Retrocardiac Mass
Toms Franquet, MD, PhD
DIFFERENTIAL DIAGNOSIS
Common
Hiatal Hernia
Descending Aortic Aneurysm
Tortuosity (Aging) of Aorta
Mediastinal Lymphadenopathy
Postoperative State, Esophagus
Less Common
Pulsion Esophageal Diverticulum
Periesophageal Omental Hernia
Achalasia
Esophageal Perforation
Paraesophageal Varices
Benign Esophageal Tumors
Esophageal Malignant Neoplasms
Carcinoma
Primary Esophageal Lymphoma
Cystic Masses
Bronchogenic Cyst
Esophageal Duplication Cyst
Rare but Important
Mediastinal Pancreatic Pseudocyst
ESSENTIAL INFORMATION
Key Differential Diagnosis Issues
Retrocardiac mass with air-fluid level is characteristic of esophageal hiatal hernia
Esophageal disorders may present radiographically as retrocardiac masses
Should always consider vascular aneurysm
Aortic aneurysm may result in anterior, middle, or posterior mediastinum
Mediastinal mass with curvilinear calcification
Helpful Clues for Common Diagnoses
Hiatal Hernia
Sliding hiatal hernia: Most common type
May be large containing stomach and portions of colon
Chest radiograph: Characteristic retrocardiac mass with or without air-fluid level
Widening of esophageal hiatus
Descending Aortic Aneurysm
Focal or diffuse left paramediastinal or posterior mediastinal mass
Calcification in aneurysm wall (75%)
CECT: Allows accurate assessment of complications
MR: Similar to CT in diagnosis of aortic aneurysms
Tortuosity (Aging) of Aorta
Increased prevalence in elderly population
Mediastinal Lymphadenopathy
Common causes: Lymphoma, lymphocytic leukemia, metastases, and granulomatous infections
Giant lymph node hyperplasia (Castleman disease): Marked enhancement of single enlarged mediastinal lymph node group
Postoperative State, Esophagus
Esophagectomy with gastric pull-up procedure
Gastric conduit is usually placed in paravertebral space of posterior mediastinum
Postsurgical complications
Postsurgical diaphragmatic hernia (omental fat ± colon)
Redundant conduit (excess length of gastric tube)
Mediastinitis due to anastomotic leak
Helpful Clues for Less Common Diagnoses
Pulsion Esophageal Diverticulum
Large sac-like protrusion in epiphrenic region
Retrocardiac soft tissue mass often containing air-fluid level
Periesophageal Omental Hernia
Omentum herniates through phrenicoesophageal ligament
Mimics lipomatous mediastinal tumor or esophageal lipoma
Achalasia
Double contour of mediastinal borders: Outer borders of dilated esophagus project beyond shadows of aorta and heart
Dilatation of esophagus
Retained fluid, food debris, and air-fluid level
Aspiration pneumonia common
Esophageal Perforation
Iatrogenic: Endoscopic procedures (80%-90%), trauma: Blunt trauma, foreign bodies: Impacted bones, spontaneous: Boerhaave syndrome, and neoplasms
Paraesophageal Varices
Right- or left-sided mediastinal soft tissue masses near diaphragm
Change in size and shape with peristalsis, respiration, and Valsalva maneuvers
CECT: Serpiginous contrast-enhanced structures
T1WI and T2WI MR: Multiple areas of flow void
Benign Esophageal Tumors
Leiomyoma
Most frequent benign tumor of esophagus (distal esophagus)
Size: 2 cm to > 10 cm
Round/ovoid filling defect, outlined by barium
Amorphous or punctate calcifications
Esophageal GIST (GI stromal cell tumors)
Large mass
May ulcerate with gas and contrast medium entering cavity
Esophageal Malignant Neoplasms
Carcinoma
Obscuration of periesophageal fat planes
Lobulated and irregular margins
Periesophageal and upper abdominal lymphadenopathy
Primary Esophageal Lymphoma
Less than 1% of all malignant esophageal neoplasms
Polypoid, ulcerated, and infiltrative
Cystic Masses
Bronchogenic Cyst
Round, oval masses usually in right paratracheal or subcarinal region
CECT: Homogeneous water density mass with thin smooth wall (50%); indistinguishable from soft tissue lesions (50%)
MR: Homogeneous low signal intensity on T1WI and high signal intensity on T2WI
Esophageal Duplication Cyst
Majority occur in infants or children
Adjacent to or within esophageal wall
Ectopic gastric mucosa within cyst: May cause hemorrhage or perforation
CT or MR: Homogeneous water density mass in intimate contact with esophagus
Helpful Clues for Rare Diagnoses
Mediastinal Pancreatic Pseudocyst
Location: 1/3 juxta- or intrasplenic, retroperitoneum, and mediastinum
Develops over a short time in patients with evidence of pancreatitis
NECT: Low-attenuation spherical or oblong mass in posterior mediastinum or adjacent thoracic cavity
CECT: Enhancement of thin fibrous capsule
Image Gallery
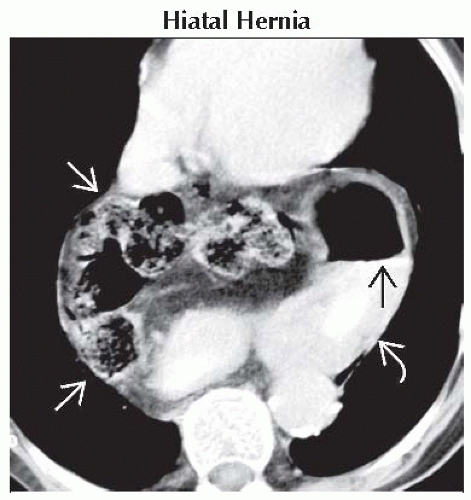 Axial CECT shows a large retrocardiac hiatal hernia containing the stomach
 and portions of the colon and portions of the colon  . Note a visible air-fluid level within the stomach . Note a visible air-fluid level within the stomach  . .Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|