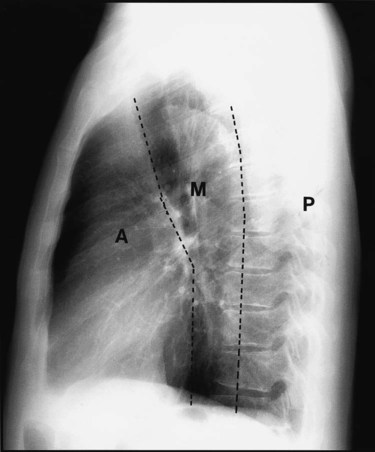
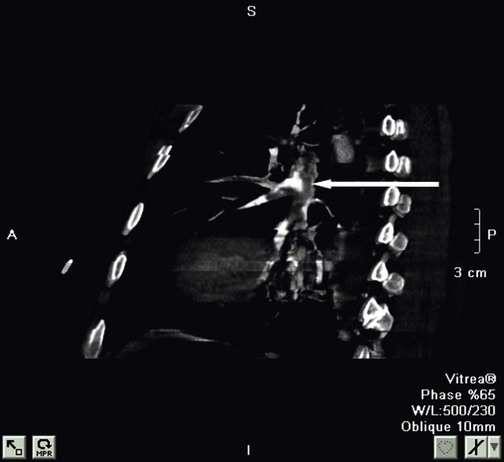
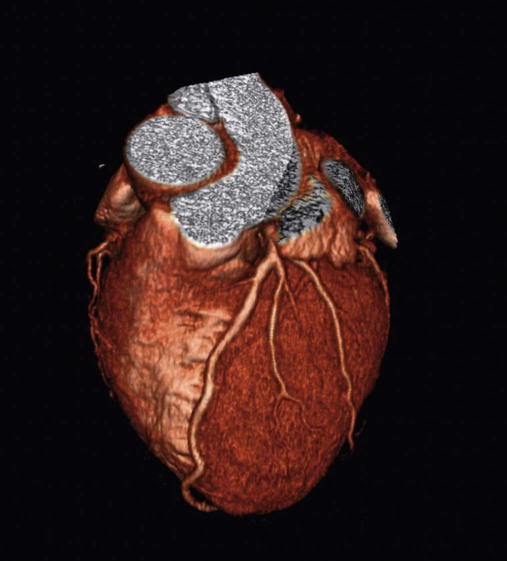
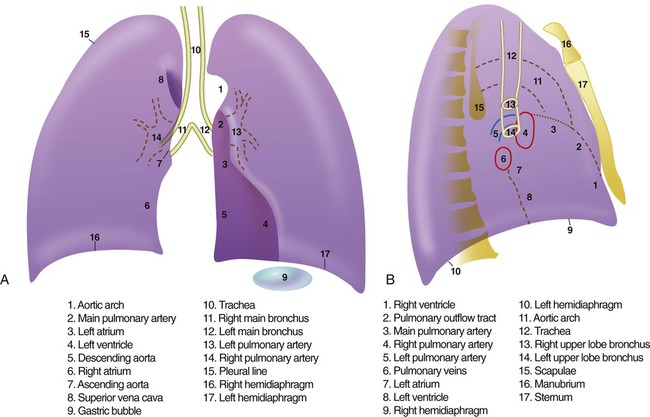
After reading this chapter you will be able to: When to obtain a chest radiograph is ultimately the decision of the attending physician. However, the RT may be able to suggest that a chest x-ray should be obtained in certain circumstances, such as when a patient in the intensive care unit suddenly deteriorates for no apparent reason. The RT needs to be familiar with the common clinical indications for obtaining a chest radiograph (Box 20-1). In broad terms, the steps in reviewing a chest film are as follows: • Identify the name on the radiograph. • Review the technique and quality of the film: Is the film well centered (i.e., the spinous processes are right in the middle of the trachea on a posteroanterior [PA] film), and is the amount of penetration of the beam adequate, too high (i.e., the lung parenchyma is too dark to see subtle changes), or too low (i.e., the lung parenchyma is too white, causing normal lung markings to appear abnormal)? • Systematically review the anatomic structures on the chest film to assess their normality or abnormality. Several technical factors should be routinely assessed when reading a chest film: 1. Is the film appropriately labeled? 2. Is the film PA with a lateral view, or is it an anteroposterior (AP) portable film? 3. Is the entire chest imaged on the film (i.e., are any structures cut off from the film)? 4. Was the patient properly positioned for the film? 5. Were the optimal settings for the x-ray beam selected when the film was taken (the term used is penetration, which is similar to exposure on camera film)? Patient rotation can make interpretation more difficult by projecting midline structures (e.g., the trachea) to the right or left. The observer can assess for rotation by comparing anterior structures such as the medial (toward the middle) ends of the clavicles with a posterior structure such as the spinous process (midline structure of the spine). In a perfectly positioned or aligned chest film, the spinous process should be seen midway between the medial ends of the clavicles and in the middle of the tracheal air column (Figure 20-1). Patient rotation makes the mediastinum appear unusually wide and obscures or distorts the appearance of the pulmonary arteries as they emerge from the mediastinum into the lung parenchyma. After the RT has reviewed the technical aspects of the chest radiograph, it is time to review the anatomic findings in the film. The main structures imaged on a routine chest radiograph are listed next and illustrated in Figure 20-2: 1. Bones (e.g., ribs, clavicles, scapulae, vertebrae) 2. Soft tissues (e.g., tissues of the chest wall, upper abdomen, lymph nodes) 3. Lungs (including the trachea, bronchi, and lung tissue or parenchyma) 4. Pleura (membranous coverings of the lung, including the visceral pleura [the part attached to the lungs] and the parietal pleura [the part lining the inside of the chest wall]; although normally occupied by only a small amount of fluid, the space between the parietal and visceral pleura is called the pleural space) 5. Heart, great vessels, and mediastinum (i.e., the tissues between the two lungs in the center of the chest, bordered by the sternum and the vertebral column in the AP dimension and by the thoracic inlet [where the trachea enters the thorax] and the diaphragm in the cephalocaudal direction) Review of the lung edge on both frontal and lateral films discloses any pleural abnormalities, such as fluid in the pleural space (e.g., hydrothorax, hemothorax [blood in the pleural space]) and air in the pleural space (pneumothorax). Evaluation of the mediastinum should include assessment of heart size. In the PA projection, the diameter of the heart shadow should not exceed one-half the diameter of the chest. An enlarged heart may occur with congestive heart failure or with a large pericardial effusion (accumulation of fluid within the space that surrounds the heart encased within the pericardium). The lateral contours of the mediastinum should correspond to normal anatomic structures as outlined in Figure 20-3. The rapid scanning that can be performed on helical CT scanners has made CT angiography possible. To perform CT angiography, a large amount of contrast dye is injected into the patient’s vein. The CT technician monitors the movement of contrast material so the scan can be started when the contrast material has entered the area to be studied. CT angiography of the chest has been used for years to identify pulmonary thromboemboli (Figure 20-4).1 More recently, CT angiography of the coronary artery has been evaluated; this seems to provide an alternative to routine coronary angiography in many patients. The imaging processing capabilities of modern CT scanners allow reconstruction of the chest in any direction and production of three-dimensional representations of some areas of the body (Figure 20-5). The term virtual bronchoscopy is used when these reconstructions simulate the view of the airways that a physician would have during bronchoscopy.
Review of Thoracic Imaging
 List the four tissue densities seen on a chest radiograph.
List the four tissue densities seen on a chest radiograph.
 Define the terms radiolucent and radiopaque.
Define the terms radiolucent and radiopaque.
 Describe how to evaluate the technical quality of a chest radiograph.
Describe how to evaluate the technical quality of a chest radiograph.
 State the differences between a posteroanterior chest film and an anteroposterior chest film.
State the differences between a posteroanterior chest film and an anteroposterior chest film.
 List the anatomic structures seen on a chest radiograph.
List the anatomic structures seen on a chest radiograph.
 List the steps used to interpret thoracic imaging studies.
List the steps used to interpret thoracic imaging studies.
 Identify the value of a computed tomography (CT) scan, high-resolution CT scan, and CT angiogram.
Identify the value of a computed tomography (CT) scan, high-resolution CT scan, and CT angiogram.
 Describe the common radiographic abnormalities seen in the pleura, lung parenchyma, and mediastinum.
Describe the common radiographic abnormalities seen in the pleura, lung parenchyma, and mediastinum.
Overview of Plain Chest Radiograph
Approach to Reading a Plain Chest Radiograph
Chest Radiograph Technique and Quality
Anatomic Structures Seen on a Chest Radiograph
Advanced Chest Imaging Techniques
Computed Tomography of the Chest
Computed Tomography Angiography
Three-Dimensional Reconstruction
Review of Thoracic Imaging

 ) scans, which have been historically used in the diagnosis of pulmonary embolism. Radioisotope
) scans, which have been historically used in the diagnosis of pulmonary embolism. Radioisotope