Perioperative Planning and Care of the Vascular Patient
Optimal care of the vascular patient in the operating room or endovascular suite requires a keen understanding and awareness of details related to monitoring, patient preparation and positioning, and anesthesia. The improved awareness of the vascular provider in each of these areas ensures the best chance for a safe, technically successful procedure with the lowest possible risk of morbidity and mortality. Each vascular procedure, whether it is an open aneurysm repair in the operating room or a percutaneous lower-extremity arteriogram and stent in the imaging suite, requires a well thought-out and communicated plan in regard to these topics. Optimal patient preparation and positioning may be accomplished through a “final time out” or operating room or endovascular suite briefing and are imperative to ensure that the correct procedure is performed on the correct patient at the correct surgical sight. The monitoring and anesthesia plans are especially relevant in transition to care of the patient in the post-procedure setting, which can be the recovery room, post-anesthesia care unit (PACU), inpatient ward, or intensive care unit (ICU). This chapter emphasizes the principles of basic cardiac and respiratory monitoring, patient preparation and positioning, and anesthesia. An understanding of these should be of particular value to surgical house staff, nurses, and other vascular providers who are often the first into the operating room or endovascular suite and the first to recognize and treat problems during the postoperative period.
OPERATIVE PLAN AND ANESTHESIA
Improved anesthetic management has been a key factor in the reduction of perioperative morbidity and mortality in vascular and endovascular surgery. The preoperative assessment of the patient and his or her comorbidities form the basis for selecting the most appropriate anesthetic. The anesthesia team must be aware of the planned procedure and the procedural conduct—much more than simply reading the name from the operating room list of the day. The type and depth of anesthetic varies widely among the range of vascular and endovascular procedures to be performed. Therefore, for the smooth conduct of any vascular or endovascular operation, regardless of level of complexity, communication between the vascular and anesthesia providers must begin before the start of the case and continue throughout.
Clinical examples that emphasize the need for communication include the requirement for patients undergoing certain endovascular procedures to remain fully awake and directable during the procedure. In these instances patients may need to remain still, hold their breath, or have neurologic evaluation during the procedure (e.g., during carotid arteriography or stenting). Any conscious sedation at all in such cases may be too
much and result in an overly sedated, noncooperative patient and a suboptimal procedure. The effectiveness of regional anesthesia for certain extremity procedures also needs to be discussed well before the procedure to avoid placement of a peripheral nerve block or regional anesthetic that does not fully anesthetize the planned area of operation (e.g., nerve block that anesthetizes the forearm and hand when the planned operation is the upper arm and axilla). And finally, the anesthesia team must be aware of specific aspects of the procedure, open or endovascular, that are most stressful to cardiac, cerebral, respiratory, and renal function in order to manage the patient effectively. This chapter provides an overview of physiologic monitoring that applies to the operating room or endovascular suite and focuses on perioperative care for carotid, aortic, and lower-extremity procedures.
much and result in an overly sedated, noncooperative patient and a suboptimal procedure. The effectiveness of regional anesthesia for certain extremity procedures also needs to be discussed well before the procedure to avoid placement of a peripheral nerve block or regional anesthetic that does not fully anesthetize the planned area of operation (e.g., nerve block that anesthetizes the forearm and hand when the planned operation is the upper arm and axilla). And finally, the anesthesia team must be aware of specific aspects of the procedure, open or endovascular, that are most stressful to cardiac, cerebral, respiratory, and renal function in order to manage the patient effectively. This chapter provides an overview of physiologic monitoring that applies to the operating room or endovascular suite and focuses on perioperative care for carotid, aortic, and lower-extremity procedures.
I.
Perioperative physiologic monitoring provides clinical data critical to assessment and maintenance of cardiac, respiratory, neurologic, and renal function during and after any open or endovascular procedure. The magnitude of the procedure and the patient’s medical condition determine the extent of monitoring, and it should be recognized that in some instances the information gathered may be misleading or imprecise and may not influence the overall outcome of the patient. It is important to understand the limitations of monitoring and use only techniques and devices that will provide useful or actionable information.
A. Basic intravenous access and monitoring.
All patients should have at least one sizable (14- or 16-gauge) intravenous line and electrocardiographic (ECG), temperature, and blood pressure monitoring. A urinary catheter and collection system to measure urine output is needed for operations that last longer than a few hours or endovascular interventions that may require the patient to remain supine for several hours following the procedure.
B.
Pulse oximeters, which attach to a finger or toe, are used to continuously measure arterial oxygen saturation of hemoglobin. Pulse oximetry functions by positioning a pulsating arterial vascular bed between a two-wavelength light source and a detector. A familiar plethysmograph waveform results. Because the detected pulsatile waveform is produced from arterial blood, the amplitude of each wavelength is related to reduced versus oxidized or oxyhemoglobin and allows continuous beat-to-beat calculation of oxygen saturation. The instrument’s ability to accurately calculate saturation can be impaired by hypothermia, hypotension, and vasopressor medications. The placement of an additional pulse oximeter probe on another site in these instances is recommended (at the alternate extremity or a more central location such as ear or nose).
C. Arterial and central venous access.
More significant open vascular cases or cases in which the patient’s blood pressure can be expected to be labile may require an indwelling radial artery line and, occasionally, a central venous catheter. The arterial line allows easier blood sampling for measurements of arterial blood gas, hematocrit, electrolytes, and glucose, as well as continuous blood pressure tracings. The central venous line allows measurements of central venous pressure
(CVP) and infusion of resuscitative fluids and medications at a more brisk rate, depending upon the size of the catheter or sheath.
(CVP) and infusion of resuscitative fluids and medications at a more brisk rate, depending upon the size of the catheter or sheath.
D.
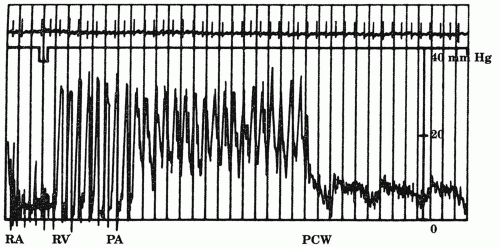
Pulmonary capillary wedge pressure measured with a Swan-Ganz pulmonary artery (PA) catheter is a reliable guide to left-sided (left atrium and left ventricle) filling pressures and even left ventricular function. The PA catheter also allows the measurement of cardiac output and mixed venous oxygen saturations (SVO2) as an indicator of oxygen delivery and end-organ extraction. Although some anesthesia providers prefer a PA catheter in all major open vascular cases, its routine use is controversial, as some studies have shown that is does not improve overall patient outcome. Therefore, use of PA catheters on a selective basis in patients with ventricular dysfunction, unstable angina, or recent myocardial in farction who require open vascular surgery on an urgent or compelling basis is recommended. If there is question about the need for a PA catheter, the surgeon and anesthesia pro vider should discuss the indications in the context of the overall operative plan. If it remains unclear whether or not a PA catheter will be needed, an introducer can be placed in a central vein at the start of the operation allowing for the catheter to be placed later if necessary. Figure 9.1 illustrates the pressure tracings as the Swan-Ganz catheter is floated through the right heart to a wedge position in a pulmonary artery. Although there are complications related to the use of a PA catheters, most of the risks are incurred in the process of obtaining central venous access.
Oximetric PA catheters allow continuous monitoring of SVO2, which is an early indicator of change in the patient’s physiologic well-being. SVO2 may be used to assess the effectiveness of a specific intervention, with a decrease in saturation indicating worsening oxygen delivery (e.g., myocardial infarction) or increased end-organ extraction (e.g., sepsis). An SVO2 of less than 60% indicates physiologic compromise and should prompt a reevaluation of the patient, to find the source or explanation. The SVO2 can then be followed as an early measure of treatment success such as the response to administration of an inotropic agent. Oximetric pulmonary artery catheters are more expensive than the standard PA catheters and should only be placed in cases where such physiologic detail will be used. Despite the physiologic information that this technology provides, the value of the Swan-Ganz catheter is debatable, as some prospective studies have shown its routine use does not improve mortality.
E.
Transesophageal echocardiography (TEE) is another option for monitoring cardiac function in the operating room, but it is less commonly used outside of the operating room in the postoperative setting. TEE is a sensitive method to detect myocardial ischemia manifest by the development of myocardial wall motion abnormalities and can accurately assess left ventricular filling and function (e.g., ejection fraction).
F.
Core temperature monitoring is critical for all open aortic or extremity vascular cases that last for more than two to three hours. Hypothermia (<35°C) is associated with risk for cardiac events, including ventricular tachycardia related to elevated levels of circulating catecholamines. In addition, hypothermia contributes to coagulopathy by adversely effecting the enzymes that participate in the clotting cascade. Esophageal, intravenous, or bladder thermistor monitoring are all generally accurate. Warming the operating room to 75°F before the patient enters and using warm air plastic drapes (Bair Hugger, Augustine Medical, Inc., Eden Prairie, MN, U.S.A.) are helpful in maintaining the core temperature of the patient.
II. Patient positioning and operating room briefing.
Positioning the patient on the operating or endovascular table is critical and should occur as part of the final time out or operating room briefing program. This preparatory step assures that the members of the team know each other as well as the patient and the planned procedure, including its stepwise conduct. The surgical site and procedure are reviewed and critical steps and necessary equipment are anticipated among the four key players in the room: surgeon or endovascular specialist, surgical assistant, circulating nurse, and anesthesia provider. Optimally, this briefing is led by the surgeon or endovascular specialist and occurs with all present at the same time. The operating room briefing program has been shown to serve in conjunction with the more basic and familiar “time out” to reduce wrong patient and wrong site procedures and to improve overall patient safety and procedural efficiency in the operating room and endo vascular suite.
Once the final time out or operating room briefing has occurred, final patient positioning and setup can take place. Special attention should be paid to whether or not to tuck the patient’s arms next to his or her side on the table and where any fluoroscopic imaging will take place during the procedure. Again, anticipation and planning before the final sterile preparation and draping is critical for a safe, effective, and efficient procedure.
In addition to positioning for proper retraction and/or fluoroscopic imaging, patient positioning has been shown to be critical




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree