INDICATIONS
The main indication for a right lower middle lobe sleeve lobectomy is a tumor involving those lobes as well as the bronchus intermedius at or near the takeoff of the right upper lobe bronchus to such an extent that a standard bilobectomy cannot be performed (Fig. 36.1). This sometimes can be determined bronchoscopically, sometimes is only apparent at the time of surgery through direct tumor involvement or a positive frozen section of the proximal bronchus intermedius. Tangential excision, which might compromise the lumen to the upper lobe or the oncologic result, is to be avoided. There may be occasional indications of a benign process such as a bronchopleural fistula or a destroyed bronchus intermedius from infection that are other potential indications.
 PREOPERATIVE PLANNING
PREOPERATIVE PLANNING
A standard workup should include careful history and physical assessment of other comorbid conditions, spirometry, and quantitative ventilation–perfusion scans because of the possibility that a sleeve of the lower middle lobe is not feasible and a pneumonectomy would have to be done. Computerized axial tomography with contrast is essential. This is important to assess vascular involvement as well as extent of tumor. In case of malignant disease, a biopsy is essential and a PET scan warranted in most patients. Magnetic resonance imaging may be helpful in some patients with questionable arterial involvement. Suspicious mediastinal lymph nodes that are identified should be biopsied and may preclude this approach. Tumors of the lower and middle lobe that involve the mediastinal nodes probably precluded this type A sleeve from consideration. It does not make oncologic sense to spare the upper lobe in most cases because of possible nodal involvement of lymph nodes contained within the upper lobe. Bronchoscopy is essential to define the endobronchial limits of the tumor and is best performed by the individual performing the surgery.
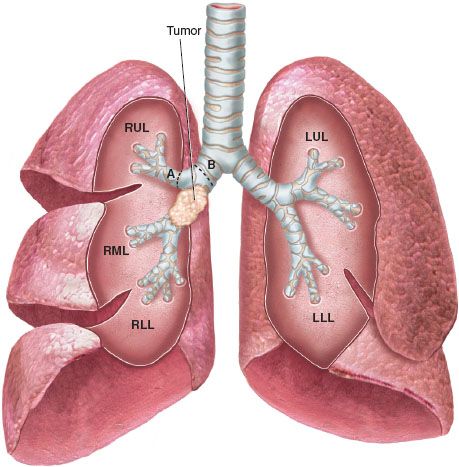
Figure 36.1 Tumor involving bronchus intermedius precluding standard bilobectomy. A,B: Points of transection of bronchus for RU/RMC sleeve.
 SURGERY
SURGERY
This operation is probably best performed in an open fashion; the ability to perform this type of sleeve procedure thoracoscopically would be limited. The need to assess the tumor by palpation and the complexity of the reconstruction would preclude a video-assisted approach in most cases. If the assessment of the mediastinal nodes is negative, the operation should be carried out through a standard posterolateral thoracotomy either as a pure muscle-sparing incision or one which preserves the serratus anterior dividing the latissimus dorsi muscle. The conduct of the operation proceeds along the lines that one would ordinarily do for a bilobectomy. Vascular structures are handled according to surgeon’s preference and dictated by the local findings. After the pulmonary artery and vein to the lower and middle lobe are controlled, the bronchus to the upper lobe is divided at its origin (Fig. 36.2). Frozen sections should be used to be certain of freedom from tumor involvement. The right mainstem bronchus should be divided at its most distal point compatible with clearance of the tumor. Frozen sections should be obtained. By dividing the bronchus in its most distal portion, it will help minimize any size discrepancy that might exist between the right mainstem bronchus and the upper lobe bronchus. The axis of the upper lobe is at 90 degrees to the axis of the right mainstem bronchus. While this is of some theoretical concern, from a practical standpoint, it does not pose a problem. The technique that we have used for all of our bronchoplastic procedures is appropriate for this type of reconstruction. It is important to line up the right upper lobe bronchus with the right mainstem bronchus. Every attempt should be made to line up cartilage-to-cartilage and membranous wall-to-membranous wall. It is much more important, however, to be certain that no torquing or kinking of the bronchus would occur with the ultimate reconstruction of the airway. We utilize traction sutures proximally and distally in the midlateral position of both the proximal and distal airway (Fig. 36.3). This allows assessment of tension and approximation of the ends of the airway on tying the individual anastomotic sutures. We have used 2-0 or 3-0 Vicryl sutures for the traction sutures. These can be adjusted according to the delicacy of the airways or surgeon’s preference. Once the traction sutures have been placed, individual anastomotic sutures are placed, we prefer the knots of the 4-0 Vicryl sutures placed to be on the outside of the airway if at all possible (Figs. 36.3 and 36.4
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


