Fig. 15.1
(a, b) Failure of the Nuss procedure can be due to bar rotation or migration as is seen in these two patient’s lateral chest roentgenogram (a) rotation of a long bar with single stabilizers is seen, (b) Rotation of the lower bar is seen on this patient with 2 support bars and stabilizers
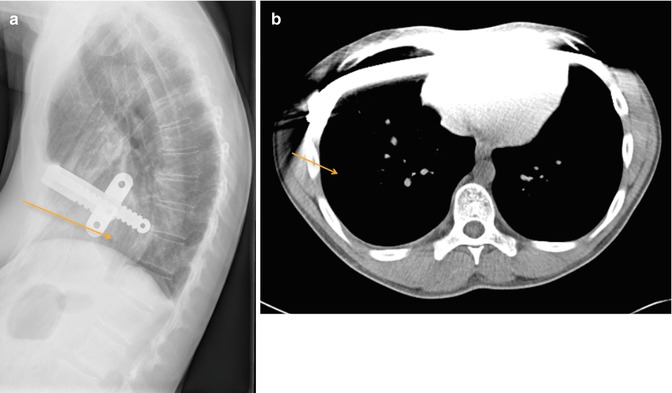
Fig. 15.2
Too lateral entrance of the support bars positions the support bars intrathoracic and fails to elevate the defect anteriorly. (a) posteriorly displaced bar is seen on in this patient’s lateral chest roentgenogram. Arrow point to pectus excavatum defect still seen below the level of the bar. (b) computerized tomography shows intrathoracic portion of support bar with failure to support and elevate the pectus excavatum defect. Arrow points to the space between the chest wall and the bar
Fig. 15.3
Malunion and recurrence of pectus excavatum defect after previous Ravitch repair are seen in these patient’s photographs, computerized tomography and 3-D reconstruction images (a) A 46 year-old female with significant recurrence after open Ravitch procedure. CT scan shows failed union between the rib (thin arrow) and Sternum (thick arrow) (b) A 44 year old male with significant recurrence after open Ravitch procedure. 3D reconstruction shows recurrence and failure of the chest wall to reconstitute
Regardless of which initial procedure was used, some patients will experience recurrence. There are only a few publications devoted exclusively to repair of recurrent pectus deformities, and most studies include children with only a few adults [1–5, 9, 11, 13, 14, 31, 37]. Several of these publications are reviewed in Table 15.1. Most of these reports describe experience with a single operative technique in the repair of recurrent pectus excavatum. The reports by Redlinger and Croitoru et al. advocated a modified Nuss technique for both open and Nuss recurrent PE [13, 14]. Multiple bars were required and they reported slightly higher complication and bar displacement rates with revision versus primary repairs. Others have advocated the use of a modified open Ravitch repair in all patients with recurrent PE, reporting excellent results in a small group of patients, with only a marginally longer length of stay compared to patients undergoing primary repair (6 days versus 5 days) [9]. Studies have shown that repairs in adults may be more difficult and have increased risks of complications due to increased rigidity of the chest wall [3, 7, 10, 18, 30, 31, 38–48]. Complex open repairs were required in many adult patients after prior open repair when compared to other studies [9, 32, 33]. Luu et al., reported on 13 recurrent patients in ages 16–54 years [9]. Eight of these were previous MIRPE and 5 had been a modified Ravitch repair. All of the failed MIRPE procedure patients in this series underwent a modified Ravitch repair for correction, while the recurrent open repair patients required complex reconstructions. Results are reported as good or excellent in many patients undergoing reoperation [5, 9, 11, 31, 49]. Follow up is limited and the long-term durability of repairs unknown. Many publications do not report their length of follow up. Those studies that do provide a longer length of follow up have shown good efficacy in preventing further recurrence of PE during the follow-up periods [2, 5, 11, 31, 49].
Table 15.1
Publications for the surgical treatment of recurrent pectus excavatum
Author | # of patients | Median age at time of reoperation | Primary repair procedure (Nuss, open) | Operative technique secondary repair | Median operative time | Results reported | Length of follow-up (average) |
|---|---|---|---|---|---|---|---|
Croitoru et al. [14] | 50 | 16 years | Nuss 23 Open 27 Multiple 2 | Minimally invasive Modified Nuss | 140 min | 8 % required revision surgery for bar displacement, 85 % report increased exercise tolerance post-op | NR |
Liu et al. [31] | 18 | 21 years | Nuss 1 Open 16 Other 1 | Minimally invasive Modified Nuss | 68.5 min | No bar displacement requiring reoperation, 14/18 (85 %) excellent result, 4/14 (15 %) good result | 19 months |
Miller et al. [11]. | 10 | 15 years | Minimally invasive Modified Nuss | 70 min | Good or excellent results in all patients, no complications | 23 months | |
Redlinger et al. [13]. | 100 | 17 years | Nuss 51 Open 45 Multiple 4 | Minimally invasive Modified Nuss | NR | Bar displacement in 9 patients, 7 of which required reoperation, 2 intraoperative cardiac arrest | NR |
Wang et al. [49]. | 12 | 15 years | Minimally invasive Modified Nuss | 100 min | Bar displacement in 2 patients, no reoperation, excellent result in 66.7 %, good in 25 %, fair 8.3 % | 10–38 months | |
Guo et al. [5]. | 28 | 15 years | Open 28 | Minimally invasive Modified Nuss | 86 min | Excellent results 64 %, Good 25 %, fair 11 % | 24–72 months |
Pison et al [64]. | Minimally invasive Modified Nuss | ||||||
Luu et al. [9] | 13 | 28 years | Nuss 8 Open 5 | Nuss recurrences modified Ravitch Open recurrences required complex reconstruction not described | NR | 1 patient returned to OR 2 years later for resection of protuberant costal cartilage, 10/13 excellent result, 2/13 good result | NR |
Schulz-Drost et al. [34] | 29 years | Open 7 | Open revision with plating | 205 | High patient satisfaction results only | NR |
Surgery for Recurrent Pectus Excavatum
In general, reoperative repair should avoid or repair the issues that contributed to the first surgical approach recurring. Assessment of why a patient’s repair was unsuccessful or recurred is necessary for treating recurrence adequately. Both open and minimally invasive techniques have been described for repair of recurrent PE. Both approaches can offer advantages in the repair of recurrent defects, however, some recurrent defects may require an application of both open and minimally invasive repair techniques to achieve optimal outcomes. Regardless of the approach advocated, reports describing experience with repair of recurrent PE all mention the increased technical difficulties, higher complication rates and longer hospital stays [9, 11, 13, 14].
Recurrent Pectus Excavatum after MIRPE or Nuss Procedure
Recurrences following the Nuss repair are reported at a similar rate as that seen after Ravitch however many aspects of the presentation differ. Technical issues constitute a large proportion of the cases reported as “failed” versus “recurrent” in patients repaired with MIRPE. Some of the more common technical failures and causes reported for recurrent PE after Nuss procedure are listed in Table 15.2.
Table 15.2
Frequent causes of failed or recurrent prior MIRPE or Nuss procedure
Rotation or displacement of bars |
Bars too long |
Bars placed too lateral |
Intercostal Stripping |
Disproportionate weight distribution of chest wall on number of bars |
Failure of bars to remain secured to chest wall |
Failure to lift with bar placement |
Chest wall too stiff and non-compliant |
Adequate number of bars not utilized for weight & compliance of chest wall |
Adequate number of bars not utilized for length and depth of defect |
Bars stripped lateral failing to support chest anteriorly |
Premature removal of bars |
Connective tissue disorders |
The majority of experienced centers reporting on revision of prior failed or recurrent MIRPE patients found that malpositioned or displaced bars were a large portion of the issue [2, 5, 13, 14, 31] (Fig. 15.4a–c). Bar displacement is the most common complication following Nuss repair, with displacement rates greater than 10 % in some studies [6–8, 12, 19, 23, 25–27, 42, 43, 50–54]. Adult patients have also been noted to have a greater incidence of bar rotation and complications [4, 5]. This can lead to recurrence of the pectus deformity as well as need for subsequent reoperation. There are a variety of different issues that can lead to bar rotation and migration. The majority of revisions reported on noted bars that were too long (Fig. 15.5) [13, 14]. These bars were replaced with bars that were 1–4 in. shorter on average. Bars that were placed too lateral or intercostal stripping and lateral displacement occurring after placement was another common technical issue noted (Fig. 15.6a, b). When lateral displacement occurs, the bar will fail to contact the sternum and support it anteriorly (Fig. 15.7). The entry and exit sites into the chest should not be too lateral or muscle stripping can occur [13, 14, 20, 26, 53]. Use of a different interspace was recommended should intercostal stripping and lateral displacement occur [13]. Figure of eight suture reinforcement of the ribs bordering the stripped intercostal space can also be performed. The utilization of forced sternal elevation may also help facilitate bar placement and rotation and minimize intercostal stripping [55].
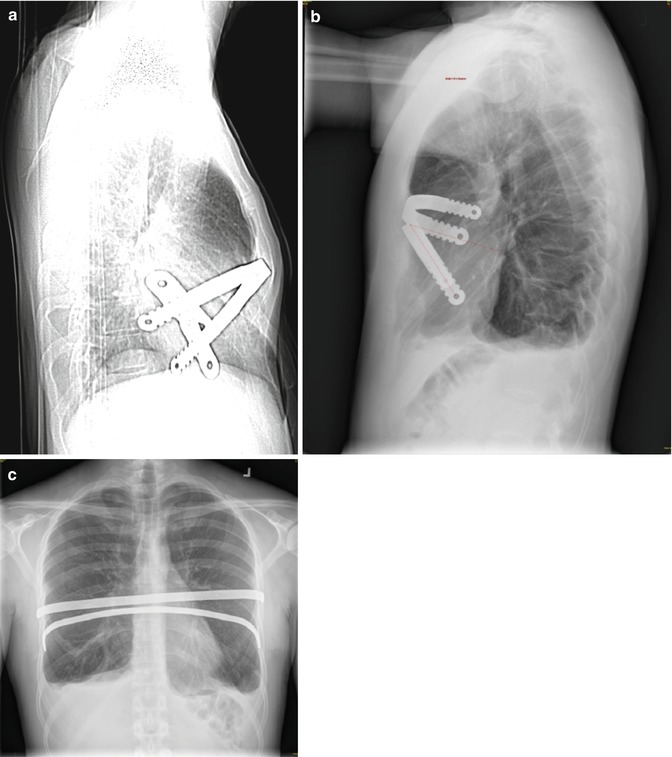
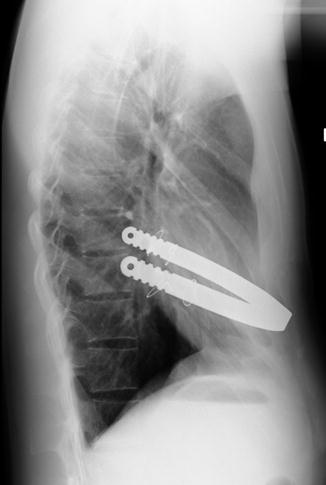
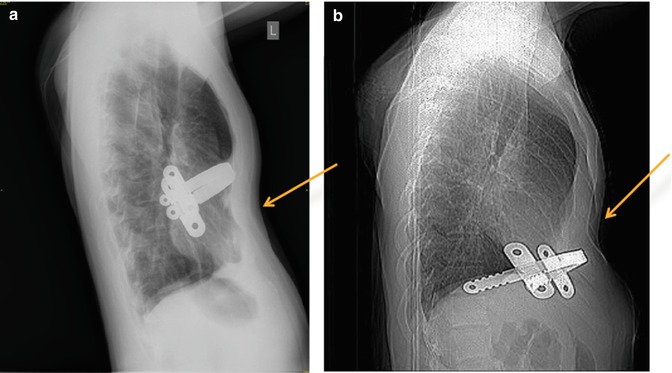
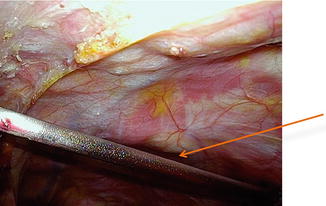
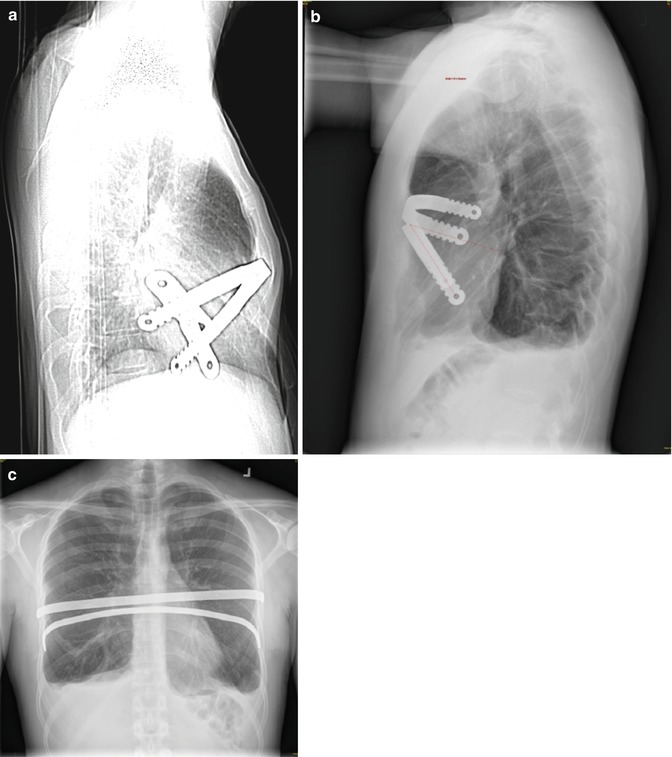
Fig. 15.4
(a–c) Lateral chest and A/P roentgenograms show bar rotation and migration in three patients after Nuss pectus excavatum repair
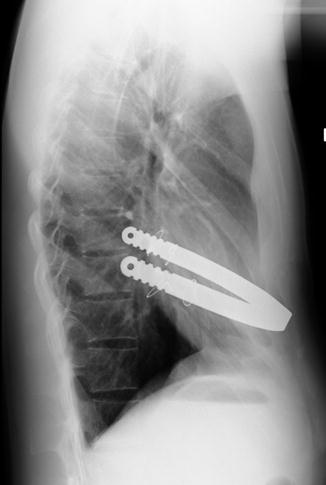
Fig. 15.5
Lateral roentgenogram of patient with recurrent pectus defect less than 1 month after Nuss repair and placement of single bar. Note a longer than recommended length of bar and curvature beyond the mid-axillary line with rotation and displacement
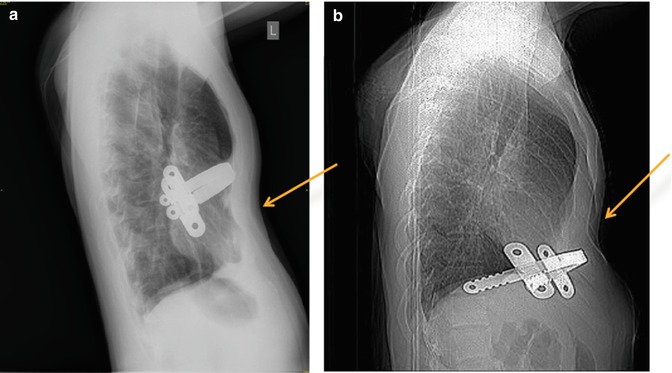
Fig. 15.6
(a, b) Lateral chest roentgenograms showing single pectus bar with failed elevation of the pectus excavatum defect secondary to lateral displacement (a) and intrathoracic migration (b). Arrows note pectus excavatum deformity still present despite support bar indwelling
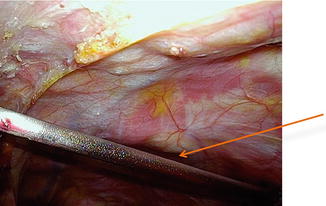
Fig. 15.7
Thoracoscopic view of intrathoracic pectus support bar which fails to contact the anterior chest wall due to lateral intercostal placement. Arrow notes space between chest wall and support bar
Adequate stability is also impacted by the number of bars and balance of the chest wall on support structures. For heavier, stiffer chests, several bars may be necessary to support the weight and elevate the defect. The pressure required to elevate the chest is significant and an inadequate number of bars to support the chest anterior can lead to lateral stripping of the intercostals and increased risk of bar rotation [22, 27, 55–58]. Recommendations as to what the adequate number of bars are varies [6, 18, 20, 25, 53, 59]. Initial reports of the Nuss procedure encompassed young patients with only one bar advocated however the majority recommend increased number of bars with more significant defects and advanced ages [53]. Older patients have also been reported by others to require more bars for PE repair and two or more bars may give better and more stable results [18, 25, 58, 60, 61]. For some patients presenting with reported recurrence, there may have been an incomplete repair of their defect following the initial Nuss with a portion of their defect remaining postsurgical due to an inadequate number of support bars (Fig. 15.8a–c) [3].
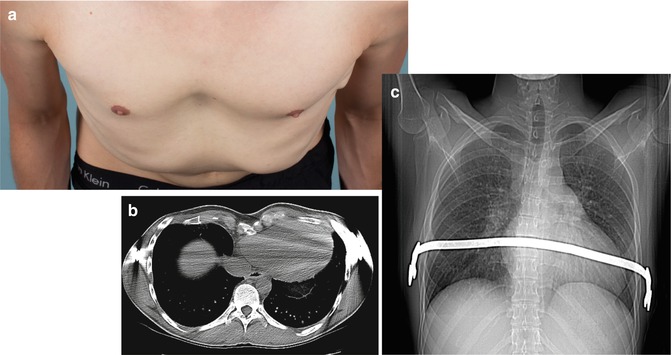
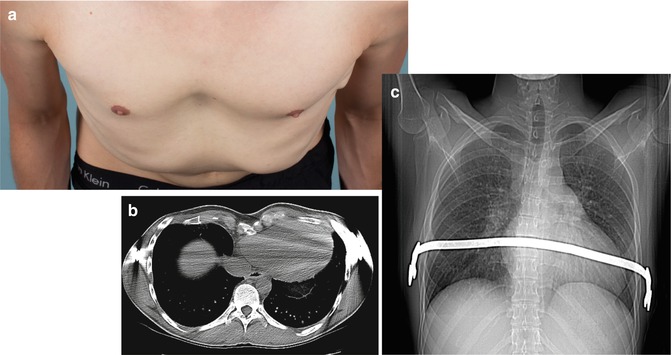
Fig. 15.8
(a–c) Photographs (a) and radiographic imaging (b, c) are shown of a 26 year-old male with pectus excavatum deformity 2 years after placement of single support bar with residual defect of Haller Index 4.6 and chronic postoperative pain. The single bar fails to elevate and support the defect inferiorly
Recurrence has also been attributed to premature removal of the pectus bars before adequate remodeling has occurred and the chest wall secured into a corrected position. The optimal length of time recommended to leave support bars in place varies however, several experienced centers have increased their recommended time to 2–3 years [6, 7, 25, 40, 57, 62]. Patients with Marfan’s and other connective tissue disorders have been shown to have a higher risk for recurrence and recommendations are for leaving the bars in place for up to 4 years [1, 4, 29].
A significant problem encountered after a failed Nuss can be extensive intrathoracic adhesions [5]. These can require several hours of extensive adhesiolysis before dissection across the chest and mediastinum is achieved for bar placement. Use of sternal elevation may be helpful and others have described a subxiphoid incision to manually elevate the sternum during dissection across the chest, especially with extensive adhesions [5, 9, 13, 14, 63, 64].
Recurrent Pectus Excavatum after Ravitch and Open Procedures
The original open procedure for PE repair was described and accredited to Ravitch in the 1940s [65, 66]. Modifications of this technique have been used successfully for several decades [2, 15, 42, 67–69]. The open repair involves resection of the deformed costal cartilage with or without sternal osteotomy. Recurrence risks are based on multiple factors as listed in Table 15.3. Once recurrence occurs, subsequent repair becomes more complex. The challenges encountered with re-operative repair can vary based on the extent of initial operative repair. There is limited literature published on repair of recurrent open PE, however, most reported higher complication rates, longer hospital stays, and higher rates of bar displacement when repaired with MIRPE [5, 13, 14].
Table 15.3
Frequent causes of failed or recurrent prior Ravitch/open procedures
Incomplete previous repair |
Repair at too young of age |
Dissection either too extensive or too little |
Early removal or lack of support structures |
Incomplete healing of the chest wall with pseudoarthrosis, “sternal floating and osteonecrosis” |
Connective tissue disorders |
Infection and seroma complications |
Surgical repair of patients having undergone a previous Ravitch or other open PE repair technique may have unique problems when recurrence occurs. Repair can be quite challenging due to rigidity of the bony chest wall and scar tissue from the prior surgical intervention. Extensive calcification, ossification and fusion of the previously excised cartilage may prevent adequate elevation of the chest wall without reexcision [9, 32, 33, 35, 70]. Osteotomies of the sternum, sterno-costal junctions and more laterally along the ribs may be necessary to mobilize the anterior chest wall. Recurrences following open PE repair can also arise from osteonecrosis, malunion due to pseudomembranous attachments, instability and/or chest wall hernia (Fig. 15.9a, b) [1, 3, 4, 9, 17, 31, 33]. When non-union occurs bilaterally, this can also lead to an entity known as “floating sternum”, which requires revision to reattach and stabilize the sternum (Fig. 15.10) [34, 36, 71].
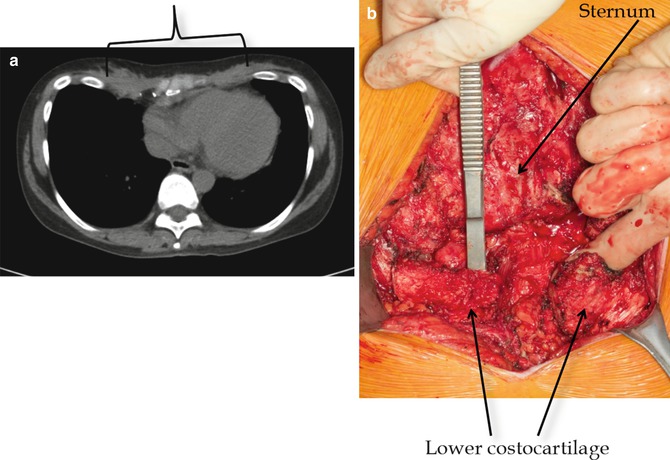
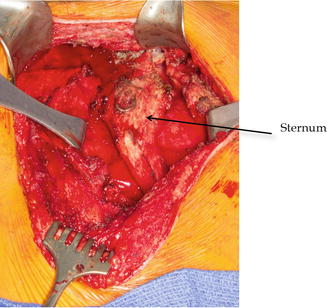
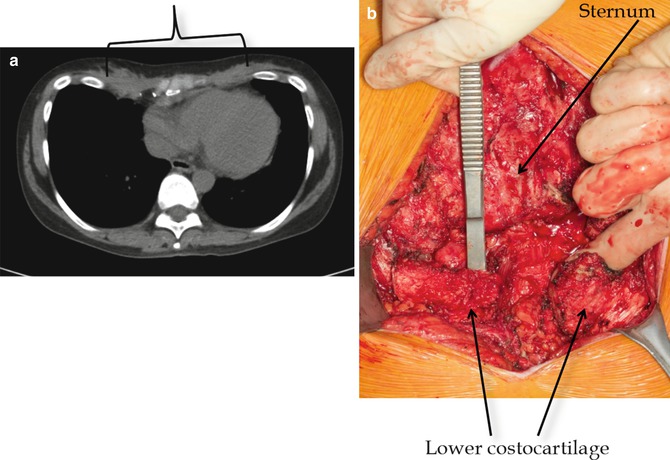
Fig. 15.9
(a, b) Computerized tomography (a) of the chest and intraoperative photograph (b) showing fibrous malunion and recurrence due to improper healing after prior Ravitch pectus repair. The instrument is place under the lower cartilage attachments which are completely separate from the sternum. Arrows
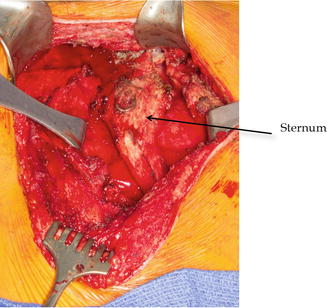
Fig. 15.10
Intraoperative photograph showing “sternal floating” after prior open Ravitch pectus repair with bilateral non-union of costocartilages and sternum
Successful repair of areas of malunion, pseudo-arthrosis and sternal floating requires repeat open repair. Open repair and stabilization has also been recommended by other authors for these complicated recurrences [3, 9]. Rib/sternal reattachment and sites of repeated osteotomies prone to malunion or non-union can be approximated with titanium plating or FiberwireTM (Arthrex, Inc, Naples, FL).
Rigidity of the chest wall following Ravitch is the main component that must be overcome to achieve an adequate repair. MIRPE is more difficult as a result, and bar displacement more likely. Additionally, a study by Redlinger et. al. also mentions findings of significant intrathoracic adhesions following Ravitch repair, despite this being considered an extra-pleural repair, making placement of pectus bars difficult [13]. The use of forced sternal elevation to move the sternum anterior has been reported to be helpful for safe dissection and repair with MIRPE [55, 57, 72–74].
Despite these challenges, MIRPE following previous open repair can be quite successful [5, 11, 14, 31]. Redlinger et al. reported on 100 patients they successfully repaired with the Nuss procedure after recurrences (45 prior open and 51 prior Nuss) [13]. Repair of patients with previous Ravitch procedures required multiple bars. Opening the previous Ravitch incision for manual lifting of the sternum during the dissection under the pectus defect was felt to significantly improve the safety of the dissection and success of the procedure [13].
Rarely following Ravitch repair at too young and age, patients can have impairment of the normal chest wall growth, or acquired asphyxiating thoracic dystrophy, which was first described by Haller in 1996 [35]. Haller speculated that this “acquired Jeune’s syndrome” was related to disruption of the normal growth centers of the affected ribs. These patients typically had repair of their defect at a very young age (<4 years), which had been common in the 1970s and 1980s. This is a complicated disorder with high risks for reconstruction to improve the chest defects presents. These patients required complex reconstructions of which discussion is beyond the context of this report and limited reports are published [21, 32, 35].
Indications for Surgical Revision Repair
Indications for repair of recurrent pectus excavatum are similar to those for primary repair and reviewed in Table 15.4 [1, 3–5, 9, 11, 14, 37, 64, 75–82]. Those patients with a recurrent, significant defect and those with symptomatology correlating with the return of their defect, including dyspnea, palpitations, and inability to keep up with their peers, all factor into the decision to repair a recurrent defect. Additionally, patients that have undergone previous open repair may have areas of non-union, chest wall hernias and other conditions that lead to chronic pain and chest wall instability [3, 33–35, 37, 71, 76]. Resultant symptoms from this type of defect can be severe and may be an indication for surgery despite not meeting criteria based on the measurements of their defect. Reoperation should be individualized to the patient with great consideration given to the increased operative complexity and risk of complications. Extensive patient education about the surgical complications, recovery period, and final results are necessary to create realistic expectations for the patient.
Table 15.4




Indications for surgical revision of prior failed pectus excavatum
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


