Reticular Pattern
Eric J. Stern, MD
DIFFERENTIAL DIAGNOSIS
Common
Idiopathic Pulmonary Fibrosis (IPF)
Pulmonary Edema
Nonspecific Interstitial Pneumonitis (NSIP)
Connective Tissue Diseases
Scleroderma
Rheumatoid Arthritis
Sarcoidosis
Asbestosis
Less Common
Chronic Hypersensitivity Pneumonitis
Drug-Induced Lung Disease
Polymyositis/Dermatomyositis
Lymphangitic Carcinomatosis
Rare but Important
Diffuse Pulmonary Lymphangiomatosis
ESSENTIAL INFORMATION
Key Differential Diagnosis Issues
Reticular pattern
Pattern produced by innumerable interlacing small linear opacities
Resembles fisherman’s net; mesh-like
Fine, medium, or coarse reticulation may reflect disease progression
Connotation for pattern on chest radiographs similar; however, summation of cystic spaces may result in reticular pattern
HRCT specific components
Small, irregular linear opacities
Irregular interlobular septal thickening
Irregular intralobular linear opacities; interstitial thickening within secondary pulmonary lobule, usually fibrosis
Architectural distortion, traction bronchiectasis, and bronchiolectasis, due to fibrosis
Helpful Clues for Common Diagnoses
Idiopathic Pulmonary Fibrosis (IPF)
Common interstitial lung disease of unknown etiology
Pathologically has usual interstitial pneumonia (UIP) pattern
Bilateral, symmetric, patchy reticular pattern; may involve all lobes but most severe in subpleural lung and lung bases
Traction bronchiectasis and bronchiolectasis; architectural distortion; irregular interfaces with pleural, vascular, and bronchial structures
Subpleural honeycombing often present (air-containing cysts measuring 2-25 mm)
Pulmonary Edema
Smooth thickening of interlobular septa and bronchovascular bundles; gravity-dependent ground-glass opacities &/or consolidation
Associated cardiomegaly, pleural effusions
Rapidly evolves; may resolve quickly with diuretics
Nonspecific Interstitial Pneumonitis (NSIP)
Most commonly in patients with connective tissue disease (scleroderma, rheumatoid arthritis) and drug-related lung disease
Histologic pattern of interstitial fibrosis and inflammation
Extent of ground-glass opacities > reticular opacities
Traction bronchiectasis usually out of proportion to severity of reticular opacities
Honeycombing uncommon
Distribution: Lower lung zones (60-90%), peripheral lung (50-70%); may be diffuse
Sparing of immediate subpleural lung in dorsal aspect of lower lobes (50%)
Scleroderma
Pattern typically NSIP; UIP pattern less common
Dilated esophagus common
Consolidation may occur due to
Pneumonia, aspiration, organizing pneumonia, diffuse alveolar damage, diffuse pulmonary hemorrhage
Rheumatoid Arthritis
Findings of NSIP (ground-glass opacities, fine reticulation), UIP pattern less common
Osseous erosions may be evident in humeral heads or sternoclavicular joints
Sarcoidosis
Reticular pattern more common with end-stage fibrotic disease (stage IV)
Extensive reticulation, mainly involving perihilar regions of upper and middle lung zones; cystic changes may occur
Architectural distortion, traction bronchiectasis, superior hilar retraction, compensatory overinflation of lower lobes
Small perilymphatic nodules may be present in less involved lung
Hilar and mediastinal adenopathy, common in early sarcoidosis; usually has resolved with extensive fibrosis
Asbestosis
Irregular thickening of inter- and intralobular septa, subpleural curvilinear opacities, parenchymal bands
Predominantly involves peripheral and dorsal aspects of lower lung zones
Frequently associated pleural plaques (90%)
Occupational exposure important
Helpful Clues for Less Common Diagnoses
Chronic Hypersensitivity Pneumonitis
Mid-lung predominance most common, especially in those with low-level continuous antigen exposure (bird breeders)
Upper lung zone predominance more common in those with intermittent exposure (farmers)
Fibrosis: Irregular linear opacities (40%), traction bronchiectasis (20%)
Often superimposed subacute findings
Poorly defined centrilobular opacities, ground-glass opacities, lobular areas of air-trapping
Drug-Induced Lung Disease
Produces wide array of injury patterns, including reticular pattern
Reticular pattern may be due to UIP, NSIP, or pulmonary edema
Polymyositis/Dermatomyositis
Symmetric basal reticular opacities, architectural distortion, irregular bronchovascular thickening; may progress to honeycombing
Early stages: Ground-glass opacities; bilateral, symmetric basal distribution
Lymphangitic Carcinomatosis
Smooth &/or nodular thickening of interlobular septa, bronchovascular bundles, interlobar fissures, and subpleural interstitium
Distribution: Often spares lobe or whole lung
May have pleural effusions and mediastinal adenopathy
Usually known history of previous malignancy
Helpful Clues for Rare Diagnoses
Diffuse Pulmonary Lymphangiomatosis
a.k.a. lymphangiectasis
Smooth, uniform thickening of interlobular septa and fissures
Marked, smooth thickening of bronchovascular bundles
Diffuse effacement of mediastinal fat and enlarged mediastinal lymph nodes key to recognition
Image Gallery
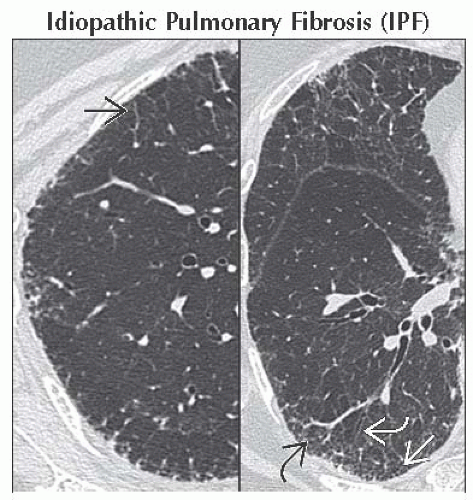 Axial HRCT of a patient with early IPF shows irregular thickened interlobular septa
 , intralobular reticulation , intralobular reticulation  , traction bronchiectasis , traction bronchiectasis  , and fine honeycombing , and fine honeycombing  . .Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|