions in coronary events, strokes, and peripheral intervention requirements in those with and without diagnosed peripheral vascular diseases using simvastatin (Zocor, Merck & Co., Inc., West Point, PA, U.S.A.) (Fig. 7.3




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree