INDICATIONS
Video-assisted thoracoscopic surgery (VATS) lobectomy is most commonly used to treat conditions of the lung parenchyma requiring resection of an entire lobar section of the lung. The most frequent indications for this approach are either early-stage tumors of the lung, or infectious diseases causing destruction of a significant portion of the lobe. A list of indications for a VATS lobectomy include the following.
Clinical stage I nonsmall cell lung cancer (NSCLC)
Uncharacterized but suspicious pulmonary nodules which are not amenable to wedge resection
Mycetoma contained in the lung parenchyma
Atypical mycobacterial infections causing destruction of the majority of the parenchyma of the lobe intended for resection
Pulmonary sequestration
 RELATIVE CONTRAINDICATIONS
RELATIVE CONTRAINDICATIONS
Contraindications to VATS lobectomy are relative based on the experience of the operator. Nearly all forms of surgically treated lung cancer have been reported to be undertaken via a VATS approach with success; however, these approaches may not apply to the general population of thoracic surgeons who do not encounter these cases with great volume. Although concerns over the adequacy of VATS lobectomy have been addressed extensively in treating stage I NSCLC, there is far less data regarding the ability to treat higher stages effectively and should be used with caution unless the operator has significant experience with this approach. In general relative contraindications to a VATS lobectomy include the following.
NSCLC higher than stage I
Tumors invading the chest wall
Tumors invading the hilum
NSCLC with macroscopic lymph node involvement
Failure to progress after a reasonable time with the VATS approach
Aberrant vascular or bronchial anatomy
Complete pleural symphysis
 PREOPERATIVE PLANNING
PREOPERATIVE PLANNING
The preoperative planning for a patient undergoing VATS lobectomy is similar for all lobes of the lung and centers mainly around evaluation of a patient’s functional and cardiopulmonary status as well as adequate tumor staging in the event of a malignancy. All patients should have basic spirometry and diffusion capacity measurements as well as a measurement of oxygen saturation during a 6-minute walk test. Quantitative perfusion scanning should be undertaken in patients with more marginal pulmonary function. Cardiac evaluation consists mainly of some form of myocardial stress testing and an echocardiogram to evaluate pulmonary artery pressures, valvular function, and ventricular function. The evaluation of a patient’s physical ability to withstand the operation is much more subjective. In general I am reluctant to perform a VATS lobectomy on wheelchair or bed-bound nonambulatory patients. Demonstrating an ability to independently ambulate as well as strong family support are positive indicators for success. The use of supplemental oxygen should not be an absolute contraindication as its use has increased with the treatment of chronic obstructive pulmonary disease and sleep apnea. Careful history taking can usually help determine whether the use of supplemental oxygen in a particular patient is an actual contraindication. Preoperative physiologic testing prior to a VATS lobectomy may be summarized by the following:
Always:
Spirometry
Diffusion capacity
Myocardial stress test
Echocardiogram
Occasional:
Quantitative perfusion scanning
Six-minute walk
Stair climb
Significant attention should be paid to preoperative imaging studies regarding staging of potential tumors, anatomy of airways and vasculature, and extent of lung destruction in the event of an infectious process. The most helpful imaging study in the preoperative planning of a VATS lobectomy is a contrast-enhanced computed tomography (CT) of the chest. Although intravenous contrast is not often used for lung cancer screening imaging it is extremely helpful in ensuring there is no unusual vascular anatomy or for determining adherence of a lesion to the pulmonary artery. Observation of the relationship of any lesion to the fissure anatomy is very important to determine whether a VATS lobectomy is feasible. 18Flourodeoxyglucose positron emission tomography (FDG-PET) is somewhat useful in predicting nodal disease. This will not be discussed in great detail here; however, the main use of FDG-PET will be to exclude patients from the VATS procedure if there is evidence of significant lymph node involvement or satellite lesions identified. Occasionally, imaging findings can be used to help counsel a patient about the possibility of converting from a VATS to an open procedure based on the above data obtained from a scan.
 SURGERY
SURGERY
The discussion of the surgical technique of a VATS lower lobectomy begins below and the specifics of achieving the operation will be discussed. It is important to realize several underlying themes when performing these procedures no matter which lobe is being resected. The key point to all of the techniques described is that they should be as constant and fixed as possible from procedure to procedure. This means that the port placement should be similar for all lobes, ports of access for staplers, although differing according to the type of lobe removed, should not deviate, direction of retraction, and order of transection of tubular structures also should be as consistent as possible from case to case. This rigid adherence may seem counterintuitive given the differences in body habitus and anatomic relationships but one of the most powerful indicators that something is going wrong with a case is the inability to achieve a step of the procedure similar to previous cases. I cannot emphasize enough that when beginning to perform these procedures the failure to achieve a step of the operation as done previously should be an indication to open the patient and figure out why prior to inadvertently transecting or injuring a structure that may not be able to be repaired.
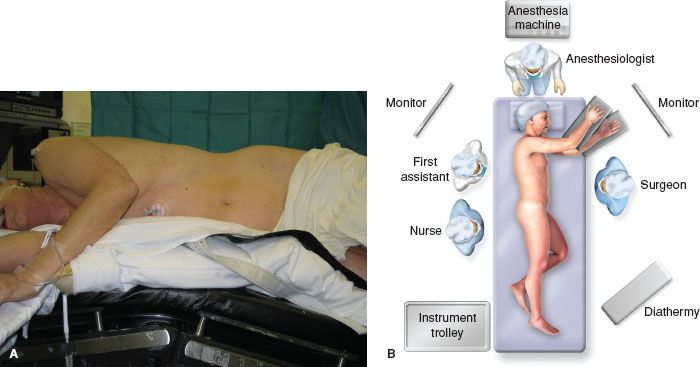
Figure 14.1 A: Standard positioning for VATS pulmonary procedures. B: Schematic description of operating room configuration for most VATS procedures.
Positioning
Positioning for all patients undergoing a VATS lobectomy is the same. The patient is placed in the lateral decubitus position with the bed maximally flexed with the breakpoint just above the superior iliac crest. This reduces the interference caused by the hips and serves to spread the rib spaces as much as possible (Fig. 14.1). Any increase in the space between the ribs will reduce the difficulty of the procedure. A schematic view of the operating room setup is illustrated in (Fig. 14.1).
Port Site Placement
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


