Chapter 22 Rigid Bronchoscopy with Laser and Stent Placement for Bronchus Intermedius Obstruction from Lung Cancer Involving the Right Main Pulmonary Artery
Case Description
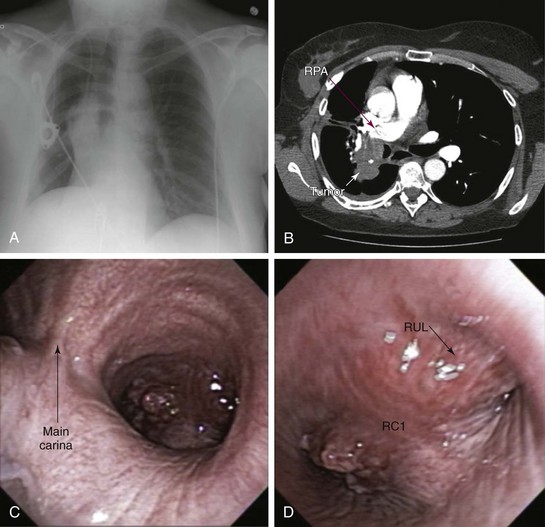
A 50-year-old female with a 30–pack-year history of smoking developed wheezing and worsening shortness of breath, limiting her daily activities. Right lateral decubitus position worsened her symptoms, and she could not sleep on her right side. She was admitted to an outside hospital, where flexible bronchoscopy showed complete obstruction of the right upper lobe bronchus and severe obstruction (≈80%) of the bronchus intermedius (BI). She was transferred for bronchoscopic restoration of airway patency. The patient had a history of stage III squamous cell carcinoma of the lung diagnosed 18 months previously. Her pulmonary function test at that time showed a vital capacity of 2.94 L (80% predicted) and FEV1 of 2.39 L (85% predicted). She received neoadjuvant chemotherapy and radiation therapy followed by right lower lobectomy and mediastinal node dissection; all nodes were negative. The primary tumor measured 2.5 × 2 × 2 cm and extended to the parenchymal resection margins; evidence showed peritumoral lung consolidation related to the secondary effects of radiation therapy. Shortly after undergoing treatment, the patient lost her insurance coverage and was unable to pursue clinical or imaging surveillance. Comorbidities included rheumatoid arthritis (RA) requiring methotrexate and prednisone 20 mg/day and bipolar disorder treated with valproic acid. She was unemployed and divorced and lived with her children. Her physical examination was remarkable for expiratory wheezing noted in the right lung field. No limitation of cervical spine mobility was detected, but she had ulnar deviation of her hands and swan neck deformities of her fingers. She had significant functional impairment with a KPS score of 30 and was scored ECOG 3. Chest radiography showed a prominent hilar mass and right middle lobe atelectasis (Figure 22-1, A). Chest CT revealed a mass measuring 4 × 7 × 3 cm that invaded the BI and encased the right pulmonary artery (Figure 22-1, B). Repeat flexible bronchoscopy showed a near complete mixed pattern of obstruction (by exophytic tumor and extrinsic compression) of the BI, but right middle lobe bronchial segments were patent. The right upper lobe bronchus was occluded by extrinsic compression (Figure 22-1, C and D), but the flexible bronchoscope could be passed beyond the occluded airway, noting patent anterior and apical segmental bronchi (see video on ExpertConsult.com) (Video V.22.1![]() ). Echocardiogram showed a systolic pulmonary artery pressure of 60 mm Hg and a moderately dilated right atrium but normal bilateral ventricular size and function.
). Echocardiogram showed a systolic pulmonary artery pressure of 60 mm Hg and a moderately dilated right atrium but normal bilateral ventricular size and function.
Discussion Points
1. Enumerate four anesthesia considerations during rigid bronchoscopic laser resection in this patient in light of severe bronchial obstruction and pulmonary artery involvement.
2. Enumerate three different types of stents that could be inserted in this patient with incomplete obstruction of the bronchus intermedius and right upper lobe bronchus.
3. Explain differences in tissue penetration and coagulation effects of neodymium-doped yttrium aluminum garnet (Nd:YAG), CO2, and potassium-titanyl-phosphate (KTP) lasers, and describe pertinent clinical implications for treating obstructive airway lesions.
4. Describe the principle of power density and its effect on tissues when the Nd:YAG laser is used.
Case Resolution
Initial Evaluations
Physical Examination, Complementary Tests, and Functional Status Assessment
This patient’s focal wheezing on auscultation of the right chest suggests airflow obstruction distal to the carina.1 Positional wheezing suggests a component of dynamic obstruction such as excessive dynamic airway collapse, malacia, or, as in our patient, positional worsening in an already narrowed airway. When localized to a bronchus, these processes will be worsened in the lateral decubitus position.
The hand-joint deformities seen in this patient are characteristic of advanced rheumatoid arthritis (RA) and may predict involvement of the axial skeleton,2 of which the cervical spine joints are the most clinically important, with a prevalence of involvement ranging from 15% to 86%.3 This patient had no symptoms of instability related to atlantoaxial (C1-C2) or subaxial (below C1-C2) subluxation. These include neck pain, stiffness, and radicular pain, all of which should be explored in cases of rigid bronchoscopy or endotracheal intubation. During these procedures, the cervical spine is hyperextended to align the mouth, larynx, and trachea. In one study, preoperative cervical spine assessment with cervical spine films in asymptomatic patients with RA before elective surgery revealed an incidence of unsuspected C1-C2 subluxation of 5.5%.4 Subluxations can vary over time, may be unrecognized, and can be fatal in up to 10% of patients because of spinal cord or brainstem compression.5 Because of the dangers of neck movements required for intubation, and because subluxation is not always symptomatic, radiographic evaluation of the cervical spine probably should be considered for all patients with RA scheduled to undergo procedures requiring cervical manipulation.6
The cricoarytenoid joint may be involved in 30% of patients with RA. Hoarseness and stridor in patients with RA suggest laryngeal involvement and are present in 75% of patients,7 but those with chronic cricoarytenoid arthritis may be relatively asymptomatic. Any disease process leading to hyperventilation, increased airflow (exertion, acidosis, infection), or reduction in the diameter of the airway (upper respiratory infection) can precipitate symptoms.8 In addition, patients with cricoarytenoid arthritis are at risk both during intubation and after extubation. Intubation may be difficult if the airway is narrow and, even if atraumatic and of short duration, can prompt mucosal edema and further compromise of airway caliber, leading to airway obstruction and stridor following extubation.9 Systemic glucocorticoids are often effective in reversing the obstruction caused by acute cricoarytenoid arthritis, and local periarticular steroid injections have been shown to improve cricoarytenoid function. In chronic cricoarytenoid arthritis, the degree of airflow limitation dictates the need for laser cordotomy or arytenoidectomy.10 Other potential manifestations of RA that could interfere with airway management include limited temporomandibular joint (TMJ) mobility (<4.5 cm), which is present in approximately 66% of patients with long-standing RA. Most of these patients experience pain and tenderness in the TMJ. Upper airway obstruction can occur because of pharyngeal obstruction, as in patients with micrognathia or obstructive sleep apnea. Furthermore, a small mouth opening from TMJ disease may preclude rigid bronchoscopic intubation. In our patient, upper airway anatomy was normal, and no signs of RA-related laryngeal involvement or TMJ disease were noted.
Comorbidities
This patient had been diagnosed with bipolar disorder. Although possibly attributable to higher unmeasured severity of illness in patients with psychiatric comorbidity, existing psychiatric disease has been found to be associated with a modestly increased risk of death among patients undergoing surgery.11 Our patient had been taking prednisone 20 mg/day for many years. The equivalent of 15 mg/day of prednisone for longer than 3 weeks should raise suspicion for hypothalamic-adrenal axis suppression,12 warranting increased glucocorticoid supplementation associated with possible adrenal insufficiency related to medical and surgical stress.12 In this regard, one must recall that supplemental corticosteroids can induce or exacerbate manic or depressive episodes, potentially interfering with postoperative care.13
Support System
1. Mental illness is associated with higher case-fatality rates in patients with cancer, in part because of the challenges of drug interactions, lack of capacity, and difficulties in coping with treatment regimens as a result of psychiatric symptoms. A multidisciplinary approach that includes members of mental health services is warranted to ensure effective treatment and to avoid inequalities of care that might result from physician biases or mismanagement of patient behaviors and treatment choices.14
2. Nonoperative non–small cell lung carcinoma (NSCLC) trials showed that marital status was not independently predictive of overall survival; however, single females had significantly better overall survival than both single and married males.15
3. Socioeconomically disadvantaged patients with NSCLC may receive less intensive cancer-specific care. Differences in access to care, comorbidities, and lifestyle may contribute to these inequalities.16
Patient Preferences and Expectations
This patient wished to improve her shortness of breath, which caused significant emotional and physical distress. Results from studies show that more than 50% of patients with inoperable lung cancer report breathing difficulty, pain, and fatigue as the symptoms most associated with physical and emotional distress.17
Procedural Strategies
Contraindications
The lack of functional lung distal to the obstruction would preclude bronchoscopic interventions. In this patient, however, flexible bronchoscopy showed a patent RML bronchus. No absolute contraindications to rigid bronchoscopy were noted, nor did concerns arise regarding RA-related upper airway obstruction. The cervical spine range of motion was normal, and dynamic (flexion-extension) magnetic resonance imaging (MRI) showed no evidence of cord compression. Entrapment of the right pulmonary artery by the tumor (see Figure 22-1) could result in hemodynamic instability during general anesthesia owing to high risk for acute cor pulmonale.
Expected Results
Relief of BI obstruction was expected to improve her lung function and potentially her dyspnea by restoring ventilation to the right middle lobe. A vast majority of patients with malignant central airway obstruction (CAO) improve their dyspnea and performance status if the CAO is palliated. The modality used to restore airway patency (i.e., laser, stent, photodynamic therapy [PDT], electrocautery, or brachytherapy) depends on tumor characteristics (i.e., extrinsic, endoluminal, or mixed) and severity and type of obstruction (i.e., critical, compromising respiratory status), operator preference, and availability of specific technologies.18 The modality used to restore airway patency might not make a difference in terms of outcome, suggesting that it is restoration of airway patency per se that counts, not the method used to achieve it.19 Survival may also be improved, especially if further systemic therapy can be initiated post procedure. Overall, the median survival of patients with untreated malignant CAO can be as low as 1 to 2 months.20 If interventional bronchoscopy is successful in relieving airway obstruction, survival is similar to that in patients without CAO.21 Stent insertion results in significant improvement in Medical Research Council Dyspnea Scales (MRC)-measured dyspnea and Eastern Cooperative Oncology Group (ECOG) performance status, although in one study, a significant survival advantage was seen only in the intermediate performance group (ECOG ≤3, MRC ≤4) when compared with historic controls. Perhaps improved survival is noted if airway patency is restored before the development of complications such as post obstructive pneumonia, irreversible atelectasis, or loss of ventilatory function from malignant CAO.22
Therapeutic Alternatives
• External beam radiation therapy (EBRT) for recurrent locally advanced NCSLC previously treated with radiation therapy is a feasible, noninvasive therapeutic alternative.23 However, when associated severe airway obstruction results in atelectasis, the response rate is 20% to 50% in studies involving more than 50 patients.24 Smaller studies showed that bronchial obstruction could be relieved in up to 74% of patients, resulting in complete or partial re-expansion of the collapsed lung. The time to initiation of treatment matters because 71% of patients irradiated within 2 weeks after radiologic evidence of atelectasis had complete re-expansion of their lungs, compared with only 23% of those irradiated after 2 weeks.25 In our patient, EBRT was potentially limited by evidence of radiation-induced toxicity from previous radiotherapy. Improvements in imaging and treatment planning using three-dimensional (3D) conformational radiation and respiratory gating can precisely target radiotherapy, and by decreasing the normal tissue margins included to account for uncertainties in position, can diminish the risk of clinically significant pneumonitis and esophagitis.26
• Endobronchial brachytherapy (EBB) has proven efficacy in patients with endoluminal tumor and a substantial extrabronchial component. For palliation of NSCLC symptoms, EBB alone appears to be less effective than EBRT. For this patient previously treated with EBRT, who was symptomatic from recurrent endobronchial CAO, EBB is a reasonable alternative.27 Success rates vary between 53% and 95%,28 but the overall incidence of fatal hemoptysis is 10% (range, 0% to 42%). Irradiation in the vicinity of major vessels, in this case the right pulmonary artery, increases bleeding risk.29 In fact some authors suggest that patients with tumors involving the major vessels should be excluded from EBB.30 Squamous cell pathology and tumor located in the mainstem bronchus or upper lobe represent additional risk factors for hemoptysis.31 Patients with poor performance status may be at higher risk for periprocedural complications such as cough, bronchospasm, and pneumothorax caused by catheter placement.
• Photodynamic therapy (PDT) could be provided, but because of the severe nature of the airway obstruction, the sloughed tissue resulting from PDT could occlude the airway and cause complete obstruction, resulting in worsening symptoms and post obstructive pneumonia.32 This patient’s previous surgery, chemotherapy, and radiation therapy did not represent contraindications to PDT, and in fact this therapy can be offered to patients who become unresponsive to chemotherapy or radiation therapy.33 PDT is most effective when obstruction from mucosal disease is greater than 50% and in patients with good performance status.34 Hemorrhage has been reported in 0 to 2.3% of patients, but the risk may be greater when the disease involves major blood vessels.
• Cryotherapy would address only the endoluminal component of the obstructing airway lesion. It can be combined with EBRT to enhance its efficacy.35 The effect is delayed, and initially sloughed tissue resulting from vasoconstriction and necrosis might worsen airway obstruction. Cryotherapy is reportedly effective in up to 75% of patients with lung cancer with endoluminal obstruction,36 but it is not the therapy of choice when extrinsic compression is present.
• Argon plasma coagulation (APC) and electrocautery allow removal of exophytic disease.18 Systemic, life-threatening APC-related gas embolism has been reported.37 Risks may be increased when highly vascularized lesions are treated and in proximity of large blood vessels. Depth of penetration and distribution of thermal-induced necrosis within tissues are not as predictable as they are with lasers because electrical current follows the path of least electrical resistance within different tissue types.
• Metal stents are more costly than silicone stents, but procedures can be performed via flexible bronchoscopy with or without fluoroscopy.38 Therefore it is an appropriate alternative, especially in patients with significant comorbidities precluding general anesthesia.
• Silicone Y stent insertion at the right primary carina (RC1) was shown to improve symptoms in a small published case series of three patients with malignant disease. The bronchial limbs of the stent saddled the involved carina between the bronchus to the right upper lobe and the bronchus intermedius.39 The very wide RC1 and the near complete obstruction in the RUL bronchus precluded this approach in our patient.
• Comfort care without palliative bronchoscopic intervention is not an unreasonable approach to treating this patient with poor quality of life and a grim prognosis. A palliative care consultation and potential initiation of hospice care, especially if quality of life continues to deteriorate, should be considered, regardless of other therapeutic alternatives.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree