INDICATIONS/CONTRAINDICATIONS
Most common indications for lobectomy include bronchiectasis, mycetoma, hemoptysis, hydatid cyst, and cancer. Cancer can further be subdivided into primary or secondary (i.e., pulmonary metastases) disease.
The two major issues, concerning contraindications for surgery, mainly comprise fitness for surgery and operability. While the term “fitness for surgery” includes pulmonary function, cardiovascular fitness, nutrition, and performance status (e.g., Karnofsky index), the issue of “operability” basically consists of diagnosis and staging.
 PREOPERATIVE PLANNING
PREOPERATIVE PLANNING
Once the indication for the surgical procedure is clear, the major factors “fitness for surgery” and “operability” have to be thoroughly checked for an approach for improvement.
Concerning fitness for surgery, there are several factors to be considered: Smoking cessation for a minimum of 2 weeks prior to surgery (3 months for lung volume reduction surgery), a steroid trial to improve lung function in patients with chronic pulmonary obstructive disease, antibiotic therapy in cases of chronic infection or poststenotic pneumonia, adjustment of cardiovascular medication (e.g., beta-blocker dose), food supplementation, and improvement of performance (by preoperative out- or inpatient rehabilitation). Operability can occasionally be influenced by neoadjuvant treatment (i.e., induction chemotherapy).
When planning the surgical procedure itself, possible difficulties such as adhesions (e.g., due to prior operations or trauma, infection, or neoadjuvant chemo- or radiotherapy), hypervascularization with increased risk of bleeding (e.g., after recurrent infections, locally advanced tumor), or central localization of the tumor with expected close resection margins, should be anticipated.
To prevent postoperative respiratory complications, physiotherapy, including instruction of independent exercises, should be started the day before surgery.
 SURGERY
SURGERY
Preparation and Positioning
All patients should receive a prophylactic single-shot dose of antibiotics intravenously 30 to 60 minutes prior to the skin incision. At our institution we use a second generation cephalosporin (1.5 g of cefuroxime) or a second generation fluoroquinolone antibiotic (500 mg of ciproxin) in case of allergy to penicillin. A thoracic epidural catheter is inserted for peri- and postoperative pain control prior to the operation while the patient is awake and cooperative. The operation is performed with the patient under general anesthesia. Usually a single-use, left-shaped double-lumen endotracheal tube is positioned in the left mainstem bronchus. As an alternative, for patients with difficult, narrow airways, a single-lumen tube may be inserted with the additional use of a bronchial blocker to allow the requested one lung ventilation (be aware that it is more difficult to exclude the lung from ventilation on the right than on the left side, due to the shorter length of the mainstem bronchus).
Now the patient is placed on a vacuum mattress and brought into a semisupine position. The right arm is elevated to 90 degrees in front of the patient and flexed in the elbow to a 90-degree angle. Care has to be taken to support the right arm on a well-cushioned overhead bar to prevent both compression and traction to the neurovascular bundle. Now the right hemithorax is disinfected and draped.
Technique
Thoracotomy
For anterolateral thoracotomy, the skin incision comes to lie at the inframammary fold and extends laterally in the direction of the inferior angle of the scapula. After the subcutaneous tissue is divided, the serratus anterior muscle is separated parallel to the direction of the muscle fibers over the fifth rib. Laterally the latissimus dorsi muscle is retracted posteriorly (Fig. 13.1). After installation of single lung ventilation, the intercostal muscles and the parietal pleura are divided just below the fifth rib, sparing the neurovascular bundle.
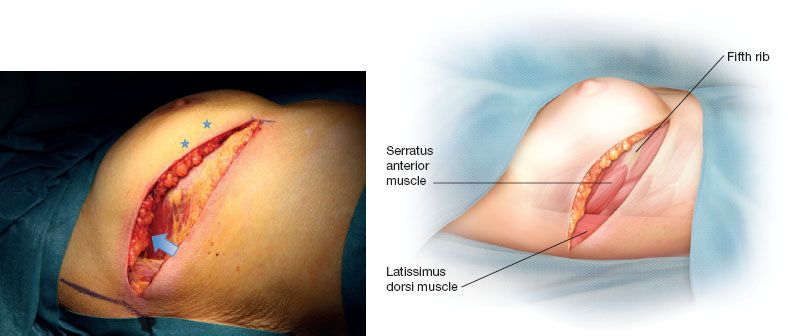
Figure 13.1 Anterolateral thoracotomy: Skin incision in the submammary fold, the latissimus dorsi muscle (arrow) is retracted posteriorly. The thoracic cavity is entered under the fifth rib (rib marked with stars).
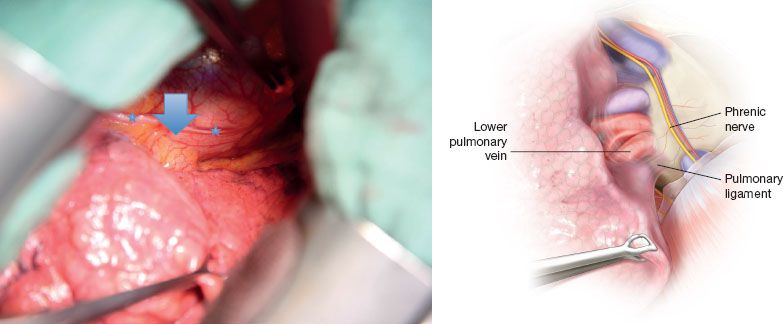
Figure 13.2 Pulmonary ligament and lower pulmonary vein (marked with arrow). Phrenic nerve (marked with stars).
Exploration of the Thoracic Cavity
The thoracic cavity is inspected and the exact position of the tumor including its resectability is evaluated. Suspicious pleural fluid, if present, is aspirated for cytologic examination. Strong adhesions are dissected if tumor invasion is suspected an extrapleural dissection is advisable. For suspected thoracic wall invasion, as well as for suspected mediastinal tumor invasion, frozen section analysis may be helpful in the decision making of chest wall resection or even questionable resectability.
Exposure of the Hilum and Vein
The mediastinal pleura at the hilum is incised to expose the pulmonary artery and the superior pulmonary vein, including the middle lobe branch. At this maneuver also the lymph nodes in station 10 are resected, to allow full exposure of the vessels. After division of the inferior pulmonary ligament by electrocautery, including resection of lymph nodes in station 9, the lower pulmonary vein is visualized and encircled by a vessel loop (Fig. 13.2).
We prefer not to divide the vein until the arterial supply of the lower lobe is completely divided, to prevent congestion and parenchymal bleeding from the lung.
During the next step the mediastinal pleura is also incised posterior to the hilum and the lymph nodes in station 8 and 7 are resected. Electrocautery should be used cautiously in this region to prevent damage to the esophageal wall, which lies in close proximity here.
Exposure of the Artery
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


