Myocardial Infarction with normal coronary arteries (MINCA) is common with a prevalence of 1% to 12% of all myocardial infarctions. The pathogenic mechanisms of MINCA are still unknown, but endothelial dysfunction has been suggested as a possible cause. To investigate risk factors and markers for MINCA, we conducted a case–control study. Considering the reported low prevalence of classical risk factors for coronary heart disease (CHD) in some but not all studies, our hypothesis was that endothelial function and intima–media thickness (IMT) were better, respectively lower, than CHD controls. One hundred patients with MINCA fulfilling diagnostic criteria according to the European Society of Cardiology/American Collage of Cardiology/American Heart Association universal definition of myocardial infarction with myocarditis excluded by cardiac magnetic resonance imaging were investigated. Risk factors, endothelial function (EndoPAT), and IMT were compared to gender- and age-matched patients with myocardial infarction and CHD, respectively healthy controls. Smoking, hypertension, impaired glucose tolerance and diabetes mellitus, inflammatory disease, and psychiatric disorders were more common in patients with MINCA than in healthy controls. In contrast to patients with CHD, the lipid profile was antiatherogenic with low low-density lipoprotein and high high-density lipoprotein cholesterol. There were no major differences between the groups regarding endothelial function and IMT that were in the normal range. In conclusion, the present study showed that MINCA was associated with many established cardiovascular risk factors without major differences in atherosclerosis markers. MINCA patients recalled a high prevalence of emotional stress before admission that together with previous psychiatric vulnerability and female gender speaks strongly in favor of Takotsubo syndrome being an important cause of MINCA.
To investigate risk factors and markers for myocardial infarction with normal coronary arteries (MINCA), we conducted a case–control study. In the Stockholm Myocardial Infarction with Normal Coronaries (SMINC) study, we compared patients with MINCA with age- and gender-matched patients with coronary heart disease (CHD) and healthy controls. Considering a reported low prevalence of classical risk factors for CHD in some but not all studies, our hypothesis was that endothelial function and intima–media thickness (IMT) were better, respectively lower, than CHD controls.
Methods
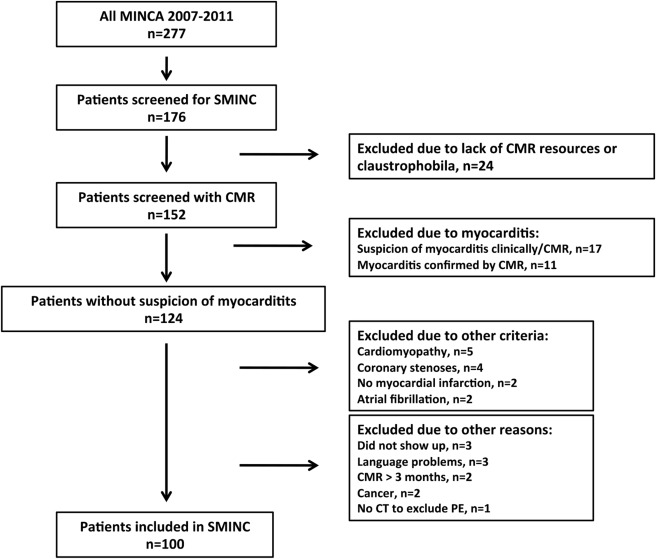
From June 2007 to May 2011, a total of 176 patients were screened at five coronary care units in the Stockholm metropolitan area. Patients aged from 35 to 70 years fulfilling the diagnostic criteria of acute myocardial infarction and a coronary angiogram with no or minimal signs of atheromatosis were eligible for the study; thus patients with Takotsubo Syndrome (TS) were included. Minimal atheromatosis was defined as small irregularities in the coronary vessel wall, giving rise to <30% reduction of the vessel lumen with all coronary angiograms independently examined by a second angiographer. Acute myocardial infarction was diagnosed according to the European Society of Cardiology/American Collage of Cardiology/American Heart Association universal definition of myocardial infarction, and the diagnosis of TS was based on the Mayo clinic diagnostic criteria. Patients with a history of structural heart disease, CHD, pacemaker, severe chronic obstructive pulmonary disease with hypoxemia due to acute exacerbation, severe renal failure (serum creatinine >150 μmol/L), or lack of sinus rhythm on admission were excluded. Medical records of all patients were examined by a cardiologist unrelated to the study to exclude patients not fulfilling the criteria for myocardial infarction. The first 100 patients underwent computed tomography (CT) of the chest to exclude pulmonary embolism, but because all turned out negative, the protocol was changed to measurement of d -dimer and CT only in case of high suspicion of pulmonary embolism. Cardiac magnetic resonance (CMR) imaging was performed in 152 patients mainly to exclude myocarditis. The screening process, including CMR results, has been described. Subsequently a total of 100 patients with MINCA were included ( Figure 1 ).
All 100 patients with MINCA were individually matched by gender and age (within ± 5 years) to 2 control groups: patients with myocardial infarction with CHD and healthy controls. Matching CHD controls were recruited during hospital stay or at follow-up at the respective coronary care unit. Healthy controls were recruited from the Stockholm population registry (2007 to 2008) or from the computer-based medical record system TAKE CARE containing all citizens in Stockholm (2009 to 2012). The controls were selected randomly by date of birth and gender to match cases and contacted for participation by an invitation letter followed by a telephone call. Ten missing healthy controls were recruited among staff, relatives, and controls’ friends. The participation proportion was approximately 50%. All healthy controls were free of symptomatic CHD and performed a normal exercise stress test.
The study was performed in accordance with the Declaration of Helsinki and Good Clinical Practice and was approved by the Stockholm Ethics Committee. For inclusion, patients were asked to give written informed consent. Each patient was assigned a study identification number, and a record for information was established and kept secured at the Cardiology Unit at Karolinska University Hospital in Solna, Sweden.
Smoking was defined as any active regular use and ex smoking as any history of regular use. Hypertension and hyperlipidemia were defined as previously diagnosed and medically treated. Diabetes mellitus was defined as previously diagnosed. Inflammatory diseases included diagnosed asthma, chronic obstructive pulmonary disease, rheumatologic diseases, pancreatitis, hepatitis, primary biliary cirrhosis, diverticulitis, collagenous colitis, and chronic tooth infection. Osteoarthritis was not included. Psychiatric disorders included depression, anxiety disorder, sleeping disorder, bipolar disorder, anorexia, social phobia, attention deficit disorder, and chronic fatigue syndrome. Thromboembolic disorders included previous thromboembolic diagnoses and known coagulopathy. Medical records were retrospectively examined by 2 of the authors (MD, CE) searching for evidence of physical and emotional stress precipitating the acute event and to confirm information regarding inflammatory diseases and psychiatric disorders.
The following data, analyzed by routine clinical chemistry, were acquired from medical records at admission for patients with MINCA and CHD controls; plasma C-reactive protein (mg/l), fasting plasma triglycerides (mmol/l), fasting plasma cholesterol (mmol/l), fasting plasma low-density lipoprotein (LDL) cholesterol (mmol/l), and fasting plasma high-density lipoprotein (HDL) cholesterol (mmol/l). Peak troponin (I or T; μg/l) or high-sensitive troponin T (ng/l) ratios were calculated relatively to the upper limit of normal. An oral glucose tolerance test was performed 2 to 3 days after admission or 6 weeks after discharge by determination of the plasma concentration of glucose (mmol/l) 2 hours after ingestion of 75-g glucose dissolved in 150 ml of water. A plasma glucose concentration >7.8 mmol/l was considered impaired glucose tolerance (IGT). Corresponding blood chemistry was analyzed at the study visit for the healthy controls. Additional blood sampling was performed at the time of a 3-month follow-up visit for patients with MINCA and CHD controls and at the study visit for the healthy controls. Plasma was stored at −80 C for subsequent analyses. Analysis of NT-proBNP (ng/l) was performed 3 months after the acute event by an electrochemical luminescence technique (Roche) to determine myocardial dysfunction.
Endothelial function was measured 3 months after the acute event with EndoPAT (Itamar-Medical Ltd), a specialized device for assessment of endothelial function. The EndoPAT system is based on peripheral arterial tone (PAT) signal technology; a noninvasive plethysmographic method measuring pulsatile volume changes in the digital bed. The test is user independent and automatically calculated and was performed in a thermoneutral and quiet surrounding avoiding pretest consumption of caffeine and smoking. The test quantifies endothelium-mediated changes in vascular tone elicited by a 5-minute occlusion of the brachial artery using a standard blood pressure cuff inflated to a suprasystolic pressure. When the cuff is deflated, the surge of blood flow causes an endothelium-dependent flow-mediated dilatation leading to reactive hyperemia and an increase in the PAT signal amplitude. Measurements from the contralateral probe are used to control for non–endothelial-dependent changes in vascular tone. The postocclusion to preocclusion ratio, called EndoScore or reactive hyperemia index (RHI), is calculated with specialized software.
Two-dimensional images of the left and right common carotid artery (CCA) were acquired, using an ultrasound scanner (Vivid 7; General Electric [GE], New York) equipped with a 12-MHz transducer, 3 months after the acute event. From each CCA, a long-axis cine loop of 3 beats and 3 diastolic images at the time of the electrocardiographic R-wave was stored digitally on magnet-optic discs for offline analysis. The IMT of the CCA far wall was measured in 3 diastolic images from each side using GE semiautomatic IMT analysis software. A 10-mm region of interest was manually placed starting 1 cm proximal to the carotid bulb. The intima–media borders of the far wall, toward the lumen and the adventitia, were identified automatically by the program. Manual correction was not performed, and in case of suboptimal tracking, the region of interest could be adjusted somewhat or another diastolic frame chosen. IMT was calculated as mean of 3 semiautomatic measurements. A mean of the results of IMT of the left and right CCA was calculated and used for comparison between the groups.
The primary end point was endothelial function measured by EndoPAT. A sample size estimation, using RHI as a continuous variable, was performed after investigation of 41 patients with MINCA and 23 CHD controls that showed an absolute 0.27% larger RHI in patients with MINCA. A number of 100 patients with MINCA and 100 CHD controls were calculated to give the study a power of 83% to show that patients with MINCA had larger RHI than CHD controls (p <0.05).
Values are presented as mean ± standard deviation (SD), percent (%), or interquartile range (IQR). Group-wise comparisons were made by the Mann–Whitney U test or the Kruskal–Wallis test for continuous variables. A chi-square test was used for categorical data. A p value of <0.05 was considered significant.
Results
The mean age of patients with MINCA and controls was 58 to 59 years. The vast majority were women (72%). Twenty-five percent of the patients with MINCA fulfilled all Mayo Clinic diagnostic criteria for TS. Another 19% showed less prominent abnormal ventricular wall motion (regional hypokinesia/akinesia/dyskinesia) on imaging with left ventriculography or echocardiography, suggestive of TS in regression or a milder state. Fifty-six percent of all patients with MINCA had a history of physical or emotional stress before admission. Eighteen percent of the patients with MINCA, respectively 41% of the CHD controls presented with ST-elevation. The relative troponin levels were similar in CHD controls compared to patients with MINCA ( Table 1 ).
| MINCA n=100 | CHD n=100 | Healthy control n=100 | MINCA vs CHD (p-value) | MINCA vs control (p-value) | |
|---|---|---|---|---|---|
| Age (years) | 58 ± 8 | 59 ± 8 | 59 ± 8 | – | – |
| Women | 72 % | 72 % | 72 % | – | – |
| BMI (kg/m 2 ) | 26 ± 5 | 27 ± 5 | 25 ± 4 | 0.037 | 0.557 |
| Heart rate (bpm) | 74 ± 15 | 75 ± 14 | 69 ± 15 | 0.706 | n.a. |
| Systolic blood pressure (mm Hg) | 147 ± 27 | 149 ± 27 | 128 ± 17 | 0.492 | n.a. |
| Troponin, ratio to normal | 110 ± 176 | 275 ± 560 | – | 0.642 | – |
| C-reactive protein > 5 μg/L | 16 % | 13 % | 5 % | 0.699 | 0.010 |
| Smoker | 21 % | 33 % | 7 % | 0.056 | 0.004 |
| Ex-smoker | 29 % | 34 % | 40 % | 0.447 | 0.102 |
| Hypertension | 37 % | 46 % | 17 % | 0.196 | 0.001 |
| Hyperlipidemia | 9 % | 20 % | 4 % | 0.027 | 0.152 |
| Diabetes mellitus | 4 % | 10 % | 0 % | 0.096 | 0.043 |
| Impaired glucose tolerance and diabetes mellitus | 39 % | 55 % | 20 % | 0.029 | 0.004 |
| Migraine | 14 % | 13 % | 13 % | 0.836 | 0.836 |
| Thrombembolic disorder | 6 % | 1 % | 2 % | 0.054 | 0.149 |
| Inflammation | 30 % | 20 % | 10 % | 0.102 | <0.001 |
| Psychiatric disorder | 20 % | 11 % | 3 % | 0.079 | <0.001 |
| Triglycerides (mmol/L) (mg/dl) | 1.0 ± 0.5 89 ± 44 | 1.4 ± 0.7 124 ± 62 | 1.0 ± 0.6 89 ± 53 | <0.001 | 0.096 |
| Cholesterol (mmol/L) (mg/dl) | 5.1 ± 1.0 197 ± 39 | 5.4 ± 1.1 209 ± 43 | 5.6 ± 1.0 217 ± 39 | 0.092 | <0.001 |
| Low density lipoprotein cholesterol (mmol/L) (mg/dl) | 3.0 ± 0.8 116 ± 31 | 3.5 ± 0.9 135 ± 35 | 3.6 ± 0.8 139 ± 31 | 0.002 | <0.001 |
| High density lipoprotein cholesterol (mmol/L) (mg/dl) | 1.6 ± 0.5 62 ± 19 | 1.3 ± 0.4 50 ± 16 | 1.6 ± 0.5 62 ± 19 | <0.001 | 1.000 |
Clinical characteristics of patients with MINCA and their respective controls are presented and compared in Table 1 . Body mass index (BMI) was lower and treatment for hyperlipidemia was less frequent in patients with MINCA than in CHD controls. Present smoking tended to be less frequent in patients with MINCA than in CHD controls but was more common than in healthy controls. The prevalence of treatment for hypertension was similar in patients with MINCA and CHD controls but higher than in healthy controls. A history of diabetes mellitus was more common in patients with MINCA than in healthy controls, whereas the combination of IGT and a history of diabetes mellitus was less frequent in patients with MINCA than in CHD controls but more common than in healthy controls. A history of inflammatory disease and psychiatric disorders was more common in patients with MINCA than in healthy controls. Plasma triglycerides were lower in patients with MINCA than in CHD controls. Plasma LDL cholesterol was lower in patients with MINCA than in both CHD and healthy controls, whereas plasma HDL cholesterol was greater in patients with MINCA than in CHD controls. Patients with MINCA fulfilling all Mayo clinic diagnostic criteria for TS had similar characteristics compared to patients with MINCA without any criteria except for female gender and psychiatric disorders that were more common in TS ( Table 2 ).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


