Percutaneous treatment of subclavian artery stenosis or occlusion has become more popular compared with surgical correction. We compared the early and late results of subclavian artery stenting with bilateral or single transradial access. From 2010 to 2015, we recruited 54 consecutive patients. In 35 cases, we used bilateral access, and in 19 cases, ipsilateral single access was used. Left subclavian artery was the culprit vessel in 72% of cases. There were more chronic total occlusions in the bilateral group (77% vs 21%, p = 0.0001). Transradial-only approach was used in all cases, except in 2 cases in the bilateral group where crossover to femoral access was required. Stents were implanted in 94% in bilateral group and 84% in single group (p = 0.47). Procedure duration (40 [35 to 60] vs 20 [15 to 30] minutes), contrast volume (200 [200 to 350] vs 150 [100 to 200] ml and fluoroscopy time (20 [12 to 30] vs 8 [4 to 11] minutes) were higher in bilateral group (all p values <0.0001). Procedural success was 96%. Overall, we observed three <5-cm hematomas and 3 asymptomatic radial artery occlusions at hospital discharge. After successful procedure, blood pressure equalized in 94% in bilateral group and 100% in single group (p = 0.54). Major cardiovascular and cerebrovascular event-free survival up to 5 years was 97% in bilateral group compared with 84% in single group (p = 0.12). Subclavian artery patency at late follow-up was 91% in bilateral group and 95% in single group (p = 1.00). Using single or bilateral transradial approach, subclavian artery lesions or occlusions can be effectively and safely treated without the risks of femoral or brachial access.
The transradial approach (TRA) for percutaneous coronary intervention is increasingly used due to its major advantages over transfemoral approach. Yet, radial or ulnar access for peripheral interventions has not yet become popular. Subclavian artery stenosis or chronic total occlusion (CTO) in patients with cardiovascular disease can be found in 2.5% to 7.5% of cases. Although many lesions remain asymptomatic, variable symptoms from arm fatigue due to arm ischemia to vertebrobasilar insufficiency and coronary steal syndrome in postcoronary artery bypass graft surgery patients have been described. Although surgery has provided good long-term patency, endovascular techniques have been developed and provide less-invasive alternatives. As previously reported, our routine practice for the treatment of upper limbs complex lesions involves the use of single ispilateral or bilateral radial access if better angiographic guidance is required. In this observational study, we compared angiographic, duplex ultrasonography and early and late clinical results of subclavian artery percutaneous interventions using single or bilateral transradial access to guide vessel recanalization and stent implantation.
Methods
Patients treated for subclavian artery stenosis or occlusion were identified from our clinical database. Clinical follow-up was performed regularly up to 5 years after the index procedure. The study was conducted in accordance with our local institutional review board regulations, and a written informed consent was obtained from all patients prior to procedure.
For single ipsilateral access, the distal radial or ulnar artery is cannulated as previously described. Briefly, with the patient’s wrist slightly hyperextended on a dedicated arm board, the right and left radial or ulnar artery is cannulated and 11 cm 6Fr hydrophilic sheaths (Terumo Medical Corporation, Tokyo, Japan) are inserted. After sheath insertion, distal forearm angiography is performed, and 5-mg verapamil is routinely administered through the sheath as spasmolytic agent. For bilateral access, both arms are prepared and a 5Fr hydrophilic sheath (Terumo Medical Corporation, Tokyo, Japan) is inserted in the contralateral artery. No ultrasound guidance was performed to achieve successful access site.
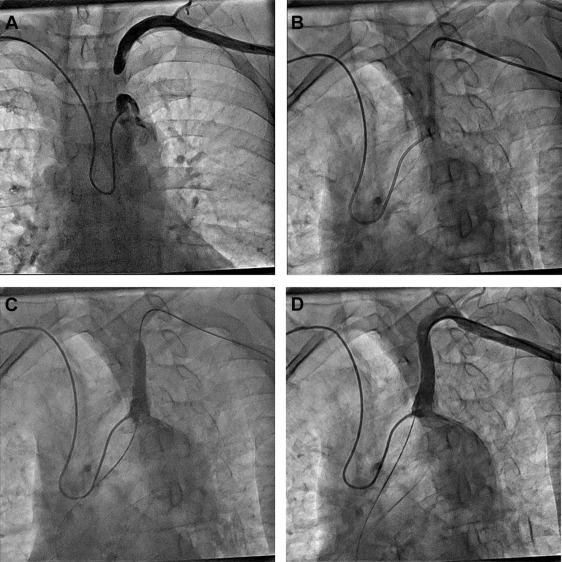
From the ipsilateral arm, we used JR 4.0 6Fr guiding catheter (Launcher; Medtronic, Minneapolis, Minnesota), and from the contralateral arm, Simmons 2 5Fr diagnostic catheter (Merit Medical, South Jordan, Utah) was used for controlled injections. The occlusion and collaterals were assessed with simultaneous bilateral injections ( Figure 1 ). Contralateral injection was used to confirm proper wire advancement within the lesion. The CTOs were crossed with coronary 0.014″ CTO wires and predilatations were made with regular 0.014″ balloon catheters ( Figure 1 ). Afterward, CTOs were recrossed with the 6Fr guiding catheter and exchanged with heavily supportive 0.035″ Amplatz 260-mm guidewire (Boston Scientific, Marlborough, Massachusetts). Ballon-expandable stents were advanced solely through guidewire without guiding catheter ( Figure 1 ). Proper stent positioning was reconfirmed with contralateral injections through the Simmons 2 catheter ( Figure 1 ).
As per our routine, all patients were preloaded with dual antiplatelet therapy (aspirin and clopidogrel 300 mg) before the procedure. After successful vascular access, a bolus of 5,000 IU of unfractionated heparin was administered intravenously.
At the end of the procedure, all catheters were removed, and hemostasis was obtained by application of TR-band (Terumo Medical Corporation, Tokyo, Japan). Per protocol, the bracelet was loosened every 15 minutes until hemostasis was achieved usually within 2 hours as previously described.
Categorical variables are expressed as numbers and percentages and continuous variables as the mean ± SD, or median (interquartile range). All calculations and statistical analysis were performed using JMP 11.0 software (SAS Institute, Cary, North Carolina).
Results
From February 2010 to February 2015, we treated 54 patients for subclavian artery stenosis or CTO. In 35 cases, we used bilateral access (bilateral group) and in 19 cases ipsilateral single (single group) access ( Table 1 ). Mean age of patients was 65 ± 9 years with 59% of men. Cardiovascular risk factors were evenly distributed in the 2 groups with 33% of patients with diabetes and 59% of current smokers. Nineteen percent of patients had experienced previous stroke with 33% showing significant carotid artery disease, and 15% had undergone previous carotid artery stenting. Twenty-four percent of patients had concomitant lower limbs arterial disease, and 30% of patients had undergone previous percutaneous coronary intervention or coronary artery bypass graft surgery.
| Variable | All (n=54) | Bilateral (n=35) | Ipsilateral (n=19) | P |
|---|---|---|---|---|
| Age (years) | 65 ± 9 | 66 ± 9 | 64 9 | 0.63 |
| Men | 32 (59%) | 18 (51%) | 14 (74%) | 0.15 |
| Height (cm) | 168 ± 11 | 167 ± 11 | 170 ± 11 | 0.35 |
| Weight (kg) | 73 ± 11 | 71 ± 10 | 77 ± 13 | 0.092 |
| Hypertension | 44 (81%) | 29 (83%) | 15 (79%) | 0.73 |
| Dyslipidemia | 30 (56%) | 18 (51%) | 12 (63%) | 0.57 |
| Diabetes Mellitus | 18 (33%) | 11 (31%) | 7 (37%) | 0.77 |
| Current smoker | 32 (59%) | 20 (57%) | 12 (63%) | 0.78 |
| Previous stroke | 10 (19%) | 6 (17%) | 4 (21%) | 0.73 |
| Previous carotid artery stenting | 8 (15%) | 3 (8.6%) | 5 (26%) | 0.11 |
| Lower limbs artery disease | 13 (24%) | 10 (29%) | 3 (16%) | 0.34 |
| Previous percutaneous coronary intervention | 13 (24%) | 8 (23%) | 5 (26%) | 1.00 |
| Previous coronary artery bypass graft surgery | 3 (5.6%) | 2 (5.7%) | 1 (5.3%) | 1.00 |
| Symptomatic | 40 (74%) | 29 (83%) | 11 (58%) | 0.058 |
Patients in bilateral group were more often symptomatic (83% vs 58%, p = 0.058), and there were significantly more CTOs in the bilateral group (77% vs 21%, p = 0.0001) than in the single group. In both groups, subclavian artery lesions were more often located in the left side (72%). The large majority of lesions were stented, except 5.7% in the bilateral group and 16% in the single group (p = 0.47). Although the number and mean diameter of stents were similar in both groups (1.06 ± 0.42 vs 0.95 ± 0.52, p = 0.44) and 7 (7 to 8) versus 7 (7 to 7), p = 0.13, respectively, the mean stented length was longer in the bilateral group 29 (15 to 39) versus 15 (15 to 18) mm, p = 0.027. Reflecting more complex procedures, procedure duration, total amount of contrast, and fluoroscopy time were greater in the bilateral group than in the single group (all p values <0.0001; Table 2 ). It should be noted that in 9.3% and 11% of the cases, patients underwent concomitant percutaneous coronary intervention or carotid artery stenting, respectively, during the same setting, without differences between the 2 groups. In all but 2 cases, procedures were completed by radial-only approach except 2 in the bilateral group, where crossover was required after failed attempt to cross subclavian artery CTO. Overall, procedural success was 97% in the bilateral group compared with 95% in the single group (p = 1.00). After intervention, blood pressure in both arms equalized in all patients with successful procedures except 2 in the bilateral group. After 5-year follow-up, 91% of stents in the bilateral group remain patent by duplex ultrasonography compared with 95% in the single group (p = 1.00; Tables 3 and 4 ; Figure 2 ).
| Variable | All (n=54) | Bilateral (n=35) | Ipsilateral (n=19) | P |
|---|---|---|---|---|
| Chronic total occlusion | 31 (57%) | 27 (77%) | 4 (21%) | 0.0001 |
| Number of stents | 1.02 ± 0.46 | 1.06 ± 0.42 | 0.95 ± 0.52 | 0.44 |
| Bridge X3 stent | 20 (37%) | 12 (34%) | 8 (42%) | 0.77 |
| Omnilink Elite stent | 21 (39%) | 16 (46%) | 5 (26%) | 0.24 |
| Rx Herculink Elite stent | 3 (5.6%) | 0 (0%) | 3 (16%) | 0.039 |
| Xpert stent | 3 (5.6%) | 3 (8.6%) | 0 (0%) | 0.54 |
| Dynamic stent | 2 (3.7%) | 2 (5.7%) | 0 (0%) | 0.54 |
| Balloon dilatation w/o stent | 3 (5.6%) | 1 (2.9%) | 2 (11%) | 0.28 |
| Direct stenting | 14 (26%) | 6 (17%) | 8 (42%) | 0.058 |
| Stent diameter (mm) | 7 [7-8] | 7 [7-8] | 7 [7-7] | 0.13 |
| Stent length (mm) | 18 [15-29] | 29 [15-39] | 15 [15-18] | 0.027 |
| Left subclavian | 39 (72%) | 25 (71%) | 14 (74%) | 1.00 |
| Right subclavian | 15 (28%) | 10 (29%) | 5 (26%) | 1.00 |
| Fluoroscopy time (minutes) | 14 [8-24] | 20 [12-30] | 8 [4-11] | <0.0001 |
| Total amount of contrast (milliter) | 200 [150-300] | 200 [200-350] | 150 [100-200] | <0.0001 |
| Procedure duration (minutes) | 35 [20-50] | 40 [35-60] | 20 [15-30] | <0.0001 |
| Procedure success | 52 (96%) | 34 (97%) | 18 (95%) | 1.00 |
| Simultaneous percutaneous coronary intervention | 5 (9.3%) | 2 (5.7%) | 3 (16%) | 0.33 |
| Simultaneous carotid artery stenting | 6 (11%) | 2 (5.7%) | 4 (21%) | 0.17 |
| Transradial access success | 52 (96%) | 33 (94%) | 19 (100%) | 0.54 |
| Variable | All (n=54) | Bilateral (n=35) | Ipsilateral (n=19) | P |
|---|---|---|---|---|
| 30-day follow-up | ||||
| Death | 0 | 0 | 0 | – |
| Myocardial infarction | 0 | 0 | 0 | – |
| Stroke | 0 | 0 | 0 | – |
| Target vessel revascularization | 0 | 0 | 0 | – |
| Long-term follow-up | ||||
| Follow-up (days) | 610 [345-985] | 610 [445-975] | 550 [198-1709] | 0.59 |
| MACCE | 4 (7%) | 1 (3%) | 3 (16%) | 0.12 |
| Death | 1 (2%) | 0 | 1 (5%) | 0.35 |
| Myocardial infarction | 1 (2%) | 0 | 1 (5%) | 0.35 |
| Stroke | 2 (4%) | 0 | 2 (11%) | 0.12 |
| Target vessel revascularization | 1 (2%) | 1 (3%) | 0 | 1.00 |
| Variable | All (n=54) | Bilateral (n=35) | Ipsilateral (n=19) | P |
|---|---|---|---|---|
| Blood pressure equalized | 50 (93%) | 32 (91%) | 18 (95%) | 1.00 |
| Patent stent on follow-up | 50 (93%) | 32 (91%) | 18 (95%) | 1.00 |
| Peak systolic velocity (cm/sec) | 81 ± 6 | 80 ± 6 | 82 ± 6 | 0.22 |
| Diameter (millimeter) | 7.7 ± 0.8 | 7.8 ± 0.7 | 7.4 ± 0.8 | 0.11 |




