This study reports the midterm results and experience of a single center of transcatheter closure of perimembranous ventricular septal defect (VSD) with Amplatzer membranous VSD occluders. Data of 301 patients who underwent attempted transcatheter closure were collected prospectively from May 2002 to December 2008. Patients’ mean age was 9.8 years, and their mean weight was 32 kg. The procedure was successful in 294 patients (97.6%). No death occurred. Complications included aortic regurgitation in 11 patients (3.7%, 2 requiring occluder retrieving), tricuspid regurgitation in 16 patients (5.4%), hemolysis in 2 patients (0.7%), and complete atrioventricular block (cAVB) in 17 patients (15 early cAVBs, 3 late cAVBs, 1 patient had early and late cAVBs). Among the 15 early cAVBs, 12 were transient and 3 were considered prolonged cAVBs (persisted >2 weeks). The 3 patients underwent surgery (1.0%) and obtained stable sinus rhythm. Pacemaker implantation was needed in all 3 patients with late cAVB (1.0%). Univariate analysis showed that risk factors were age (p = 0.01) and weight (p = 0.021). No risk factors were found in multivariate analysis. In conclusion, midterm results of transcatheter closure of perimembranous VSD showed high closure rate and limited complications. The major concern is the occurrence of cAVB. Long-term investigation is needed to assess the efficacy and safety compared to surgery.
Transcatheter closure of perimembranous ventricular septal defect (VSD) has been demonstrated as an alternative to surgery since 1987. Because it is less traumatic and has good cosmetic effect, it is welcomed by patients and their families. After the introduction of the specifically designed Amplatzer membranous VSD occluder, transcatheter closure has become a routine procedure with high closure rate, low mortality, and acceptable complication rates. In the current era, occurrence of complete atrioventricular block (cAVB) is the major concern in this procedure and in some cases requires pacemaker implantation. However, the mechanism underlying cAVB occurrence and the therapeutic policies are undefined. These problems need further evaluation in a large series of patients. This study describes our experience with the Amplatzer membranous VSD occluders in 301 patients, focusing on cAVB.
Methods
Data of patients who underwent transcatheter closure of a perimembranous VSD were collected from May 2002 to December 2008. General characteristics are presented in Table 1 . Inclusion criteria of patients were (1) weight ≥8 kg, (2) isolated defects between the 9 and 11 o’clock positions of an analog clock in short-axis view, (3) maximum diameter ≤16 mm by transthoracic echocardiography (TTE), (4) left to right shunt, and (5) pulmonary pressure <70 mm Hg by TTE. Exclusion criteria were (1) severe aortic regurgitation, (2) aortic valve prolapse, (3) contraindication to antiplatelet therapy, (4) sepsis, (5) subaortic rim <1 mm separating the aortic valve from the perimembranous VSD, and (6) cardiac function class IV. Of patients eligible for closure, 5 patients had postoperative residual VSDs and 62 patients had aneurysmal VSDs.
| Men | 155 |
| Women | 146 |
| Age (years), median (range) | 9.8 (1.2–50) |
| Age groups (years) | |
| <3 | 25 (8.3%) |
| 3–10 | 129 (42.9%) |
| 10–15 | 110 (36.5%) |
| >15 | 37 (12.3%) |
| Weight (kg), median (range) | 32 (8–80) |
| Fluoroscopic time (minutes) | 9.3 ± 3.2 |
| Procedure time (minutes) | 35 ± 8 |
| Systolic pulmonary artery pressure (mm Hg) | 25 ± 5 |
| Mean pulmonary artery pressure (mm Hg) | 14 ± 3 |
| Defect size by transthoracic echocardiography (mm) | 8.0 ± 2.5 |
| Device size (mm) | 9.3 ± 2.4 |
| Device used | 294 |
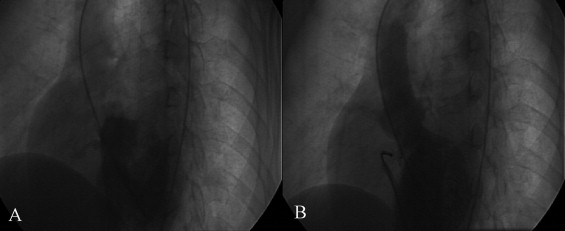
Devices used in this study were Amplatzer membranous VSD occluders designed by AGA Medical Corporation (Golden Valley, Minnesota). The devices and their delivery systems have been previously described. Transcatheter closure of a VSD was performed under general anesthesia for patients <10 years old and under local anesthesia for patients ≥10 years old. The procedure was performed with fluoroscopic and transthoracic echocardiographic guidance. Routine right- and left-sided cardiac catheterization was performed ( Figure 1 ). The device was to be 1 to 2 mm larger than the VSD diameter measured by TTE. Successful closure was defined by device implantation in the correct position with no significant complications (such as significant valve regurgitation) or significant residual shunt that required surgery. Aspirin was prescribed 3 to 5 mg/kg/day for 6 months after the procedure. All patients underwent electrocardiographic monitoring for 5 days and TTE before discharge, at 1 month and 3, 6, and 12 months during follow-up, and every 12 months thereafter. Patients with cAVB and other arrhythmias soon after the procedure were monitored by Holter monitor for 2 weeks.
Data were expressed as frequency or percentage for nominal variables and as mean ± SD for continuous variables. SPSS 11.0 (SPSS, Inc., Chicago, Illinois) was used for computation. cAVB was analyzed as a dependent variable. Independent variables in the analysis included age (<3 or ≥3 years), weight (<12 or ≥12 kg), repeated maneuver of catheter and/or sheath across the defect (<3 or ≥3), and device diameter. Univariate analysis was performed using chi-square test and Fisher’s exact test. Multivariate analysis was performed using Cox proportional hazard regression analysis.
Results
Procedure data and device used are presented in Table 1 . In all 301 patients with inclusion criteria, 294 had successful closure (97.6%). VSDs in 7 patients failed to close ( Table 2 ). Reasons for the 7 failures included cAVB in 2 patients (1 during repeated maneuver of catheter, 1 after release of occluder), significant aortic regurgitation in 2 patients (subaortic rim <1 mm by ventriculography, the device impinged on the aortic valve), and instable position of the device in 3 patients (the septum could not provide enough support to the occluder). The procedure was stopped in these patients and occluders were retrieved. All underwent uneventful surgical VSD closure.
| Patient Number | Age (years)/Sex | Weight (kg) | Defect Size (mm) | Device Size (mm) | Problem |
|---|---|---|---|---|---|
| 1 | 1.2/M | 10 | 8 | 9 | Complete atrioventricular block |
| 2 | 1.8/F | 11 | 11 | 12 | Aortic valve regurgitation |
| 3 | 2.4/M | 12 | 8 | 10 | Complete atrioventricular block |
| 4 | 3.1/M | 13 | 14 | 15 | Instable position of device |
| 5 | 7.5/F | 20 | 8 | 10 | Instable position of device |
| 6 | 11/M | 29 | 10 | 12 | Instable position of device |
| 7 | 13/M | 34 | 13 | 15 | Aortic valve regurgitation |
During the procedure, there were no deaths, device embolization, or pericardial tamponade. In total 58 early complications were observed (19.3%), and 33 of these required management (10.9%).
Aortic regurgitation occurred in 11 patients (3.7%). In 2 patients regurgitation occurred during the procedure and the procedures were aborted. The other 9 patients (3.0%) had trivial regurgitation and no treatment was needed. No aggravation was found during follow-up. Tricuspid regurgitation occurred in 16 patients (5.4%) and was defined as small (regurgitation volume <5 ml). No rupture of chordae tendineae was observed by TTE. No treatment was needed in these patients. During follow-up, tricuspid regurgitation disappeared in 10 patients and showed a decrease in regurgitation volume in 6 patients (regurgitation volume <2 ml).
Transient left bundle branch block occurred in 11 patients (3.7%). They were treated with steroids. Preoperative right bundle branch block remained unchanged after the procedure. No significant new right bundle branch block occurred. cAVB occurred in 2 patients during the procedure and in 15 patients (5.1%) 1 week after the procedure; of these 15 patients, 3 were <3 years old, 6 were 3 to 10 years old, 5 were 10 to 15 years old, and 1 was >15 years old. They were treated with steroids and isoprenaline (Harvest Pharmaceutical Co. Ltd., Shanghai, China), and 12 of them recovered in 2 weeks. The other 3 patients with no improvement underwent surgery to remove the devices and repair the defects ( Table 3 ). All 3 patients recovered sinus rhythm the day after surgery.



